-
Review Article
Short cervix and use of cervical pessary for preventing preterm birth in singleton and twin pregnancies: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo10
03-18-2025
Summary
Review ArticleShort cervix and use of cervical pessary for preventing preterm birth in singleton and twin pregnancies: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo10
03-18-2025Views94See moreAbstract
Objective:
Preterm birth remains a significant contributor to neonatal morbidity and mortality. The use of cervical pessaries as an intervention for preventing preterm delivery in women with a short cervix has been a subject of interest. We evaluated the effectiveness of cervical pessary compared to standard care in preventing preterm delivery in women with a short cervix.
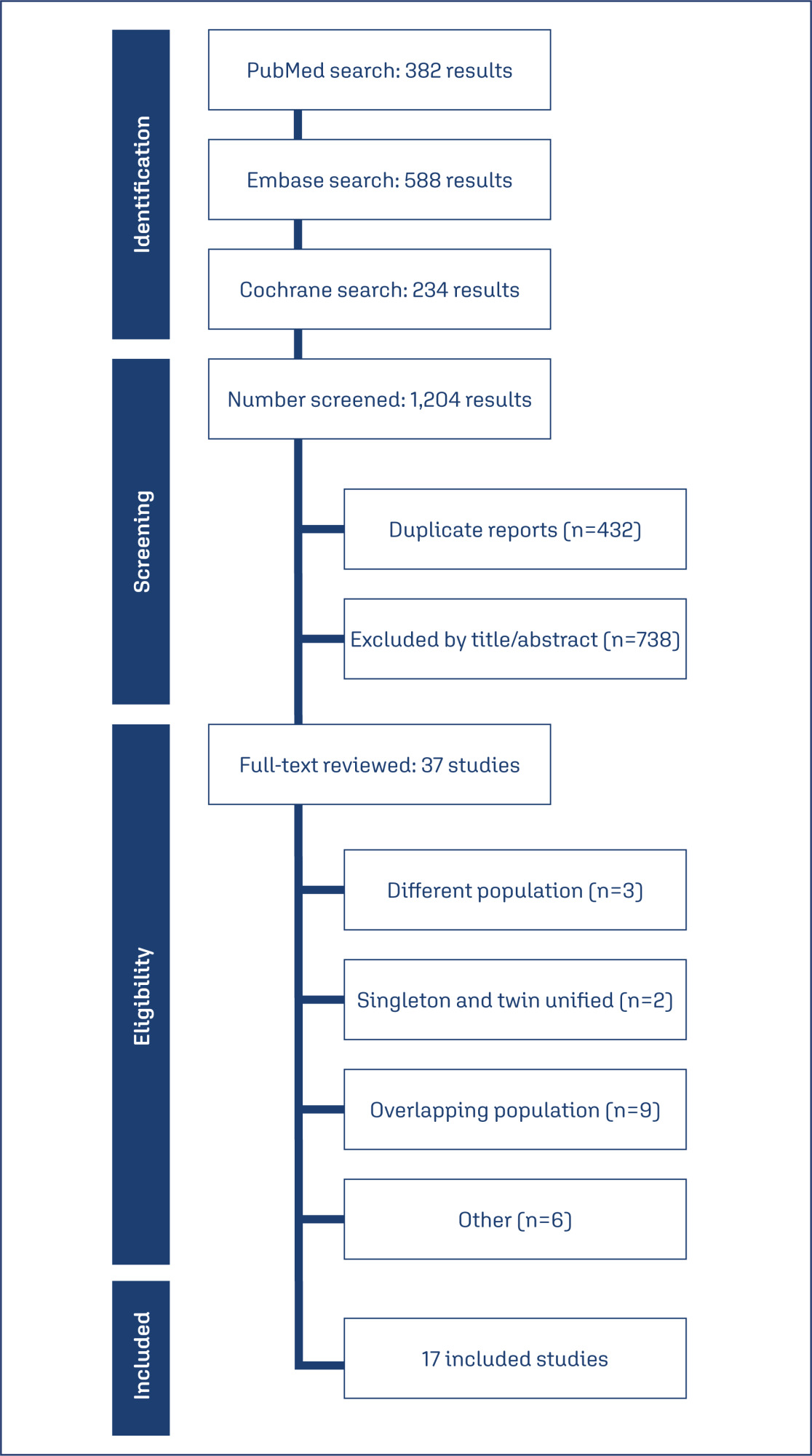
Data source:
Databases were systematically searched in PubMed, Cochrane, and Embase databases in December 2023.
Study selection:
Randomized clinical trials with the outcomes of interest were included.
Data collect:
We computed risk ratios for binary endpoints, with 95% confidence intervals. Heterogeneity was assessed using I2 statistics. Data were analyzed using R software (version 4.3.0). The primary outcomes of interest were preterm delivery before 37 weeks, and preterm delivery before 34 weeks.
Data synthesis:
Seventeen studies with 5,704 patients were included. The use of cervical pessary was associated with a decreased risk of preterm delivery before 37 (RR 0.88; 95% CI 0.81-0.96) and 34 weeks (RR 0.79; 95% CI 0.63-0.99) of gestation in twin pregnancies as compared to standard care without progesterone. There were no significant differences in preterm delivery in singleton pregnancy, neonatal outcomes, preterm premature rupture of the membranes or chorioamnionitis.
Conclusion:
The use of cervical pessary was associated with a significant reduction in preterm delivery at 34 and 37 weeks of gestation in twin pregnancies among patients with a short cervix compared to no treatment. No significant difference was found in singleton pregnancies or maternal outcomes.
-
Original Article
Screening and prevention of preterm birth: how is it done in clinical practice?
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo32
04-09-2024
Summary
Original ArticleScreening and prevention of preterm birth: how is it done in clinical practice?
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo32
04-09-2024Views457Abstract
Objective:
To ascertain how screening for preterm birth is performed among obstetricians working in public and private practice in a middle-income country.
Methods:
Cross-sectional study of 265 obstetrician-gynecologists employed at public and private facilities. An online questionnaire was administered, with items designed to collect data on prematurity screening and prevention practices.
Results:
The mean age of respondents was 44.5 years; 78.5% were female, and 97.7% had completed a medical residency program. Universal screening (i.e., by ultrasound measurement of cervical length) was carried out by only 11.3% of respondents in public practice; 43% request transvaginal ultrasound if the manual exam is abnormal, and 74.6% request it in pregnant women with risk factors for preterm birth. Conversely, 60.7% of respondents in private practice performed universal screening. This difference in screening practices between public and private practice was highly significant (p < 0.001). Nearly all respondents (90.6%) reported prescribing vaginal progesterone for short cervix.
Conclusion:
In the setting of this study, universal ultrasound screening to prevent preterm birth was used by just over half of doctors in private practice. In public facilities, screening was even less common. Use of vaginal progesterone in cervical shortening was highly prevalent. There is an unmet need for formal protocols for screening and prevention of preterm birth in middle-income settings.
Key-words attitudes, practiceCervical length measurementgynecologistshealth knowledgeInfant, prematureobstetriciansPreterm birthPreventionScreeningsurveys and questionnairesSee more -
Original Article
Women’s Obstetric History and Midtrimester Cervical Length Measurements by 2D/3D and Doppler Ultrasound
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(9):540-546
10-23-2020
Summary
Original ArticleWomen’s Obstetric History and Midtrimester Cervical Length Measurements by 2D/3D and Doppler Ultrasound
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(9):540-546
10-23-2020Views151Abstract
Objective
The aim of the present study was to compare the obstetric history and both two- and tri-dimensional ultrasound parameters according to different cervical lengths.
Methods
The present cross-sectional study analyzed 248 midtrimester pregnant women according to cervical length and compared the data with the obstetric history and 2D/3D ultrasound parameters. Patients were divided into 3 groups according to cervical length: The Short Cervix group for cervical lengths ≥ 15mm and< 25mm(n= 68), the Very Short Cervix group for cervical lengths< 15mm (n = 18) and the Control group, composed of 162 pregnant women with uterine cervical lengths ≥ 25mm.
Results
When analyzing the obstetric history of only non-nulliparous patients, a significant association between the presence of a short cervix in the current pregnancy and at least one previous preterm birth was reported (p = 0.021). Cervical length and volume were positively correlated (Pearson coefficient = 0.587, p < 0.0001). The flow index (FI) parameter of cervical vascularization was significantly different between the Control and Very Short Cervix groups. However, after linear regression, in the presence of volume information, we found no association between the groups and FI. Uterine artery Doppler was also not related to cervical shortening.
Conclusion
The present study showed a significant association between the presence of a short cervix in the current pregnancy and at least one previous preterm birth. None of the vascularization indexes correlate with cervical length as an independent parameter. Uterine artery Doppler findings do not correlate with cervical length.
Key-words Cervical length measurementCervix uteriPregnancy trimester, secondPregnancy, high riskreproductive historySee more -
Original Articles
Risk Assessment for Preterm Delivery using the Fetal Fibronectin Test Associated with the Measurement of Uterine Cervix Length in Symptomatic Pregnant Women
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):507-512
09-01-2018
Summary
Original ArticlesRisk Assessment for Preterm Delivery using the Fetal Fibronectin Test Associated with the Measurement of Uterine Cervix Length in Symptomatic Pregnant Women
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):507-512
09-01-2018Views97See moreAbstract
Objective
To analyze the use of the measurement of uterine cervix length (MUCL) and the fetal fibronectin (fFN) rapid test as predictors of preterm delivery (PTD) in symptomatic pregnant women assisted at the Santa Casa de Misericórdia de Sobral Maternity Hospital.
Methods
This was a prospective and analytic study involving 53 parturients assisted between September of 2015 and July of 2016; the participants were between 24 and 34 weeks of gestational age (GA) and presented complaints related to preterm labor (PTL) prodromes. Vaginal secretion was collected for fFN testing, and the MUCL was obtained via transvaginal ultrasonography.
Results
A total of 58.49% of the subjects showed MUCL < 25 mm, and 41.51% were positive in the fFNrapid test.Atotal of 48 patients were followed-up until their delivery date, and 54.17% resulted in PTL. The relative risk (RR) for PTD in patients with MUCL < 25 mm was 1.83 (p = 0.09, 0.99-3.36, 95% confidence interval [CI]), with a mean time before delivery of 2.98 weeks. Based on fFN positive results, the RR was 3.50 (p = 0.002, 1.39- 8.79, 95%CI) and themean time until delivery was 1.94weeks. The RRwas 2.70 (p = 0.002, 1.08-6.72, 95%CI) when both tests were used. The RR of PTD within 48 hours, and 7 and 14 days were, respectively, 1.30 (p = 0.11, 95% CI 1.02-1.67), 1.43 (p = 0.12, 95% CI % 0.99-2.06), and 2.03 (p = 0.008, 95% CI 1.26-3.27), when based on the MUCL, and 1.75 (p = 0.0006, 95% CI 1.20-2.53), 2.88 (p = 0.0001, 95% CI, 1.57-5.31), and 3.57 (p = 0.0002, 95% CI 1.63-7.81) when based on positive fFN results. The RR at 48 hours and 7 and 14 days considering both tests was 1.74 (p = 0.0001, 95% CI 1.14-2.64), 2.22 (p = 0.0001, 95% CI 1.22-4.04), and 2.76 (p = 0.0002, 95% CI 1.27-5.96), respectively.
Conclusion
In symptomatic pregnant women, we concluded that the MUCL < 25 mm associated with positive fFN rapid test indicate increased the risk for PTD. Further studies with larger sample sizes could contribute in supporting the results presented in the current study.
-
Artigos Originais
Preterm birth prediction: sequential evaluation of the cervix and the test for phosphorylated protein-1 linked to insulin-like growth factor
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(9):394-400
11-06-2013
Summary
Artigos OriginaisPreterm birth prediction: sequential evaluation of the cervix and the test for phosphorylated protein-1 linked to insulin-like growth factor
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(9):394-400
11-06-2013DOI 10.1590/S0100-72032013000900003
Views49PURPOSE: To investigate the usefulness of the measurement of cervical length and of the test for phosphorylated insulin-like growth factor binding protein-1 (phIGFBP-1) performed sequentially in the prediction of preterm birth and the correlation between tests. METHODS: We analyzed data from 101 asymptomatic pregnant women with a history of premature delivery. The ultrasound measurement of cervical length and phIGFBP-1 test were performed in parallel every three weeks, between 24 and 34 week. The best cutoff value for each cervical evaluation was established by the ROC curve, and the two tests were compared using nonparametric tests. We determined the sensitivity, specificity and predictive values of each test and of the association of the exams for the occurrence of delivery before the 37th weeks. RESULTS: There were 25 preterm births (24.8%). The cervix length showed the highest sensitivity and was able to predict preterm birth in all evaluations, with similar accuracy at different gestational ages. The test for phIGFBP-1 was not helpful at 24 weeks, but was able to predict prematurity when performed at 27, 30 and 33 weeks. The combination of tests increased the sensitivity (81.8%) and negative predictive value (93.7%) when compared to the separate use of each test. The mean cervical length was lower in women with a positive test. CONCLUSIONS: Both cervical length and the test for phIGFBP-1 were able to predict premature delivery, and sequential combination of both tests showed a high sensitivity and high negative predictive value.
Key-words Biological markersCervical length measurementCervixInsulin-like growth factor binding protein-1Premature birthRisk assessmentSee more -
Trabalhos Originais
Longitudinal Assessment of Cervix Length in Twin Gestation
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(6):377-381
09-23-2002
Summary
Trabalhos OriginaisLongitudinal Assessment of Cervix Length in Twin Gestation
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(6):377-381
09-23-2002DOI 10.1590/S0100-72032002000600004
Views55See morePurpose: to establish a reference range for cervical length measurement throughout gestation in twin pregnancies and to correlate cervical length with gestational age at delivery. Methods: retrospective analysis of prospectively collected data between 1994 and 2000, involving 149 twin pregnancies undergoing transvaginal ultrasound examination every four weeks for measurement of cervical length. Results: one hundred and twenty-seven women (85.2%) delivered after 34 weeks, 20 (13.4%) between 24 and 33 weeks and two pregnancies resulted in fetal loss before 24 weeks. The mean gestational age at delivery was 36.3 weeks. A total of 497 ultrasound examinations with cervical length measurement were performed in 127 patients with twin pregnancies who delivered after 34 weeks (mean = 4 examinations per patient). All scans were carried out between 9 and 39 weeks (mean = 29.4 weeks). There was an inverse correlation between cervical length measurement and gestational age at the scan in twin pregnancies (r=-0.44; p < 0.0001). The mean value was 44 mm at 10 weeks and 28 mm at 36 weeks. The corresponding fifth percentile values of these gestations were 28 mm and 12 mm, respectively. Cervical length measurement changes were more pronounced in the second half of the pregnancy (Kruskal-Wallis test, p=0.0006). Mean cervical length measurement and 90% prediction interval values were established throughout gestation by regression analysis. Twenty-six cases delivered before 34 weeks, nine of these cases (34.6%) had at least one cervical length measurement below the 5th percentile. Conclusions: cervical length shortens gradually throughout gestation in twin pregnancies but changes are more significant in the second half of the pregnancy. Approximately one-third of the pregnancies that delivered before 34 weeks had at least one cervical length measurement below the 5th percentile for the gestational age.


