Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(8):431-437
DOI 10.1590/S0100-72031999000800002
Purpose: to evaluate risk factors and papillomavirus (HPV) associated lesions in male partners of women with genital intraepithelial neoplasia. Patients and Methods: three hundred and thirty-seven men were evaluated by urethral cytology, peniscopy, and biopsy, if necessary. We analyzed the results and the relations to age, educational level, smoking, contact time with the present partner, age at first intercourse, number of partners, previous sexually transmitted diseases (STD), circumcision, peniscopic findings, and female lesion grade. Results: peniscopy was positive in 144 (42,7%) and HPV infection was diagnosed in 105 (31,2%). Smoking, contact time with the present partner up to 6 months, and more than one previous sexual partner were associated with HPV lesions (p<0,05). The urethral cytology was suspect in 4,2% and smoking, positive peniscopy or biopsy and partners of women with high-grade lesion (p<0,05) were associated with the diagnosis. 72.1% of 229 biopsies were positive, independently of the peniscopic findings and women's lesion grade. Conclusions: HPV infection was diagnosed in 31.2% and was associated with smoking, contact time with the present partner up to 6 months and more than one previous sexual partner, but not with the female lesion grade, educationa level, previous STD, circumcision and peniscopic findings.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):619-626
DOI 10.1590/S0100-72032005001000009
PURPOSE: to evaluate the prevalence of cytologic, colposcopic and histopathologic alterations observed in the uterine cervix of adolescents with suspected cervical neoplasia and to compare it with young adult women. METHODS: a cross-sectional, retrospective study that analyzed 366 medical records of females referred to clarify diagnosis of the suspected cervical neoplasia. The patients had been classified into two groups defined by age. The Adolescent group was composed of 129 females between 13 and 19 years and the Adult group was composed of 237 females between 20 and 24 years. Data were analyzed statistically by the prevalence ratio (PR), respective confidence intervals (CI) at 95% for each variable, chi2 test, or Fisher exact test used to compare proportion. RESULTS: the first sexual intercourse coitarche occurred on average at 15.0 years in the Adolescent group and 16.6 years in the Adult group. The possibility of diagnosis of cytological alterations in the first Papanicolaou smears (PR=2.61; CI 95%: 2.0-3,4), the condition of non-clarified cervical intraepithelial neoplasia (CIN) (PR=1.78; CI 95%: 1.26-2,52), and the colposcopic impressions of low grade (PR=1.42; CI 95%: 1.08-1.86) were statistically significant in the Adolescent group. The histopathologic analysis did not show differences at any grade of CIN. However, two cases of microinvasive carcinoma, one in each group, and three cases of clinical invasive carcinoma in the Adult group were identified. CONCLUSION: our study suggests that cervical cancer is rare among adolescents, but we verified that alterations associated with it occurred even in younger women. The evaluation of cervical intraepithelial neoplasia with the careful application of the same tools used for adult women was appropriate also in adolescence.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(2):65-70
DOI 10.1590/S0100-72032000000200002
Purpose: to evaluate conization by the loop electrosurgical excision procedure (LEEP) for the diagnosis and treatment of cervical intraepithelial neoplasms (CIN), the importance of the margins and follow-up of these women. Methods: 95 women who underwent conization by LEEP for CIN and microinvasive carcinoma from January 1996 to December 1997 were evaluated. For statistical analysis, we used the kappa agreement coefficient and the tendency test of Cochran Armitage. Results: among 63 cases who underwent colposcopically directed biopsy before the conization, the cone presented the same grade of lesion in 20 and no residual disease in 8. The cone lesion presented a higher grade in 24 cases and one of them was a microinvasive carcinoma. Among the 25 women who underwent the cone biopsy with a previous biopsy suggestive of cervicitis or CIN 1, 56% had CIN 2 or 3 in the cone. Among the 32 women without previous biopsy, 15 had CIN 2 or 3, and four had microinvasive carcinoma in the cone. Regarding the margins of the cone, 25 cases presented some grade of CIN in the endocervical margins and 2/10 who underwent a second procedure presented residual disease on histological analysis. Among the 70 women with free cone margins, 2/4 who underwent a second procedure had residual disease on histological analysis. Conclusion: conization by LEEP without previous directed biopsy depends on the experience of the colposcopist. The second resection after LEEP for the diagnosis and treatment of CIN depends not only on the presence of disease in the cone margins but also on the follow-up. A second histological analysis is recommended in cases with microinvasive carcinoma and glandular lesion and affected margins.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(9):721-725
DOI 10.1590/S0100-72032004000900008
PURPOSE: to analyze the association between bacterial vaginosis (BV), high-risk HPV DNA, and Pap smear abnormalities in women submitted to diathermic conization for the treatment of high-grade cervical intraepithelial neoplasia (CIN 2 or 3). METHODS: a descriptive clinical study with 81 women submitted to diathermic conization for the treatment of CIN 2 or 3. Initial Pap smear was performed by the time of the biopsy and was also used to verify the presence of BV. Prior to conization, samples for the detection of high-risk HPV DNA through hybrid capture II (HC II) were collected. A control visit was scheduled for four months after the conization to repeat these tests. Twenty-seven women were found to have BV and 54 were not. Statistical analysis comprised odds ratios (OR) to assess the correlations between BV and HPV detection before and after diathermic conization and cytological abnormalities. All analyses were performed with a 95% confidence interval (95% CI). RESULTS: high-risk HPV DNA detection before conization was identical in both groups (89%). After conization, HPV DNA detection decreased to 26 and 18% in the groups with and without BV, respectively (OR=1.5; 95% CI 0.5 to 4.6). In addition, 41% of the women with BV and 20% without BV showed Pap smear abnormalities (OR=2.7; 95% CI 1.0 to 7.4). Regarding these 22 women with Pap smear abnormalities approximately four months after the diathermic conization, 83% of the BV group tested positive for HPV DNA compared with 50% in the group without BV (OR=5.0; IC 95% 0.5 a 52.9). CONCLUSION: women with BV presented more Pap smear abnormalities after conization when compared to the women without BV, although this was not statistically significant. This association was not related to high-risk HPV DNA.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(3):213-219
DOI 10.1590/S0100-72032004000300007
OBJECTIVE: to evaluate the effectiveness of the hygroscopic dilator in the colposcopic examination of the endocervical canal in patients with high-grade lesion in the cytopathology and unsatisfactory colposcopy. METHODS: prospective study, including 62 patients with unsatisfactory colposcopic examination and cytology compatible with high-grade intraepithelial lesion. The patients were submitted to dilation of the endocervical canal by means of a hygroscopic dilator. After dilation, the new colposcopic findings were recorded, and then conization was made through loop electrosurgical excision procedure. The incidence of neoplasic involvement of surgical margins was compared between patients with examinations modified toward satisfactory results and those that remained with unsatisfactory colposcopy. In order to compare the incidence of involved margins and the incidence of residual disease, two retrospective control-groups were used: the GinSat group (n = 35): patients with unsatisfactory colposcopy; GSat group (n = 38): patients with satisfactory colposcopy and endocervical atypy. RESULTS: 80.6% of the cases presented satisfactory colposcopic vision after dilation. 80.4% of those presented disease-free resection margins. The incidence of disease-free resection margins in patients with persistent unsatisfactory colposcopy after dilation was 36.3%. Affected surgical margins occurred in 28% of the group that had undergone dilation, 28.5% of the cases in GinSat group, and 31.5% in the Gsat group. Follow-up showed the incidence of residual disease in 7.5% of the patients under dilation, 28.5% in the GinSat group and 28.9% in the GSat group. CONCLUSION: the use of hygroscopic dilation improved visualization of lesions of difficult access to the colposcopic examination, thus permitting reduction in the percentage of residual neoplasic disease in patients with unsatisfactory colposcopy treated with loop electrosurgical excision procedure.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(2):97-102
DOI 10.1590/S0100-72032004000200003
PURPOSE: to correlate the type of cervical lesion diagnosed by Pap smear with CD4 cell counts and HIV-RNA viral load in HIV-positive patients. METHODS: one hundred and fifteen HIV patients were evaluated retrospectively in the present study, during the period from January 2002 to April 2003, at a university hospital. Eighty-three patients presented cervical intraepithelial neoplasia (CIN) in Pap smear, in comparison with thirty-two with no lesions. Patients were divided into three groups, according to CD4 counts: CD4 more than 500 cells/mm³, between 200 and 500 cells/mm³, and less than 200 cells/mm³, and other three groups, according to HIV viral load: less than 10,000 HIV-RNA copies/mL, between 10,000 and 100,000 HIV-RNA copies/mL, or more than 100,000 HIV-RNA copies/mL. Correlation was investigated by the Fisher test. RESULTS: of the eighty-three patients with CIN, 73% presented CD4 counts less than 500 cells/mm³. In all CD4 groups, more than 50% of the patients presented CIN. According to the viral load, 71.7% of the patients with less than 10,000 HIV-RNA copies/mL presented CIN I, compared with 11.3% that showed CIN III. In the group with higher viral load (>100.000 HIV-RNA copies/mL), 61.5% showed CIN I and 30.8% presented CIN III. CONCLUSION: association between viral load and CIN was established (p=0.013), which was not observed with CD4 cell counts and CIN. Concomitant cervicovaginal infection was considered a potential confounding factor.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(6):339-345
DOI 10.1590/S0100-72032000000600004
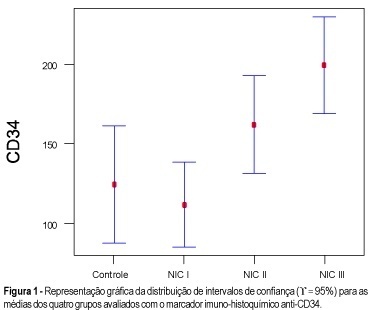
Purpose: to quantify the vessels and epithelial proliferation, applying immunohistochemical staining with anti-CD34 as well as anti-PCNA markers, in intra-epithelial neoplasia of the uterine cervix. Methods: in the present study, 16 patients with CIN III, 16 with CIN II, 21 with CIN I and 11 with normal cervix (control group) were investigated. Slide analysis was performed at the same time by two observers, in 10 consecutive sites using 100X and 400X magnification, both in the highest vascularization (CD34) and proliferative activity sites (PCNA). Results: the means obtained with the use of anti-PCNA in intraepithelial neoplasias were: 78.2% (CIN III), 52.1% (CIN II), 33.3% (CIN I) and 4.6% (control group), while 199.1 vessels (CIN III), 162.0 vessels (CIN II), 111.7 vessels (CIN I) and 124.4 vessels (control group) were quantified using anti-CD34 as a vascular marker. Conclusion: the results showed that both markers, anti-PCNA and anti-CD34, are useful for investigating proliferative and angiogenic activity, respectively. However, anti-PCNA showed better and more accurate results than anti-CD34 in differentiating intraepithelial neoplasias.