Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo90
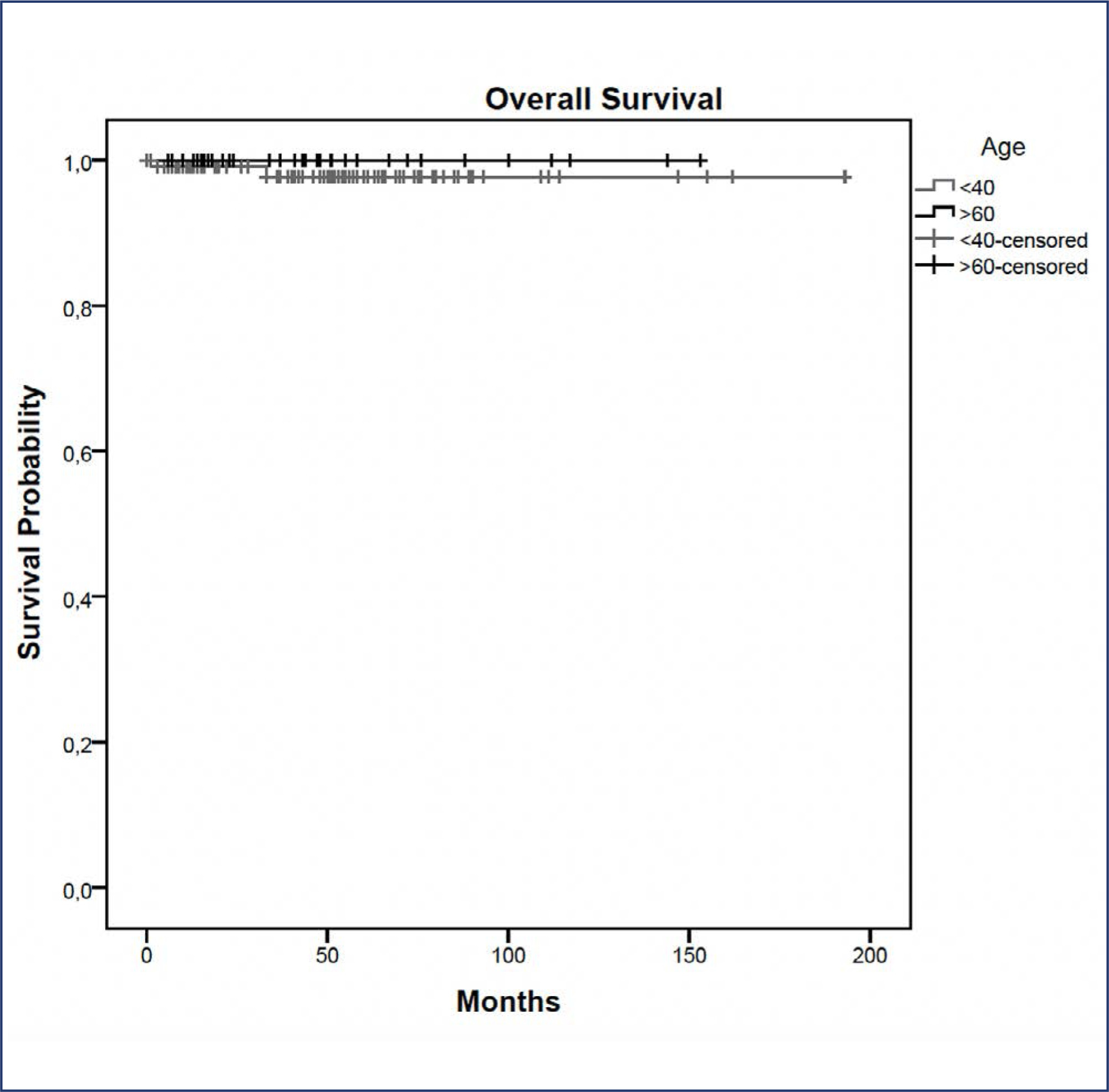
In this study, we compared indications and outcomes of 115 young (< 40 years) versus 40 elderly (> 60 years) patients undergoing nipple-sparing mastectomy (NSM) as risk-reducing surgery or for breast cancer (BC) treatment.
Between January 2004 and December 2018, young and elderly patients undergoing NSM with complete data from at least 6 months of follow-up were included.
BC treatment was the main indication for NSM, observed in 85(73.9%) young versus 33(82.5%) elderly patients, followed by risk-reducing surgery in 30(26.1%) young versus 7(17.5%) elderly patients. Complication rates did not differ between the age groups. At a median follow-up of 43 months, the overall recurrence rate was higher in the younger cohort (p = 0.04). However, when stratified into local, locoregional, contralateral, and distant metastasis, no statistical difference was observed. During the follow-up, only 2(1.7%) young patients died.
Our findings elucidate a higher recurrence rate of breast cancer in younger patients undergoing NSM, which may correlate with the fact that age is an independent prognostic factor. High overall survival and low complication rates were evidenced in the two groups showing the safety of NSM for young and elderly patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo50
To determine the relationship between early age at menarche, late age at menopause with specific subtypes of breast cancer (BC).
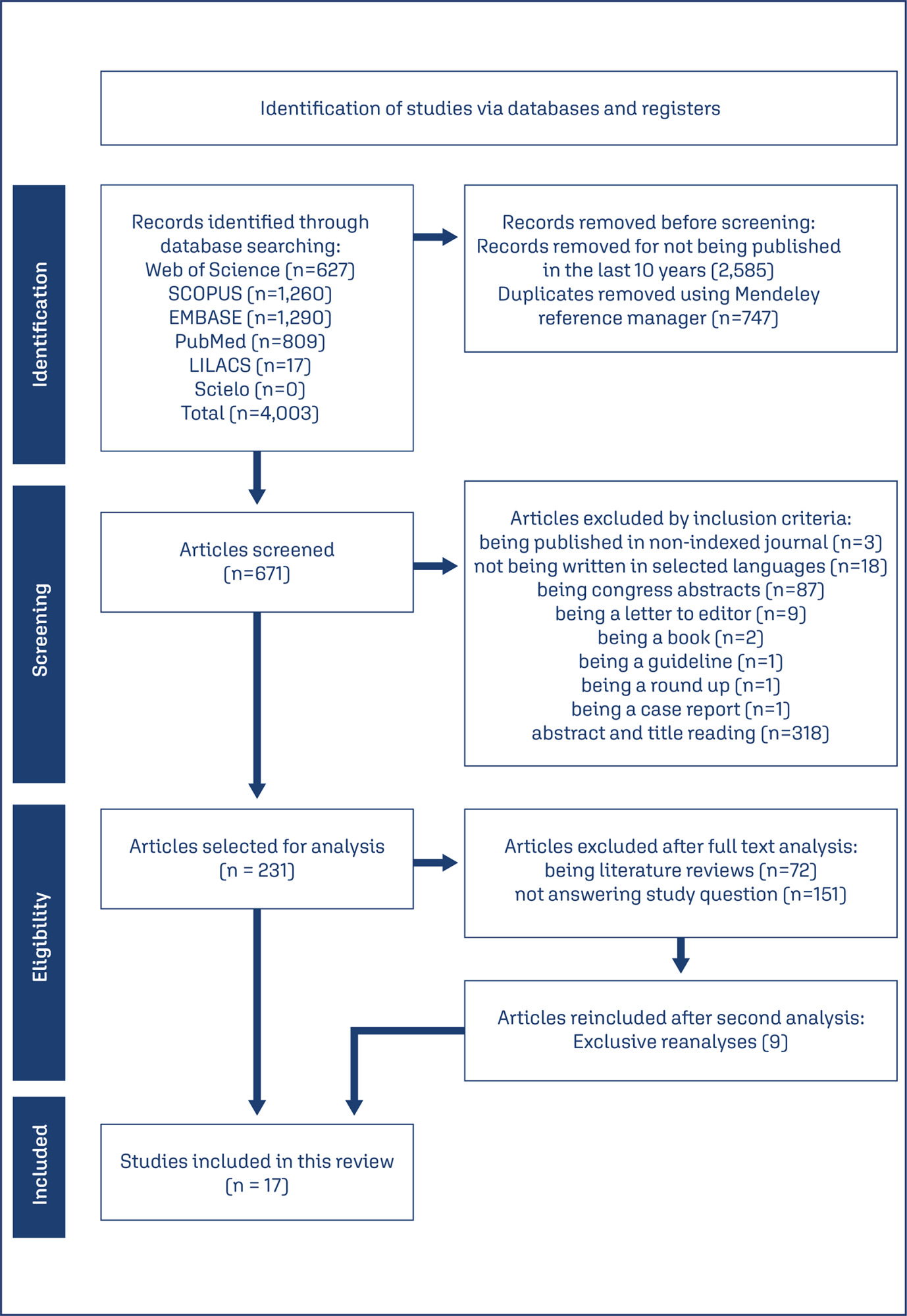
A literature search was conducted in Embase, Lilacs, PubMed, Scopus, and Scielo databases, following the Joanna Briggs Institute scoping review protocol and answering the question “How early age at menarche or late age at menopause are related to different breast cancer subtypes?”.
A number of 4,003 studies were identified, of which 17 were selected. Most of the included articles found a clear relationship between early menarche, late menopause and some subtypes of BC, mainly, PR+, ER+, luminal, and HER-2 tumors. However, some studies have found a contradictory relationship and one study didn’t find any relationship between them.
A relationship between early age at menarche and advanced age at menopause was observed with some subtypes of breast cancer, since other factors must be considered in its understanding.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo76
To evaluate early complications in prepectoral breast reconstruction.
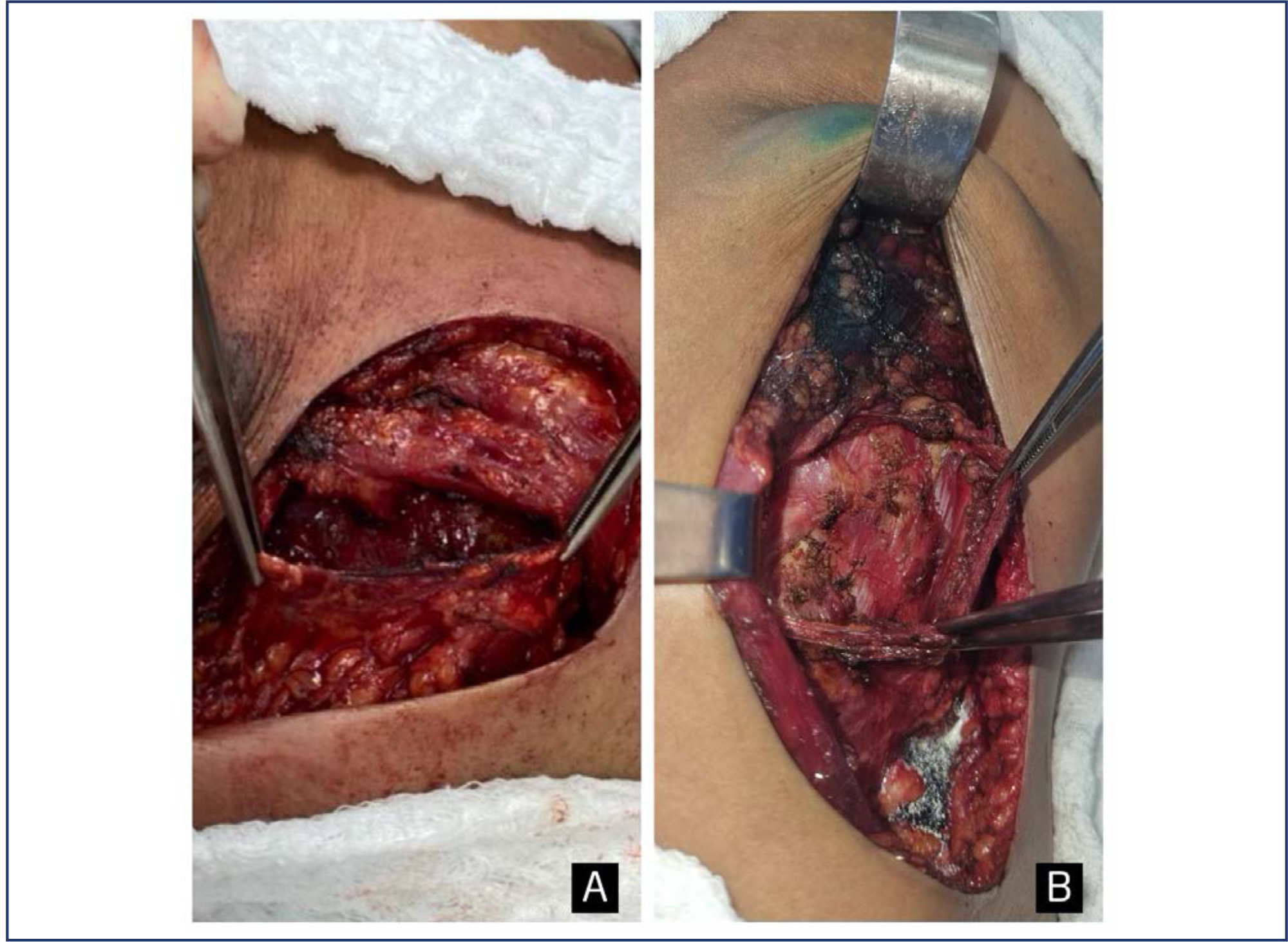
A retrospective cohort study including 180 consecutive cases of nipple-sparing mastectomy, comparing immediate breast reconstruction with subpectoral to prepectoral mammary implants in 2012-2022. Clinical and demographic characteristics and complications in the first three months following surgery were compared between the two techniques.
The prepectoral technique was used in 22 cases (12.2%) and the subpectoral in 158 (87.8%). Median age was higher in the prepectoral group (47 versus 43.8 years; p=0.038), as was body mass index (25.1 versus 23.8; p=0.002) and implant volume (447.5 versus 409 cc; p=0.001). The prepectoral technique was more associated with an inframammary fold (IMF) incision (19 cases, 86.4% versus 85, 53.8%) than with periareolar incisions (3 cases, 13.6% versus 73, 46.2%); (p=0.004). All cases in the prepectoral group underwent direct-to-implant reconstruction compared to 54 cases (34.2%) in the subpectoral group. Thirty-eight complications were recorded: 36 (22.8%) in the subpectoral group and 2 (9.1%) in the prepectoral group (p=0.24). Necrosis of the nipple-areola complex/skin flap occurred in 27 patients (17.1%) in the subpectoral group (prepectoral group: no cases; p=0.04). The groups were comparable regarding dehiscence, seroma, infection, and hematoma. Reconstruction failed in one case per group (p=0.230). In the multivariate analysis, IMF incision was associated with the prepectoral group (aOR: 34.72; 95%CI: 2.84-424.63).
The incidence of early complications was comparable between the two techniques and compatible with previous reports. The clinical and demographic characteristics differed between the techniques. Randomized clinical trials are required.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo71
To conduct a systematic review of external validation studies on the use of different Artificial Intelligence algorithms in breast cancer screening with mammography.
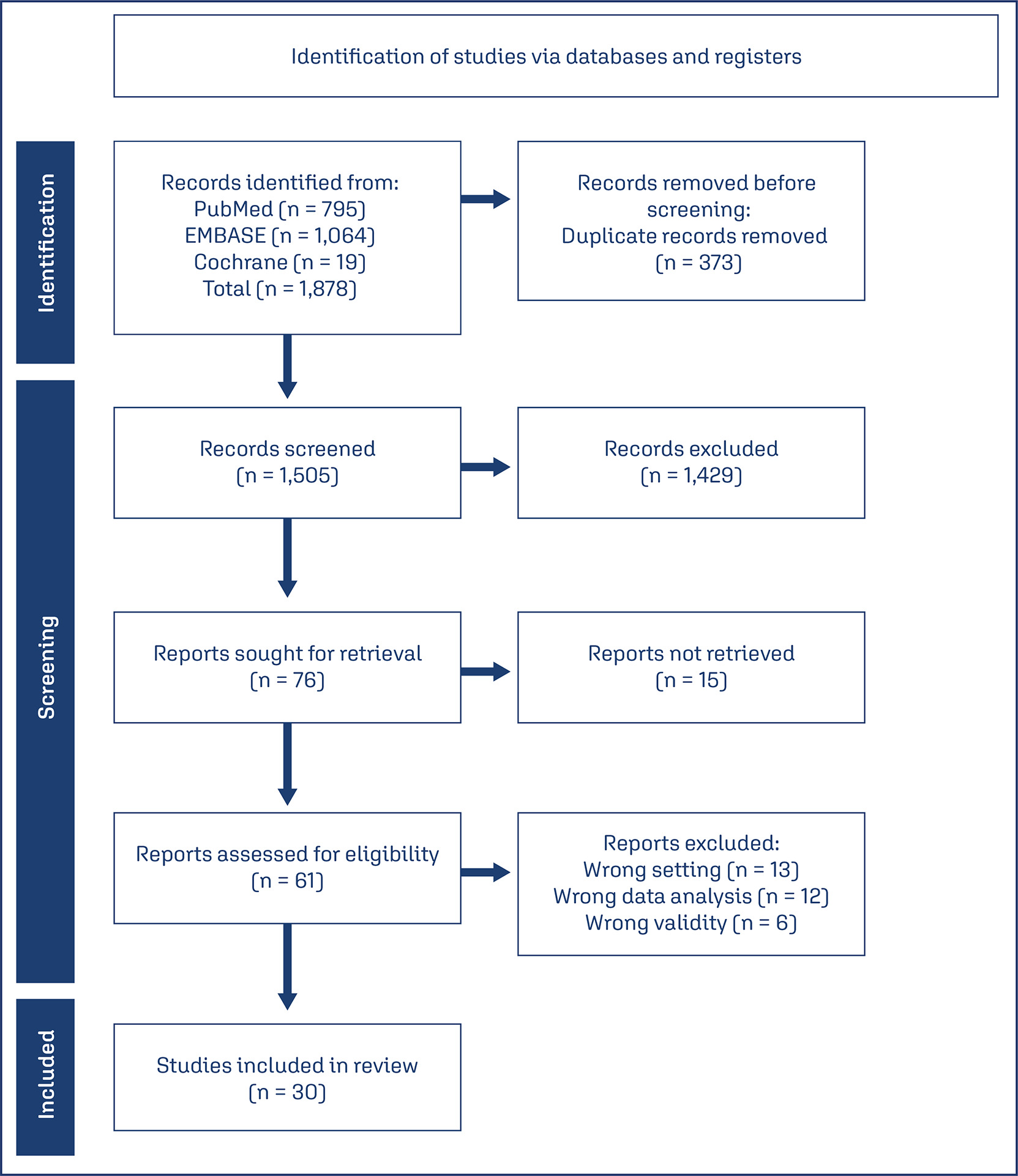
Our systematic review was conducted and reported following the PRISMA statement, using the PubMed, EMBASE, and Cochrane databases with the search terms “Artificial Intelligence,” “Mammography,” and their respective MeSH terms. We filtered publications from the past ten years (2014 – 2024) and in English.
A total of 1,878 articles were found in the databases used in the research. After removing duplicates (373) and excluding those that did not address our PICO question (1,475), 30 studies were included in this work.
The data from the studies were collected independently by five authors, and it was subsequently synthesized based on sample data, location, year, and their main results in terms of AUC, sensitivity, and specificity.
It was demonstrated that the Area Under the ROC Curve (AUC) and sensitivity were similar to those of radiologists when using independent Artificial Intelligence. When used in conjunction with radiologists, statistically higher accuracy in mammogram evaluation was reported compared to the assessment by radiologists alone.
AI algorithms have emerged as a means to complement and enhance the performance and accuracy of radiologists. They also assist less experienced professionals in detecting possible lesions. Furthermore, this tool can be used to complement and improve the analyses conducted by medical professionals.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo13
The purpose of this study was to compare postoperative pain between SF flap and serratus anterior muscle (SM) in direct-to-implant breast reconstruction.
This is a prospective cohort study that included 53 women diagnosed with breast cancer who underwent mastectomy and one-stage implant-based breast reconstruction from January 2020 to March 2021. Twenty-nine patients (54.7%) had SF elevation, and 24 patients (45.3%) underwent SM elevation. We evaluated patient-reported early postoperative pain on the first day after surgery. Also, it was reported that all surgical complications in the first month and patient reported outcomes (PROs) were measured with the BRECON 23 questionnaire.
The serratus fascia group used implants with larger volumes, 407.6 ± 98.9 cc (p < 0.01). There was no significant difference between the fascial and muscular groups regarding the postoperative pain score reported by the patients (2 versus 3; p = 0.30). Also, there was no difference between the groups regarding early surgical complications and PROs after breast reconstruction.
The use of SF seems to cause less morbidity, which makes the technique an alternative to be considered in breast reconstruction. Although there was no statistical difference in postoperative pain scores between the fascia and serratus muscle groups.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo15
To compare the medical image interpretation's time between the conventional and automated methods of breast ultrasound in patients with breast lesions. Secondarily, to evaluate the agreement between the two methods and interobservers.
This is a cross-sectional study with prospective data collection. The agreement's degrees were established in relation to the breast lesions's ultrasound descriptors. To determine the accuracy of each method, a biopsy of suspicious lesions was performed, considering the histopathological result as the diagnostic gold standard.
We evaluated 27 women. Conventional ultrasound used an average medical time of 10.77 minutes (± 2.55) greater than the average of 7.38 minutes (± 2.06) for automated ultrasound (p<0.001). The degrees of agreement between the methods ranged from 0.75 to 0.95 for researcher 1 and from 0.71 to 0.98 for researcher 2. Among the researchers, the degrees of agreement were between 0.63 and 1 for automated ultrasound and between 0.68 and 1 for conventional ultrasound. The area of the ROC curve for the conventional method was 0.67 (p=0.003) for researcher 1 and 0.72 (p<0.001) for researcher 2. The area of the ROC curve for the automated method was 0. 69 (p=0.001) for researcher 1 and 0.78 (p<0.001) for researcher 2.
We observed less time devoted by the physician to automated ultrasound compared to conventional ultrasound, maintaining accuracy. There was substantial or strong to perfect interobserver agreement and substantial or strong to almost perfect agreement between the methods.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo29
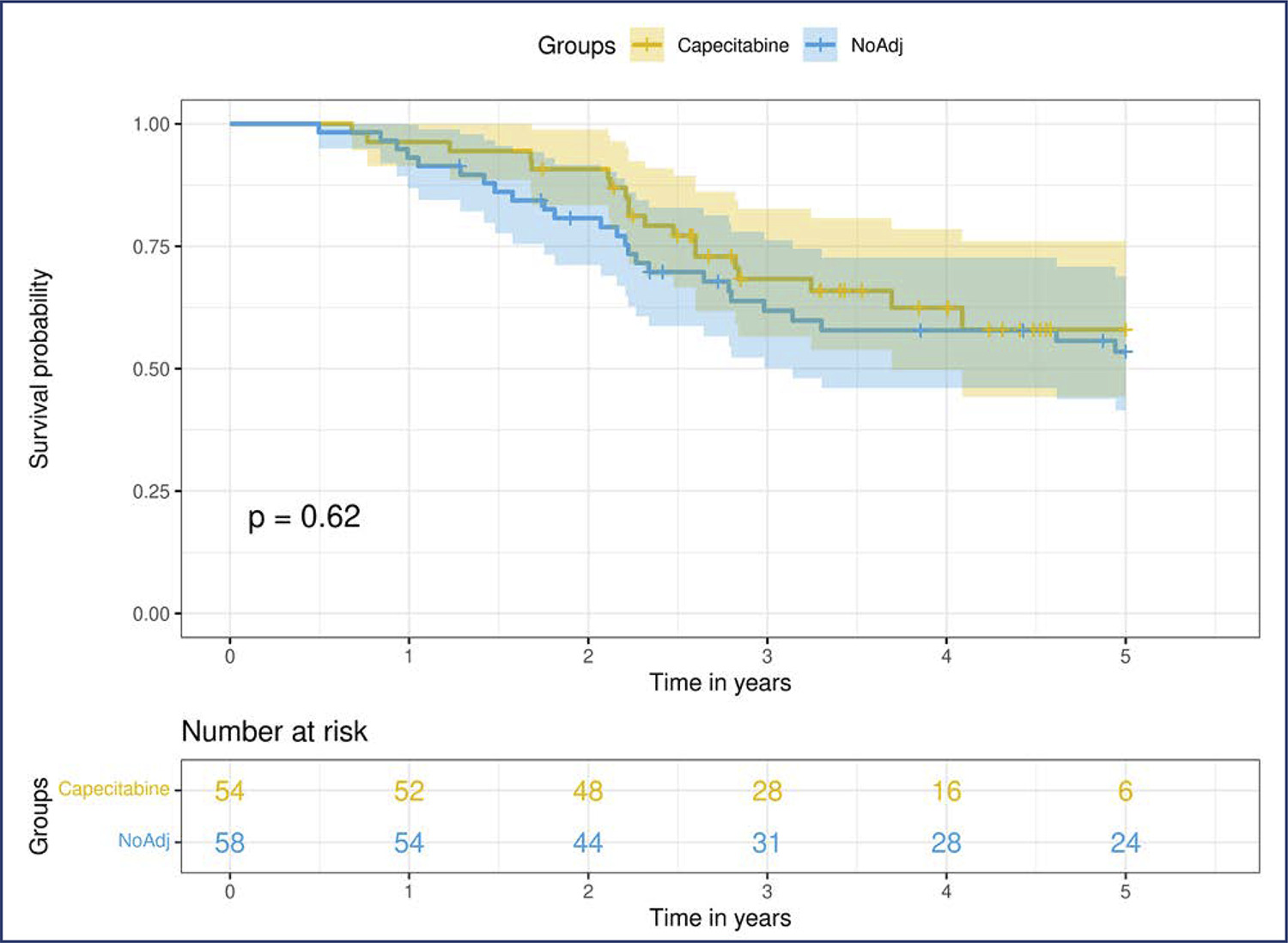
Neoadjuvant chemotherapy (NACT) has become the standard of care for patients with triple-negative breast cancer (TNBC) with tumors > 1 cm or positive axillary nodes. Pathologic complete response (pCR) has been used as an endpoint to select patients for treatment scaling. This study aimed to examine the benefit of adding adjuvant capecitabine for TNBC patients who did not achieve pCR after standard NACT in a real-world scenario.
This retrospective cohort study included all patients with TNBC who underwent NACT between 2010 and 2020. Clinicopathological data were obtained from the patient records. Univariate and multivariate analyses were conducted at the 5 years follow-up period.
We included 153 patients, more than half of whom had stage III (58.2%) and high-grade tumors (60.8%). The overall pCR rate was 34.6%, and 41% of the patients with residual disease received adjuvant capecitabine. Disease-specific survival (DSS) among the patients who achieved pCR was significantly higher (p<0.0001). Residual disease after NACT was associated with detrimental effects on DSS. In this cohort, we did not observe any survival benefit of adding adjuvant capecitabine for patients with TNBC subjected to NACT who did not achieve pCR (p=0.52).
Our study failed to demonstrate a survival benefit of extended capecitabine therapy in patients with TNBC with residual disease after NACT. More studies are warranted to better understand the indication of systemic treatment escalation in this scenario.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo55
Our study evaluated the effectiveness of the Botucatu Abbreviated Protocol in breast magnetic resonance imaging (MRI) within Brazil’s public healthcare system, focusing on its impact on patient access to MRI exams.
This retrospective study involved 197 breast MRI exams of female patients over 18 years with histological breast carcinoma diagnosis, conducted at Hospital das Clínicas de Botucatu - UNESP between 2014 and 2018. Two experienced examiners prospectively and blindly analyzed the exams using an Integrated Picture Archiving and Communication System (PACS). They first evaluated the Botucatu Abbreviated Protocol, created from sequences of the complete protocol (PC), and after an average interval of 30 days, they reassessed the same 197 exams with the complete protocol. Dynamic and morphological characteristics of lesions were assessed according to BI-RADS 5th edition criteria. The study also analyzed the average number of monthly exams before and after the implementation of Botucatu Abbreviated Protocol.
The Botucatu Abbreviated Protocol showed high sensitivity (99% and 96%) and specificity (90.9% and 96%). There was a significant increase in the average monthly MRI exams from 6.62 to 23.8 post-implementation.
The Botucatu Abbreviated Protocol proved effective in maintaining diagnostic accuracy and improving accessibility to breast MRI exams, particularly in the public healthcare setting.