Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(10):453-458
DOI 10.1590/S0100-72032012001000004
PURPOSES: To assess the quality of life of breast cancer survivors compared to a sample of age-matched healthy women. METHODS: A cross-sectional design was conducted on 199 consecutive breast cancer survivors, one year or more after diagnosis, treated at two large hospitals. The patients were compared to age-matched healthy women consisting of employees and volunteers of the two hospitals. Quality of life was evaluated using the World Health Organization Quality of Life Questionnaire, version Bref (WHOQOL-bref) and socioeconomic, clinical, and treatment data were obtained. The χ² test and a generalized linear model were used for statistical analysis. The adopted level of significance was 5%. RESULTS: The mean age of breast cancer survivors was 54.4 years (SD=10.4) and the average length of time since diagnosis was 5.0 years (SD=4.6). The survivors reported a poorer overall quality of life (p=0.001), and for the physical (p<0.001), psychological (p=0.002) and environment (p=0.029) domains than the comparison group, after adjusting for potential confounders. There was no significant difference in the social relationships domain (p=0.929) between groups. CONCLUSION: The results suggest that many breast cancer survivors experienced worse quality of life assessment than healthy women. This information may be useful to establish strategies to improve the quality of life of women with breast cancer.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(2):86-91
DOI 10.1590/S0100-72032012000200008
PURPOSE: To evaluate the actions of the "Um Beijo Pela Vida" Program developed in a Brazilian Northeast city to increase adherence to breast cancer screening by women registered by the Brazilian Family Health Strategy for breast cancer screening. METHODS: A quantitative approach was used to evaluate the coverage of screening actions for aged 40 years-old or more. Community workers from the nine Family Health Teams of the town carried out an active search. The percentage of eligible women who were screened for breast cancer by clinical breast examination or mammography, mammogram classification according to BI-RADS®, women screened who were referred for further testing and treatment, and the number of breast cancers detected were collected by means of a structured questionnaire, analyzed with the EPI-INFO TM software and compared to previously defined patterns. RESULTS: 3,608 women were included, corresponding to 68.4% of the target population registered in the Brazilian Family Health Strategy. Coverage rates of clinical breast examination for women aged 40 to 49 years-old and of mammograms for women aged 50 to 69 years-old were 58.9 and 56.7%, respectively. All women with highly suspicious mammographic lesions were submitted to fine needle aspiration or core biopsy (100%). Six new cases of cancer were detected and 80% of the standards established for this evaluation were carried out. CONCLUSIONS: The evaluation of the actions of the Program suggests its adequacy considering the degree of fulfillment of the previously defined requirements.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(7):123-131
DOI 10.1590/S0100-72032011000700002
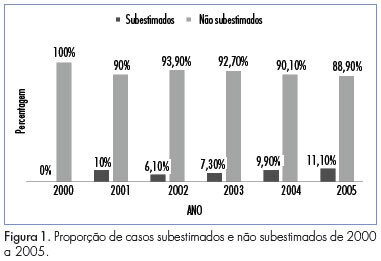
PURPOSE: To determine the rate of underestimation of an image-guided core biopsy of nonpalpable breast lesions, with validation by histologic examination after surgical excision. METHODS: We retrospectively reviewed 352 biopsies from patients who were submitted to surgery from February 2000 to December 2005, and whose histopathologic findings were recorded in the database system. Results were compared to surgical findings and underestimation rate was determined by dividing the number of lesions that proved to be carcinomas at surgical excision by the total number of lesions evaluated with excisional biopsy. Clinical, imaging, core biopsy and pathologic features were analyzed to identify factors that affect the rate of underestimation. The degree of agreement between the results was obtained by the percentage of agreement and Cohen's kappa coefficient. The association of variables with the underestimation of the diagnosis was determined by the chi-square, Fisher exact, ANOVA and Mann-Whitney U tests. The risk of underestimation was measured by the relative risk (RR) together with the respective 95% confidence intervals (95%CI). RESULTS: Inconclusive core biopsy findings occurred in 15.6% of cases. The histopathological result was benign in 26.4%, a high-risk lesion in 12.8% and malignant in 45.2%. There was agreement between core biopsy and surgery in 82.1% of cases (kappa=0.75). The false-negative rate was 5.4% and the lesion was completely removed in 3.4% of cases. The underestimation rate was 9.1% and was associated with BI-RADS® category 5 (p=0,01), microcalcifications (p CONCLUSIONS: The core breast biopsy under image guidance is a reliable procedure but the recommendation of surgical excision of high-risk lesions detected in the core biopsy remains since it was not possible to assess clinical, imaging, core biopsy and pathologic features that could predict underestimation and avoid excision. Representative samples are much more important than number of fragments.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(2):75-80
DOI 10.1590/S0100-72032011000200004
PURPOSE: to determine the prevalence of lymphedema and its associated factors in breast cancer patients. METHODS: Two hundred and fifty women that had undergone more than six months of breast cancer treatment and were being treated at an oncology reference hospital in Juiz de Fora, Minas Gerais, Brazil. They were interviewed and submitted to physical evaluation. Data from the patients' medical records regarding the treatment of breast cancer, the extent of axillary intervention and the tumor were analyzed. Lymphedema was diagnosed when the difference between both upper limbs was 2 cm or more by perimetry. The groups of women with and without lymphedema were compared regarding the possible risk factors, and central tendency, dispersion, and prevalence were measured, with a significance level of 95%. RESULTS: One hundred and twelve women (44.8%) presented lymphedema. A significant difference was found between the groups of women with and without lymphedema regarding the median numbers of removed lymph nodes (p=0.02); presentation of superficial lymphatic thrombosis in the arm ipsilateral to the surgery (p<0.01); local application of radiotherapy, use of chemotherapy (p<0.01 for both); removal of the cuticles of the ipsilateral hand with pliers, and weightlifting after the treatment (p<0.01 and p=0.05, respectively). CONCLUSIONS: the association between lymphedema and the mentioned factors requires an interdisciplinary approach to this condition. It is of paramount importance that health teams and patients become aware of the prevention and treatment of lymphedema, a condition often undervalued.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(1):27-30
DOI 10.1590/S0100-72032011000100004
PURPOSE: to evaluate the concordance rate of ultrasound-guided core needle biopsy followed by excisional biopsy in palpable breast lumps, suggestive of fibroepithelial tumors. METHOD: a retrospective study included 70 biopsies with a histological diagnosis of fibroepithelial tumor in 67 out of 531 patients with breast lesions submitted to ultrasound-guided core needle biopsy with a high frequency (7.5 MHz) linear transducer, using an automatic Bard-Magnum gun and a 14-gauge needle. Cases with a diagnosis of fibroepithelial tumor by core needle biopsy or excisional biopsy and with a diagnosis of fibrosclerosis were included in the study. The agreement between the two biopsy methods was assessed using the Kappa coefficient. RESULTS: excisional biopsy revealed 40 cases of fibroadenoma (57.1%), 19 cases of phyllodes tumor (27.2%), and 11 cases of fibrosclerosis (15.7%). The concordance rate for fibroadenoma was substantial (k = 0.68, 95%CI = 0.45 - 0.91), almost perfect for the phyllodes tumor (k = 0.81, 95%CI = 0.57 - 1.0), and moderate for fibrosclerosis (k = 0.58, 95%CI = 0.36 - 0.90). CONCLUSIONS: the core needle biopsy is a minimally invasive method that has "substantial" to "almost perfect" concordance rate with excisional biopsy. Fibrosclerosis should be considered in the differential diagnosis of fibroepithelial tumors.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(12):602-608
DOI 10.1590/S0100-72032010001200007
PURPOSE: to prospectively evaluate the effects of immediate breast reconstruction on the quality of life of women who underwent mastectomy. METHODS: 76 women that underwent mastectomy at Centro de Atenção Integral à Saúde da Mulher da Universidade Estadual de Campinas, in Campinas, São Paulo, Brazil, from August 2007 to December 2008, were included. Two groups were formed: 41 women who underwent mastectomy combined with immediate breast reconstruction (M+RI) and 35 that were subjected to mastectomy alone (M). The quality of life evaluation was assessed with the World Health Organization's questionnaire - Quality of Life (WHOQOL-100). The questionnaire was administered on three occasions: at the time of admission, one month after surgery, and again six months after surgery. The WHOQOL-100 scores were calculated according to analysis' guidelines by the World Health Organization. For comparison of the scores between groups, it was used the Student's t-test, Fisher exact test, chi-square test, and Mann-Whitney test. For the analysis of repeated measures over time, ANOVA and ANOVA for repeated measures were used. RESULTS: at all time points evaluated, beginning with the preoperative assessment, the average quality of life scores of the M+IR Group were higher than those of the M Group, primarily in the "physical", "psychological", "level of independence" and "social relationships" domains of the questionnaire. Of the six areas covered by the questionnaire, three ("physical", "social relations", "environment") showed no significant differences between groups. The M+IR Group had a better score (15.5 to 14.9 for the M+IR and 14.3 to 14.2 for M; p=0.04) in the psychological domain. There was a significant reduction in the level of independence in the first month after surgery in both groups, with a significant recovery after six months. CONCLUSIONS: the present results suggest that immediate breast reconstruction is significantly beneficial regarding the psychological aspects of quality of life, without affecting the patient's physical functionality.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(12):597-601
DOI 10.1590/S0100-72032010001200006
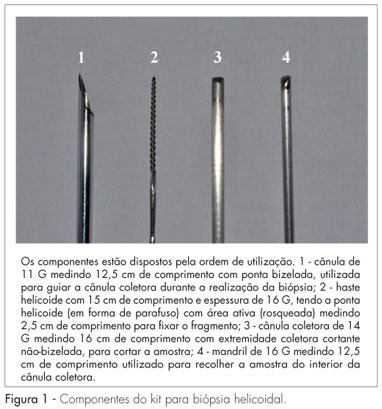
PURPOSE: to assess the helicoid biopsy performance when carrying out breast biopsies. METHODS: thirty patients with breast cancer submitted to mastectomy were selected at random. Women with a tumor of petreous consistency, nonpalpable, submitted to previous surgical manipulation or containing fluid were excluded. The helicoid biopsy kit and a core biopsy device with a cannula and a 14-gauge-needle, respectively, were used to collect a fragment each from a healthy area and from the tumor of each surgical specimen, for a total of 120 fragments for histological study. Data were analyzed statistically by the parametric Student's t-test and by the Kappa concordance index at the 95% confidence level, using the SPSS software, version 13. RESULTS: the mean patient's age was 51.6 (±11.1) years old. The core biopsy showed 93.3% sensitivity, 100% specificity and 96.7% accuracy, and the helicoid biopsy showed 96.7% sensitivity, 100% specificity, and 98.3% accuracy. The comparison of tumor histology and biopsy fragments revealed a high degree of concordance in the diagnoses (Kappa equal to 0.9, with p<0.05). CONCLUSIONS: both methods provided a highly accurate histological diagnosis of the lesions. The results of the present study demonstrate that the helicoid biopsy is a reliable alternative for the preoperative diagnosis of breast lesions.