Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):518-526
09-01-2018
To assess the relationship between the use of psychoactive substances during pregnancy and the occurrence of severe maternal morbidity (SMM), perinatal outcomes and repercussions on the neuropsychomotor development of exposed children.
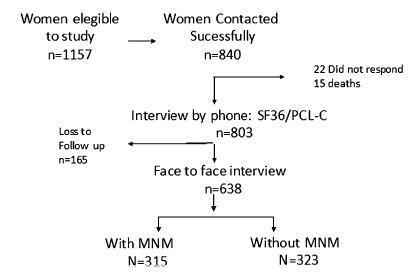
A case-control study nested within a cohort of severe maternal morbidity (COMMAG) was performed. Women with SMM were considered cases. Controls were thosewith low-risk pregnancy,without SMMand admitted during the same time period as the cases. Cohort data were collected retrospectively in hospital records for childbirth. A face-to-face interview was also performed with 638 women (323 without SMM and 315 with SMM) and their children of the index pregnancy between 6 months and 5 years after childbirth. During the interview, substance abuse during pregnancy was assessed by a modified question from the Alcohol, Smoking and Substance Involvement Screening Test 2.0 (ASSIST) and the neuropsychomotor development in the children was assessed by the Denver Developmental Screening Test, 2nd edition.
The prevalence of licit or illicit drug use during pregnancy was ~ 17%. Among drug users, 63.9% used alcohol, 58.3% used tobacco, 9.2% used cocaine/crack and 4.6% used marijuana. There was no association between drug use during pregnancy and SMM, although tobacco use during pregnancy was associated with bleeding, presence of near-miss clinical criteria (NMCC) and alteration in infant development; alcohol use was associated with neonatal asphyxia; and cocaine/crack use was associated with the occurrence of some clinical complications during pregnancy.
The use of psychoactive substances during pregnancy is frequent and associated with worse maternal, perinatal and child development outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(4):155-161
04-01-2017
To evaluate whether the presence of maternal blood pressure reduces the risks of morbidity, perinatal mortality and morbidity at 24 months of age in very low birth weight infants (VLBWIs) compared with a control group.
A retrospective, observational, case-control study. Total 49 VLBWIs were allocated to the study group, called the maternal arterial hypertension group (AHG), and matched with 44 in the control group (CG). The infants were assessed during hospitalization and at 12 and 24 months corrected age at a specialized clinic. For the assessment of growth, the World Health Organization (WHO) Anthro software (Geneva, 2006) was used, and for the psychomotor assessment, the Denver II test was used.
In relation to the antenatal variables, the infants of the AHG had more centralized circulation assessed by Doppler, received more corticosteroids and magnesium sulfate, and were born by cesarean section more frequently. In terms of the postnatal and in-hospital outcomes, the AHG had a higher gestational age at birth (30.7 versus 29.6 weeks) and a lower frequency of 5-minute Apgar scores of less than 7 (26.5% versus 52.3%). The CG had a higher rate of pulmonary dysplasia (30.2% versus 8.3%). There were no differences in terms of hospital mortality, complications, somatic growth and functional problems at 24 months of corrected age.
The presence of maternal hypertension, especially preeclampsia, was not a protective factor against morbidity, mortality and evolution in VLBWIs aged up to 24 months. Therefore, the clinical practice should be focused on prolonging the pregnancy for as long as possible in these conditions as well.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(6):274-280
08-02-2013
DOI 10.1590/S0100-72032013000600007
PURPOSE: To analyze the perinatal and pediatric outcome of fetuses that showed nuchal translucency (NT) above the 95th percentile (P95) and a normal karyotype in order to obtain data allowing better maternal prenatal counseling. METHODS: fetuses from a tertiary obstetric service with an NT above P95 and a normal karyotype were analyzed between 2005 and 2011. We analyzed gestational ultrasound follow-up, fetal and postnatal echocardiography (ECHO), weight, length and Apgar score at birth, and neuropsychomotor development by the Ages and Stages Questionnaire (ASQ) up to July 2012. RESULTS: During this period, there were 116 cases of nuchal translucency above the 95th percentile, and the fetal karyotype was determined in 79 of them (68%). Forty-three analyses were normal (54.4%) and 36 were altered (45.6%). Among the fetuses with a normal karyotype, one was miscarried at 15 weeks of gestation with Cantrel pentalogy and one died at 24 weeks with several structural abnormalities. There was one neonatal death of unknown cause and two cases of intraventricular communication (IVC) detected by fetal ECHO. Postnatal echocardiography revealed the persistence of IVC in one case and one case of atrial septal defect (ASD) and patent ductus arteriosus (PDA). Of the 40 surviving children, only 1 showed delayed speech development and another presented autism. The remaining cases resulted in normal neurodevelopment. CONCLUSION: During the monitoring of fetuses with increased NT and a normal karyotype, parents can be best advised that when a 2nd trimester morphological-echocardiography ultrasound study is normal, the probability of the child being born alive and well is high (93.5%).