-
Original Article
Switching of Hormone Therapies in Breast Cancer Women
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):185-189
01-19-2021
Summary
Original ArticleSwitching of Hormone Therapies in Breast Cancer Women
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):185-189
01-19-2021Views72See moreAbstract
Objective
The objective of the present study was to analyze the reasons that led to hormone therapies (HTs) regimen changes in women with breast cancer.
Methods
This was a retrospective cross-sectional study from a single-institution Brazilian cancer center with patient records diagnosed with breast cancer between January 2012 and January 2017.
Results
From 1,555 women who were in treatment with HT, 213 (13.7%) women had HT switched, either tamoxifen to anastrozole or vice-versa. Most women included in the present study who switched HT were > 50 years old, postmenopausal, Caucasian, and had at least one comorbidity. From the group with therapy change, ‘disease progression’ was reason of change in 124 (58.2%) cases, and in 65 (30.5%) patients, ‘presence of side effects’ was the reason. From those women who suffered with side effects, 24 (36.9%) had comorbidities.
Conclusion
The present study demonstrated a low rate of HT switch of tamoxifen to anastrozole. Among the reasons for changing therapy, the most common was disease progression, which includes cancer recurrence, metastasis or increased tumor. Side effects were second; furthermore, age and comorbidities are risk factors for side effects.
-
Original Articles
Estrone and Estradiol Levels in Breast Cancer Patients Using Anastrozole Are Not Related to Body Mass Index
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(1):14-20
01-01-2017
Summary
Original ArticlesEstrone and Estradiol Levels in Breast Cancer Patients Using Anastrozole Are Not Related to Body Mass Index
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(1):14-20
01-01-2017Views128See moreABSTRACT
Objective:
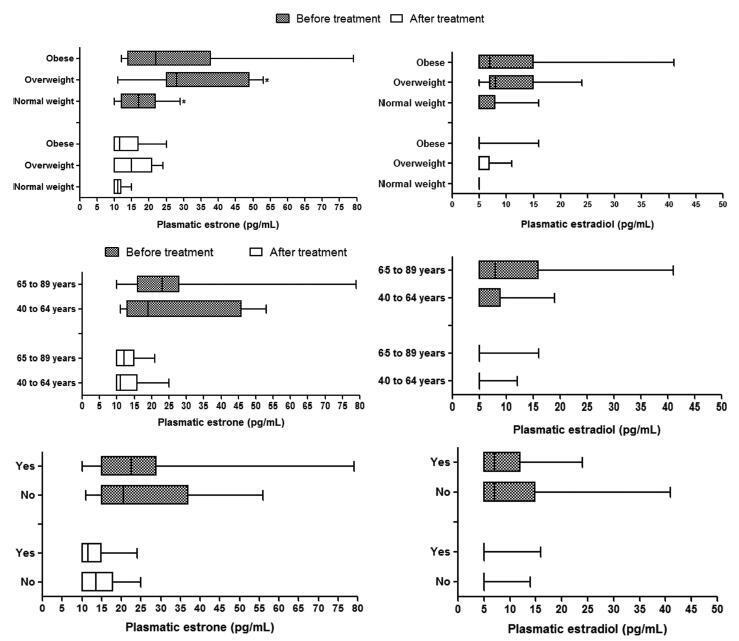
Obesity is associated with an increased risk for breast cancer. Recent studies have shown that aromatase inhibitors may be less effective in women with a high body mass index (BMI). The aim of this study was to establish the relationship between the BMI and plasma estrone and estradiol levels in postmenopausal women with hormone receptor-positive breast cancer using anastrozole.
Methods:
In this cohort study, the patients were divided into three groups according to BMI (normal weight, overweight and obese) to compare and correlate plasma hormone levels before starting anastrozole hormone therapy and three months after treatment. Plasma hormone levels were compared for age and use of chemotherapy.
Results:
A statistically significant reduction in estrone and estradiol levels was observed between baseline and three months after starting the anastrozole treatment (p < 0.05). There was no statistically significant difference in plasma estrone and estradiol levels among the BMI groups (p > 0.05), but a significant reduction in plasma estrone levels was observed after three-months' treatment relative to baseline in all groups, as well as a reduction in estradiol in the obese group (p < 0.05). The use of chemotherapy and age > 65 years had no influence on plasma steroid levels.
Conclusion:
Changes in estrone and estradiol levels in the studied groups were not associated with BMI, chemotherapy or age.