Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(12):569-574
DOI 10.1590/S0100-72032013001200007
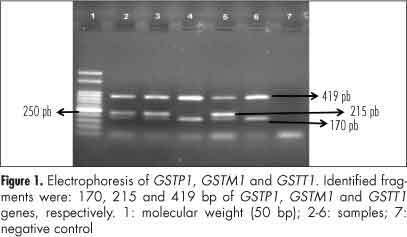
PURPOSE: This study aimed to evaluate the frequency of homozygous deletion of GSTM1 and GSTT1 genes and their combinations between patients with breast cancer and healthy individuals, associating them with disease susceptibility. METHODS: This is a case-control study in which 49 women diagnosed with breast cancer confirmed by pathological examination and 49 healthy women with no evidence of cancer and no prior family history of breast cancer were invited to participate. All of them answered a questionnaire with epidemiological data and were submitted to blood sample collection. Genomic DNA was extracted from blood, and genotyping was performed by polymerase chain reaction. Data were analyzed with SPSS 20.0. RESULTS: The frequency of null alleles for GSTM1 and GSTT1 was 58.8 and 61.7%, respectively, for patients with breast cancer, and 41.2 and 38.3%, respectively, in control patients. In homozygous deletion of the GSTM1 gene, a significantly higher frequency was found in the breast cancer cases. CONCLUSION: Breast cancer patients presented higher frequency of homozygous deletion of the GSTM1 gene compared with the control group.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(5):221-225
DOI 10.1590/S0100-72032013000500006
PURPOSE: We aimed to determine whether clinical examination could adequately ascertain the volume of tissue to be resected during breast-conserving surgery after neoadjuvant therapy. METHODS: We reviewed the clinical reports of 279 patients with histologically diagnosed invasive breast carcinomas treated with neoadjuvant therapy followed by surgery or with primary surgery alone. We estimated volumes of excised tissues, the volume of the tumor mass and the optimal volume required for excision based on 1 cm of clear margins. The actual excess of resected volume was estimated by calculating the resection ratio measured as the volume of the resected specimen divided by the optimal specimen volume. The study endpoints were to analyze the extent of tissue resection and to ascertain the effect of excess resected tissue on surgical margins in both groups of patients. RESULTS: The median tumor diameter was 2.0 and 1.5 cm in the surgery and neoadjuvant therapy groups, respectively. The median volume of resected mammary tissue was 64.3 cm³ in the primary surgery group and 90.7 cm³ in the neoadjuvant therapy group. The median resection ratios in the primary surgery and neoadjuvant therapy groups were 2.0 and 3.3, respectively (p<0.0001). Surgical margin data were similar in both groups. Comparison of the volume of resected mammary tissues with the tumor diameters showed a positive correlation in the primary surgery group and no correlation in the neoadjuvant therapy group. CONCLUSION: Surgeons tend to excise large volumes of tissue during breast-conserving surgery after neoadjuvant therapy, thereby resulting in a loss of the correlation between tumor diameter and volume of the excised specimen.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(5):215-220
DOI 10.1590/S0100-72032013000500005
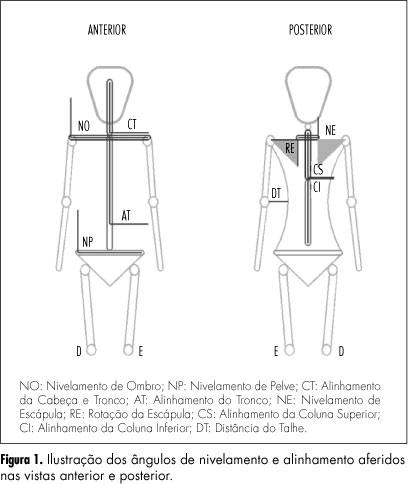
PURPOSE: To evaluate the body posture of women submitted to treatment for breast cancer, to identify the postural changes in the first three months after surgery and to investigate the correlation of these findings with the woman's age and type and side of surgery. METHODS: A longitudinal study that monitored the postural changes of 39 women who underwent mastectomy and quadrantectomy. Postural evaluation was performed using the technique of biophotogrammetry before surgery, after drain removal and three months after surgery. Statistical analysis was performed using parametric and nonparametric tests, with the level of significance set at p<0.05. RESULTS: The average age of the women studied was 50±10.5 years, 48.8% underwent mastectomy and the left breast was operated in 61.5% of them . There was no statistically significant difference in the women's posture during the study period. However, the pelvis and trunk of women submitted to quadrantectomy showed better alignment (90°) compared to the women submitted to mastectomy (91.3°). The women submitted to surgery in the left breast had shoulder elevation and ipsilateral inclination of the trunk within a short period of time. CONCLUSION: Postural changes were correlated with the type and side of surgery. The follow-up of this group after completion of treatment is needed to clarify long-term postural changes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(4):171-177
DOI 10.1590/S0100-72032013000400007
PURPOSE: To evaluate changes in the venous axillary-subclavian and lymphatic systems of women with lymphedema after axillary lymphadenectomy for breast cancer treatment. METHODS: This was a case series involving 11 women with unilateral upper limb lymphedema after axillary lymphedenectomy for the treatment of breast cancer. The study was carried out in the Mastology Program of the Clinical Hospital of the Federal University of Goiás, Goiânia, GO, during the period between March 2010 and March 2011. Doppler velocimetry ultrasonography was used to detect the presence of venous changes in the subclavian and axillary veins. Lymphatic changes were evaluated by lymphoscintigraphy in both upper limbs. Fisher's exact test was used for the comparison between limbs. RESULTS: Subclavian vein flow volume in the upper limb with lymphedema was significantly different from that in the contralateral limb (p<0.001), 54.6% of the women had increased flow. In the axillary vein, 45.4% had increased flow and 45.4% had decreased flow, with a statistically significant difference (p<0.01) between limbs. Compared to the contralateral limb, significant lymphatic changes (p<0.05) were also found in the vessel route (not visualized), number of lymphatic vessels (none), axillary lymph nodes (absent) and dermal reflux (present). In the contralateral upper limb without lymphedema, no venous or lymphatic alterations were encountered. CONCLUSION: The women subjected to axillary lymphadenectomy for the treatment of breast cancer presented both venous and lymphatic changes in the upper limb with lymphedema.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(3):97-102
DOI 10.1590/S0100-72032013000300002
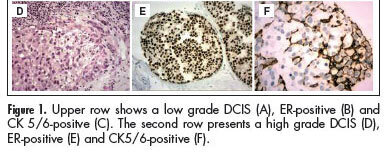
PURPOSE:To compare the prognostic and predictive features between in situ and invasive components of ductal breast carcinomas. METHODS:We selected 146 consecutive breast samples with ductal carcinoma in situ (DCIS) associated with adjacent invasive breast carcinoma (IBC). We evaluated nuclear grade and immunohistochemical expression of estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2), cytokeratin 5/6 (CK5/6), and epidermal growth factor receptor (EGFR) in both components, in situ and invasive, and the Ki-67 percentage of cells in the invasive part. The DCIS and IBC were classified in molecular surrogate types determined by the immunohistochemical profile as luminal (RE/PR-positive/ HER2-negative), triple-positive (RE/RP/HER2-positive), HER2-enriched (ER/PR-negative/HER2-positive), and triple-negative (RE/RP/HER2-negative). Discrimination between luminal A and luminal B was not performed due to statistical purposes. Correlations between the categories in the two groups were made using the Spearman correlation method. RESULTS:There was a significant correlation between nuclear grade (p<0.0001), expression of RE/RP (p<0.0001), overexpression of HER2 (p<0.0001), expression of EGFR (p<0.0001), and molecular profile (p<0.0001) between components in situ and IBC. CK 5/6 showed different distribution in DCIS and IBC, presenting a significant association with the triple-negative phenotype in IBC, but a negative association among DCIS. CONCLUSIONS: Our results suggest that classical prognostic and predictive features of IBC are already determined in the preinvasive stage of the disease. However the role of CK5/6 in invasive carcinoma may be different from the precursor lesions.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(2):78-83
DOI 10.1590/S0100-72032013000200007
PURPOSE: To understand the reproductive and sexual life of women treated for breast cancer. METHODS: A total of 139 women with a diagnosis made at least 6 months ago were interviewed after being randomly selected in a rehabilitation service. The interviews were carried out between 2006 and 2010. The inclusion criteria were: to have used a rehabilitation service between 2006 and 2010, to be a Unified Health System user, to have been a patient at a regional hospital and to be resident in the area of DRS XIII-Ribeirão Preto, state of São Paulo. The interviewees were visited at home where a face to face questionnaire regarding sociodemographic features and questions about the disease and reproductive and sexual life was administered. For the last one, the Female Sexual Function Index instrument was used. Data were analyzed statistically by the χ² test, Fisher exact test, Student's t test, multivariate analysis by logistic regression, factorial analysis and the Cronbach's alpha. RESULTS: Most patients had between 2 to 3 children and 80% used some contraceptive. About half of them had had sexual intercourse in the last month, 45.3% had interrupted sexual intercourse during treatment and 25.9% did not. There were reports of decreasing sexual activity, although half of the interviewees had re-started sexual life during the first six months after treatment. About half presented sexual dissatisfaction. An active sexual life is associated with being younger than 40 years of age and to have a partner. No association was found between active sexual life and diagnosis and types of treatment. CONCLUSION: Sexual activity of women treated for breast cancer is not associated with the treatments, but with age and with the opportunity of having sex.