-
Original Article
Mortality from Breast Cancer in Women under 50 Years of Age in Colombia
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):775-779
01-11-2023
Summary
Original ArticleMortality from Breast Cancer in Women under 50 Years of Age in Colombia
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):775-779
01-11-2023Views86See moreAbstract
Objective
To calculate and analyze the mortality rates from breast cancer in women under 50 years of age in Colombia and to compare them with those of other countries in the region.
Methods
Based on data from the registry of deaths in 2018 and the results of the National Population and Housing Census of Colombia for the same year, specific mortality rates in women with breast cancer, specific mortality according to age group, standardized by age, proportional mortality, potential years of life lost, and years of life expectancy lost in women under 50 years of age who died from breast cancer were calculated. The mortality rate of regional countries was consulted on the Global Cancer Observatory webpage.
Results
In the group from 20 to 49 years, the specific mortality rate was higher in the age range from 45 to 49 years, with a rate of 23.42 × 100,000, a value that was above the specific mortality rate due to breast cancer in women in Colombia, 15.17 × 100.000. In the age range of 45 to 49 years, the potential years of life lost were 42.16. Of the 0.275 years of life expectancy lost by the population due to this neoplasia, women under 50 years of age represented 0.091 (33%). Colombia is the fifth in the rank of mortality in Latin American countries in this age group.
Conclusion
Breast cancer in patients from 30 to 59 years is the number one cause for the decrease in life expectancy of women in Colombia. Women under 50 years of age represent one third of this decrease. This neoplasm is also the leading cause of mortality in women younger than 50 years in South America.
-
Original Article
Treatment and Management Experience of Idiopathic Granulomatous Mastitis in a Low-income Country
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(6):319-324
08-04-2023
Summary
Original ArticleTreatment and Management Experience of Idiopathic Granulomatous Mastitis in a Low-income Country
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(6):319-324
08-04-2023Views175See moreAbstract
Objective
Reporting our experience of the management and treatment of Idiopathic granulomatous mastitis (IGM) in a low-income country by describing patients characteristics and therapy with emphasis on conservative surgical excision and postoperative care as the cornerstone of treatment.
Methods
A retrospective cohort of women with histopathological diagnosis of IGM from 2014 to 2018 at Instituto Nacional Materno Perinatal in Lima, Peru. Patients' characteristics, clinical presentation, treatment, management, postoperative care, and follow-up were analyzed.
Results
Thirty-eight patients with histopathological diagnosis of IGM were identified. Their average age was 35.9 years and 23 (60.5%) reported previous use of hormonal contraceptives. Nine (23.7%) patients had chronic mastitis with previous treatment. The time from the onset of symptoms to the first clinic consult was 5.1 months on average. Twenty-one (55.3%) patients had the lesion in the right breast, with a mean size of 6.9 cm. Conservative surgical excision was performed in all patients. Additionally, 86.8% required corticosteroids and 78.9% were treated with antibiotics. Complete remission was obtained at 141 days on average (range 44 to 292 days). Six (15.8%) women reported ipsilateral recurrence and 5 (13.2%), contralateral. The latency time was 25.5 months on average.
Conclusion
The conservative surgical treatment demonstrated and close follow-up made for a high cure rate, but with recurrence similar to that reported in the literature. Use of gloves is an alternative to manage post operative wounds in a low-income country. The most frequent adverse effect was breast surgical scar.
-
Original Article
Effect of Testosterone on Proliferation Markers and Apoptosis in Breasts of Ovariectomized Rats
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(12):703-709
02-03-2019
Summary
Original ArticleEffect of Testosterone on Proliferation Markers and Apoptosis in Breasts of Ovariectomized Rats
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(12):703-709
02-03-2019Views161See moreAbstract
Objective
To investigate the action of testosterone (T), isolated or associated with estradiol benzoate (EB), on the proliferation markers and apoptosis of breasts of ovariectomized rats.
Methods
A total of 48 castrated female Wistar rats were divided into 6 groups, and each of them were submitted to one of the following treatments for 5 weeks: 1) control; 2) EB 50 mcg/day + T 50 mcg/day; 3) T 50mcg/day; 4) EB 50 mcg +T 300 mcg/day; 5) T 300 mcg/day; and 6) EB 50 mcg/day. After the treatment, the mammary tissue was submitted to a histological analysis and immunoexpression evaluation of proliferation markers (proliferating cell nuclear antigen, PCNA) and apoptosis (caspase-3).
Results
There was a statistically significant difference among the groups regarding microcalcifications and secretory activity, with higher prevalence in the groups treated with EB. There was no difference among the groups regarding atrophy, but a higher prevalence of atrophy was found in the groups that received T versus those that received EB +T. There was a difference among the groups regarding the PCNA (p = 0.028), with higher expression in the group submitted to EB +T 300 mcg/day. Regarding caspase-3, there was no difference among the groups; however, in the group submitted to EB +T 300 mcg/day, the expression was higher than in the isolated T group.
Conclusion
Isolated T did not have a proliferative effect on the mammary tissue, contrary to EB. Testosterone in combination with EB may or may not decrease the proliferation, depending on the dose of T.
-
Case Report
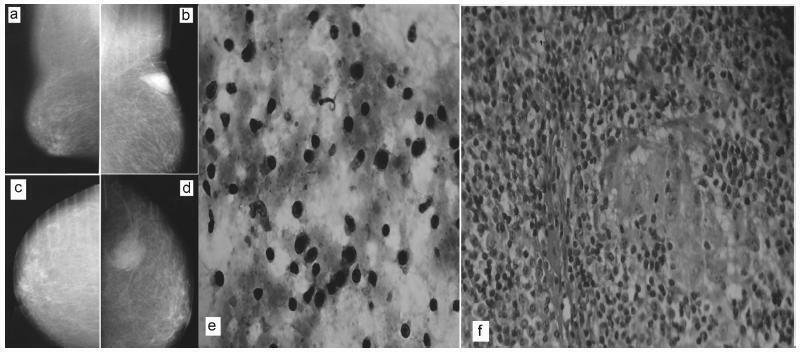
Fine-needle Aspiration Cytology to Identify a Rare Mimicker of Breast Cancer: Plasma Cell Mastitis
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):491-493
08-01-2018
Summary
Case ReportFine-needle Aspiration Cytology to Identify a Rare Mimicker of Breast Cancer: Plasma Cell Mastitis
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):491-493
08-01-2018Views110See moreAbstract
There are rare benign diseases that can mimic malignant breast neoplasms in the clinical exam and in mammography. We evaluated the contribution of an accessible procedure to most clinicians, the fine-needle aspiration cytology, to identify a rare mimicker of malignant breast neoplasms. A type 2 diabetic 85-year-old female presented with a 6-month history of a left breast lump. The physical exam and mammography were compatible with breast cancer. Nevertheless, after fine-needle aspiration cytology, the diagnosis was plasma cellmastitis. Once this rare diagnosis was established, the tumor was extirpated, and the final histologic diagnosis corroborated chronic plasma cellmastitis. The patient’s postoperative evolution was uneventful, and no other treatment was needed. Fine-needle aspiration cytology could be a valuable tool to identify rare mimickers of malignant breast neoplasms.
-
Original Article
Molecular Subtypes of Breast Cancer Are Not Associated with the Clinical Under- or Overstaging of Breast Cancer
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(5):239-245
05-01-2016
Summary
Original ArticleMolecular Subtypes of Breast Cancer Are Not Associated with the Clinical Under- or Overstaging of Breast Cancer
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(5):239-245
05-01-2016Views126See moreAbstract
Purpose
to evaluate the agreement between the clinical and pathological stagings of breast cancer based on clinical and molecular features.
Methods
this was a cross-sectional study, in which clinical, epidemiological and pathological data were collected from 226 patients who underwent surgery at the Prof. Dr. José Aristodemo Pinotti Women's Hospital (CAISM/Unicamp) from January 2008 to September 2010. Patients were staged clinically and pathologically, and were classified as: understaged, when the clinical staging was lower than the pathological staging; correctly staged, when the clinical staging was the same as the pathological one; and overstaged, when the clinical staging was greater than the pathological staging.
Results
understaged patients were younger (52.2 years; p < 0.01) and more symptomatic at diagnosis (p = 0.04) when compared with correctly or overstaged patients. Clinicopathological surrogate subtype, menopausal status, parity, hormone replace therapy and histology were not associated with differences in staging. Women under 57 years of age were clinically understaged mainly due to underestimation of T ( tumor staging) (p < 0.001), as were the premenopausal women (p < 0.01). Patients whose diagnosis was made due to clinical complaints, and not by screening, were clinically understaged due to underestimation of N (lymph nodes staging) (p < 0.001).
Conclusion
the study shows that the clinicopathological surrogate subtype is not associated with differences in staging, while younger women diagnosed because of clinical complaints tend to have their breast tumors understaged during clinical evaluation.
-
Case Report
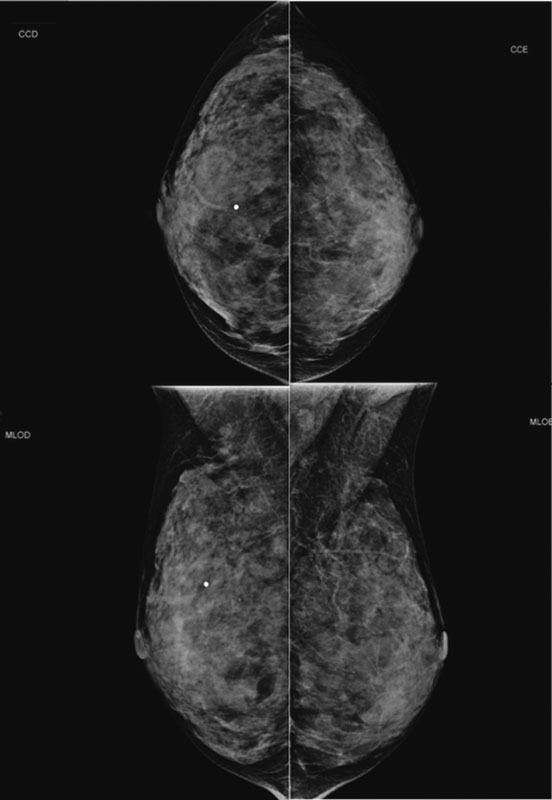
Lobular Carcinoma in Situ with Atypical Mass Presentation: a Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(2):112-116
02-01-2016
Summary
Case ReportLobular Carcinoma in Situ with Atypical Mass Presentation: a Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(2):112-116
02-01-2016Views176See moreLobular carcinoma in situ (LCIS) is associated with an increased risk of breast cancer and accounts for 1 to 2% of all breast cancers. LCIS diagnosis currently remains one of the major identifiable risk factors for subsequent breast cancer development. Imaging methods are becoming increasingly sensitive, and the consequent detection of small lesions and subtle abnormalities increases the chance of detection of in situ and invasive carcinomas, leading to a reduction in mortality. This report describes a case of a palpable complaint with abnormal imaging findings, including a solid LCIS mass.
-
Article
Volume of breast tissue excised during breast-conserving surgery in patients undergoing preoperative systemic therapy
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(5):221-225
07-05-2013
Summary
ArticleVolume of breast tissue excised during breast-conserving surgery in patients undergoing preoperative systemic therapy
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(5):221-225
07-05-2013DOI 10.1590/S0100-72032013000500006
Views111See morePURPOSE: We aimed to determine whether clinical examination could adequately ascertain the volume of tissue to be resected during breast-conserving surgery after neoadjuvant therapy. METHODS: We reviewed the clinical reports of 279 patients with histologically diagnosed invasive breast carcinomas treated with neoadjuvant therapy followed by surgery or with primary surgery alone. We estimated volumes of excised tissues, the volume of the tumor mass and the optimal volume required for excision based on 1 cm of clear margins. The actual excess of resected volume was estimated by calculating the resection ratio measured as the volume of the resected specimen divided by the optimal specimen volume. The study endpoints were to analyze the extent of tissue resection and to ascertain the effect of excess resected tissue on surgical margins in both groups of patients. RESULTS: The median tumor diameter was 2.0 and 1.5 cm in the surgery and neoadjuvant therapy groups, respectively. The median volume of resected mammary tissue was 64.3 cm³ in the primary surgery group and 90.7 cm³ in the neoadjuvant therapy group. The median resection ratios in the primary surgery and neoadjuvant therapy groups were 2.0 and 3.3, respectively (p<0.0001). Surgical margin data were similar in both groups. Comparison of the volume of resected mammary tissues with the tumor diameters showed a positive correlation in the primary surgery group and no correlation in the neoadjuvant therapy group. CONCLUSION: Surgeons tend to excise large volumes of tissue during breast-conserving surgery after neoadjuvant therapy, thereby resulting in a loss of the correlation between tumor diameter and volume of the excised specimen.


