-
Original Article
Preventing Uterine Cervix Cancer: The Clinical Meaning of Atypical Glandular Cells
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):483-488
02-09-2022
Summary
Original ArticlePreventing Uterine Cervix Cancer: The Clinical Meaning of Atypical Glandular Cells
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):483-488
02-09-2022Views206Abstract
Objective
To determine the prevalence of the atypical glandular cells (AGCs) cytology and to analyze its clinical significance in different age ranges.
Methods
Retrospective observational study using computerized data from the Brazilian National Cancer Institute, including women screened between January 2002 and December 2008. The women included were those with an AGC result who were properly followed-up with colposcopy and a second cytology.
Results
A total of 132,147 cytopathological exams were performed during the study period. Five-hundred and thirty-three (0.4%) women with AGC cytology were identified and, of these, 69.41% (370/533) were properly referred for colposcopy and a new cytology. Most of the women (79.2%) with a 1st or 2nd AGC cytology were between the ages of 25 and 54 years. The 2nd cytology demonstrated 67.6% (250/370) of normality, 24.5% (91/370) of squamous atypia, and 6.2% (23/370) of AGC, 0.8% (3/370) adenocarcinoma in situ and 0.8% (3/370) adenocarcinoma invasor. On biopsy of the women with a second AGC cytology, 43.4% (10/23) had normal histology, 43.4% (10/23) had squamous lesions, 8.7% (2/23) had invasive adenocarcinoma, and 1.2% (1/23) had an inconclusive report. All of the women with high-grade squamous intraepithelial lesion (HSIL) or invasive adenocarcinoma (respectively 5 and 2 patients), after a 2nd AGC cytology were 25 years old or older.
Conclusion
The prevalence of the AGC cytology was low in the studied population. Most of the AGC cytology cases occurred in adult women between the ages of 25 and 54. Although most of the patients had normal histology after follow-up, several of them presented with squamous intraepithelial lesions or invasive adenocarcinoma.
Key-words AGCatypical glandular cellsBethesda systemcervical cancer screeningCytologyglandular cervical neoplasiaSee more -
Original Article
Prevalence of Human Papillomavirus Infection and Cervical Cancer Screening among Riverside Women of the Brazilian Amazon
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):350-357
07-01-2017
Summary
Original ArticlePrevalence of Human Papillomavirus Infection and Cervical Cancer Screening among Riverside Women of the Brazilian Amazon
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):350-357
07-01-2017Views215Abstract
Purpose
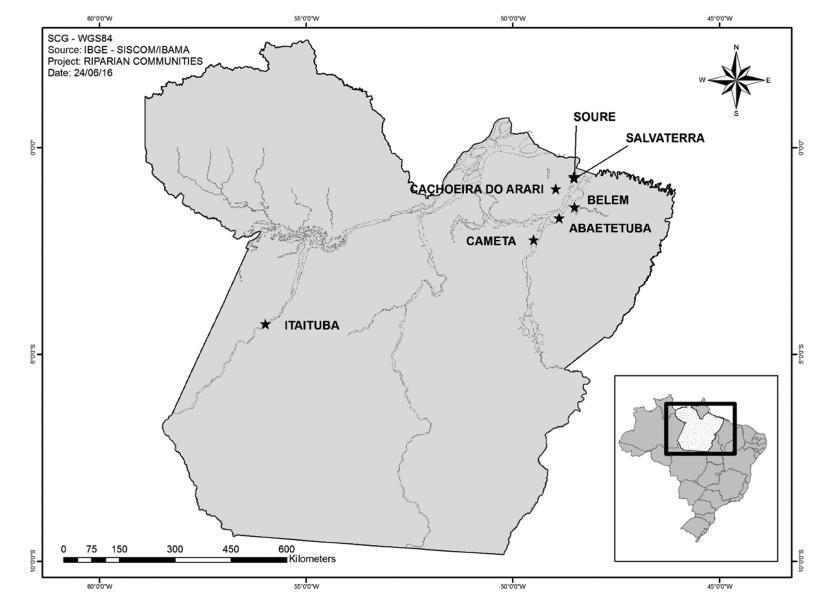
The aim of this study was to evaluate the overall and type-specific prevalence of human papillomavirus (HPV) infection among females living in riverside communities in the state of Pará, in the Eastern Brazilian Amazon. These communities are inhabited by low-income people, and are accessible only by small boats. Cervical cytology and risk factors for HPV infection were also assessed.
Methods
Cervical samples from 353 women of selected communities were collected both for Papanicolau (Pap) test and HPV detection. Conventional polymerase chain reaction (PCR) and real-time PCR were used to assess the overall and type-specific prevalence of HPV-16 and HPV-18, the main oncogenic types worldwide. Epidemiological questionnaires were used for the assessment of the risk factors for HPV infection.
Results
The mean age of the participants was 37 years (standard deviation [SD] ± 13.7). Most were married or with a fixed sexual partner (79%), and had a low educational level (80%) and family monthly income (< U$ 250; 53%). Overall, HPV prevalence was 16.4% (n = 58), with 8 cases of HPV-16 (2.3%) and 5 of HPV-18 (1.4%). Almost 70% of the women surveyed had never undergone the Pap test. Abnormal cytology results were found in 27.5% (n = 97) of the samples, with higher rates of HPV infection according to the severity of the lesions (p = 0.026).
Conclusions
The infections by HPV-16 and HPV-18 were not predominant in our study, despite the high prevalence of overall HPV infection. Nevertheless, the oncogenic potential of these types and the low coverage of the Pap test among women from riverside communities demonstrate a potential risk for the development of cervical lesions and their progression to cervical cancer, since the access to these communities is difficult and, in most cases, these women do not have access to primary care and public health services.
Key-words cervical cancer screeningEpidemiologyhuman papillomavirus 16human papillomavirus 18Sexually transmitted diseasesSee more