Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(12):771-778
12-01-2018
To assess the sexual function, anxiety, and depression of infertile women relative to a control group.
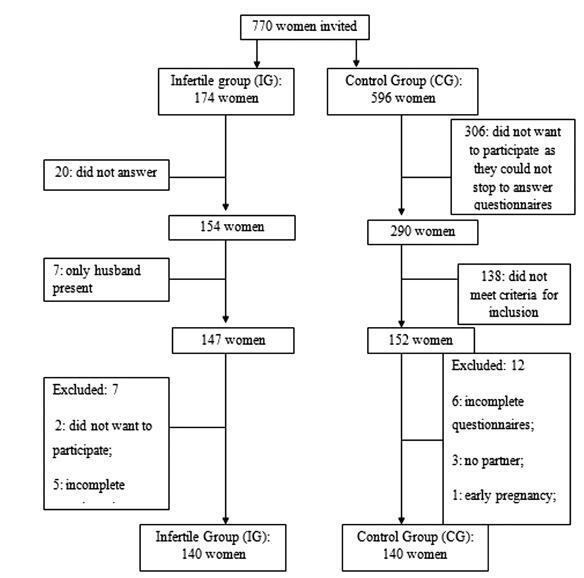
Infertile women (infertile group, IG) of reproductive age were invited to participate in this controlled study. A control group (CG) of women was recruited from the general population of the same city. Sexual function was assessed by the Female Sexual Function Index (FSFI), and anxiety and depression were measured by the Hospital Anxiety and Depression Scale (HADS).
A total of 280 women participated in the present study, 140 in the IG and 140 in the CG. The analysis of the FSFI scores showed that 47 women (33.57%) in the IG and 49 women (35%) in the CG had sexual dysfunction (FSFI ≤ 26.55; p = 0.90). Women with anxiety or depression had a greater risk of sexual dysfunction, and sexual dysfunction increased the risk of anxiety and depression. Married women had a lower risk of depression than single women who were living with their partners.
Infertilewomenhadno increased riskof sexual dysfunction relativetocontrols. Anxiety and depression increased the risk of sexual dysfunction in the studied population.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(5):218-224
05-01-2016
To evaluate whether women with endometriosis have different ovarian reserves and reproductive outcomes when compared with women without this diagnosis undergoing in vitro fertilization/intracytoplasmic sperm injection ( IVF/ ICSI), and to compare the reproductive outcomes between women with and without the diagnosis considering the ovarian reserve assessed by antral follicle count ( AFC ).
This retrospective cohort study evaluated all women who underwent IVF/ ICSI in a university hospital in Brazil between January 2011 and December 2012. All patients were followed up until a negative pregnancy test or until the end of the pregnancy. The primary outcomes assessed were number of retrieved oocytes and live birth. Women were divided into two groups according to the diagnosis of endometriosis, and each group was divided again into a group that had AFC 6 (poor ovarian reserve) and another that had AFC 7 (normal ovarian reserve). Continuous variables with normal distribution were compared using unpaired t-test, and those without normal distribution, using Mann-Whitney test. Binary data were compared using either Fisher's exact test or Chi-square (2) test. The significance level was set as p < 0.05.
787 women underwent IVF/ICSI (241 of which had endometriosis). Although the mean age has been similar between women with and without the diagnosis of endometriosis (33.8 4 versus 33.7 4.4 years, respectively), poor ovarian reserves were much more common in women with endometriosis (39.8 versus 22.7%). The chance of achieving live birth was similar between women with the diagnosis of endometriosis and those without it (19.1 versus 22.5%), and also when considering only women with a poor ovarian reserve (9.4 versus 8.9%) and only those with a normal ovarian reserve (25.5 versus 26.5%).
Women diagnosed with endometriosis are more likely to have a poor ovarian reserve; however, their chance of conceiving by IVF/ICSI is similar to the one observed in patients without endometriosis and with a comparable ovarian reserve.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(9):679-686
01-19-2003
DOI 10.1590/S0100-72032003000900010
PURPOSE: to evaluate the first in vitro fertilization results at a medical university using low-cost programmed cycles. METHODS: from May to December 2002, 66 programmed cycles of in vitro fertilization were carried out using norethisterone acetate, clomiphene citrate and human chorionic gonadotrophin (hCG). The ovarian follicle aspiration was guided by ultrasonography, 34 to 36 h after the administration of hCG, and the embryo transfer, 48 h after puncturing. The diagnosis of clinical pregnancy was defined when a pulsating heart was detected by transvaginal ultrasonography. RESULTS: the cycle cancelation rate was 21.2%. An average of 2.8 follicles and 1.7 oocytes were obtained per puncture. In 79.6% of the punctured cycles it was possible to retrieve oocytes and 69% of them were fertilized. The number of embryos per transfer was 1.5. Some level of difficulty occurred in 10.2% of the aspiration procedures and 32.4% in the embryo transfer. The obtained pregnancy rate was 10,8% per transfer; however, the drug cost per transferred embryo was only R$ 96,00. CONCLUSION: the difficulty to begin an in vitro fertilization program in a medical school, not aiming at profits and to help a population without financial possibilities, became evident. After progressive experience, the cumulative pregnancy rate tends to be similar to that of reference centers, but with significantly lower costs and incidence of complications.