You searched for:"Marcelo Zugaib"
We found (76) results for your search.Summary
Rev Bras Ginecol Obstet. 2001;23(8):529-533
DOI 10.1590/S0100-72032001000800008
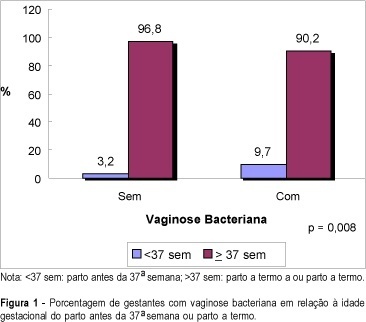
Purpose: to evaluate the relationship between bacterial vaginosis (BV) and spontaneous preterm delivery. Method: a total of 611 pregnant women from the general antenatal clinic of the "Clínica Obstétrica do Hospital das Clínicas da Universidade de São Paulo" were enrolled in this study. All pregnancies were dated by an early scan. Iatrogenic preterm deliveries were excluded. The presence of bacterial vaginosis was evaluated between 23 and 24 weeks of pregnancy by a Gram stain of the vaginal smear collected from the posterior vaginal wall using a sterile swab. Vaginal pH was also assessed from the lateral vaginal wall by a Universal 0-14 pH strip produced by Merck. Result: a complete follow-up was obtained in 551 patients and bacterial vaginosis was diagnosed in 103 (19%) cases. Among the patients with BV in the vaginal smear, 9.7% delivered before 37 weeks against only 3.2% in the group with normal vaginal smear (p=0.008). The sensitivity, specificity, accuracy and false-positive rate for preterm delivery in the presence of bacterial vaginosis on Gram stain of the vaginal smear were 41.7, 82, 80.2 and 18%, respectively, with a relative risk of 1.8 for preterm delivery. The mean vaginal pH in the group of positive BV was 4.9 and in the group with normal smear it was 4.3 (p=0.0001). Conclusion: bacterial vaginosis during pregnancy increases the risk for spontaneous preterm delivery, with a relative risk of 1.8.
Summary
Rev Bras Ginecol Obstet. 2009;31(11):547-551
DOI 10.1590/S0100-72032009001100004
PURPOSE: to study the effect of acoustic stimulation in the fetal cardiac response, according to parameters from computerized cardiotocography in low risk pregnancies. METHODS: twenty low risk pregnant women were included in the study, according to the following criteria: age over 18; single gestation, living fetus; gestational age between 36 and 40 weeks; amniotic liquid index over 8.0 cm and absence of fetal malformation. Cases with post-natal diagnosis of fetal anomaly were excluded. Computerized cardiotocography was performed for 20 minutes, before and after fetal acoustic stimulation. Results were analyzed by the t test for dependent samples, with significance level at p<0.05. RESULTS: acoustic stimulation was successfully performed in all cases analyzed. By the analysis of the cardiotocographic parameters, there was no significant difference when the pre and post-stimulation parameters were compared: average number of fetal movements per hour (55.6 versus 71.9, p=0.1); mean basal fetal heart rate (FHR) (135.2 versus 137.5 bpm, p=0.3); mean FHR increases>10 bpm (6.5 versus 6.8, p=0.7); mean FHR increases>15 bpm (3.8 versus 4.3, p=0.5); mean duration of high FHR variation episodes (11.4 versus 10.9 min, p=0.7); mean duration of low FHR variation episodes (2.5 versus 1.1 min, p=0.2), and mean short-term variation (10.6 versus 10.9 ms, p=0.6). CONCLUSIONS: in low risk gestations at term, computerized cardiotocography has not evidenced differences in the FHR parameters after the fetal sonic stimulation.
Summary
Rev Bras Ginecol Obstet. 2013;35(2):55-59
DOI 10.1590/S0100-72032013000200003
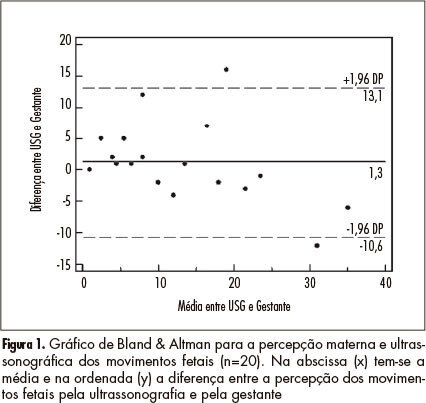
PURPOSE: To determine the agreement between maternal perception of fetal movements and the movements recorded simultaneously by ultrasound in low-risk pregnancies. METHODS: Twenty pregnant women were evaluated with the following inclusion criteria: single pregnancy, alive fetus, maternal age between 18 and 35 years; between 36 and 40 weeks gestation; normal fetal morphology at ultrasound, and absence of maternal comorbidities. The pregnant women were evaluated for 10 minutes, during which cardiotocography was used to record fetal movements triggered with the event marker, with the paper speed set at 3 cm/min. At the same time, fetal movements were observed by ultrasonography. RESULTS: The kappa index for interobserver agreement analysis was 0.62, showing good agreement (95%CI 0.45 - 0.79). The intraclass correlation coefficient was 0.82 (95%CI 0.61 - 0.92). Analysis by the Bland & Altman graph indicated good agreement. A linear regression analysis showed a significant correlation between maternal perception (x) and ultrasound (y) observation (r²=0.71, p<0.001; equation: y=5.31+0.66x). CONCLUSIONS: The agreement between ultrasound and maternal perception of fetal movement is good, allowing the use of fetal movement counting in the assessment of fetal wellbeing.
Summary
Rev Bras Ginecol Obstet. 2000;22(9):557-566
DOI 10.1590/S0100-72032000000900004
Purpose: to study the fetal well-being assessment in pregnancies complicated by diabetes, and to analyze the neonatal results. Methods: we studied 387 pregnant women with diabetes at the Fetal Surveillance Unit. The last examination (cardiotocography, fetal biophysical profile, amniotic fluid index and dopplervelocimetry) was correlated with the neonatal outcome. Results: the studied population included 46 (12%) type I diabetes, 45 (12%) type II and 296 (76%) gestational diabetes. Type I diabetes with abnormal or suspected cardiotocography was related to abnormal 1st minute Apgar (50 and 75%, p<0.05) and to the need for neonatal intensive care unit (50 and 75%, p<0.05). The abnormal biophysical profile in type II diabetic pregnancy was related to the need for neonatal intensive care (67%, p<0.05), and abnormal umbilical artery Doppler study was related to abnormal 1st minute Apgar (67%, p<0.05). Gestational diabetes with abnormal cardiotocography presented 36% abnormal 1st minute Apgar (p<0.05), 18% abnormal 5th minute Apgar (p<0.01) and 18% neonatal death (p<0.01). Abnormal amniotic fluid index was related to abnormal 5th minute Apgar (p<0.05) and need for neonatal intensive care unit (p<0.05). Gestational diabetes with abnormal umbilical artery Doppler was related (p<0.05) to: abnormal 1st and 5th minute Apgar, respectively, 25 and 8%, Need for neonatal intensive care in 17% and neonatal death in 8%. Conclusions: the fetal well-being examinations correlated with adverse perinatal outcome, showing the need for fetal surveillance in diabetic pregnant women.
Summary
Rev Bras Ginecol Obstet. 2001;23(9):561-566
DOI 10.1590/S0100-72032001000900003
Purpose: to evaluate fetuses with facial cleft as to type of lesion, associated malformations and aneuploidies. Method: the following parameters were evaluated: maternal age and previous history, gestational age at diagnosis, lesion side, type of lesion, presence of associated malformations and aneuploidies, mortality rate and postnatal follow-up. Results: forty fetuses had facial cleft, 18 (45%) cases had cleft lip, 19 (47.5%) had cleft lip and palate, and 3 (7.5%) cases presented with cleft palate. Isolated facial cleft was observed in 10 fetuses (25%), all of them unilaterally located. Aneuploidies were identified in 10/30 (33.33%) of the patients with associated malformations. Cleft lip and palate was more often seen in this group (18/30 - 60%), followed by bilateral lesion (8/30 - 26.7%) and median cleft (10/30 - 33.3%). Conclusion: facial clefts are considered excellent signs for the presence of associated malformations and fetal aneuploidies. Fetuses with facial cleft must be referred to specialized centers in order to have specialized ultrasound and genetic analysis which can provide the best prenatal counseling for these cases. Isolated facial cleft was associated with very good prognosis.

Summary
Rev Bras Ginecol Obstet. 2005;27(9):561-566
DOI 10.1590/S0100-72032005000900010
Preterm delivery is the most common cause of neonatal morbidity and mortality. About 75% of preterm births follow preterm labor. The pathogenesis of spontaneous preterm birth is complex and its clinical management is based on a careful assessment of the risks for mother and infant and on continuing the pregnancy versus delivery. The goal of the present article is to review the diagnosis of preterm labor, the tocolytic treatment, glucocorticoid therapy, antimicrobial treatment, and management of progressive preterm labor.
Summary
Rev Bras Ginecol Obstet. 2015;37(12):565-570
DOI 10.1590/SO100-720320150005488
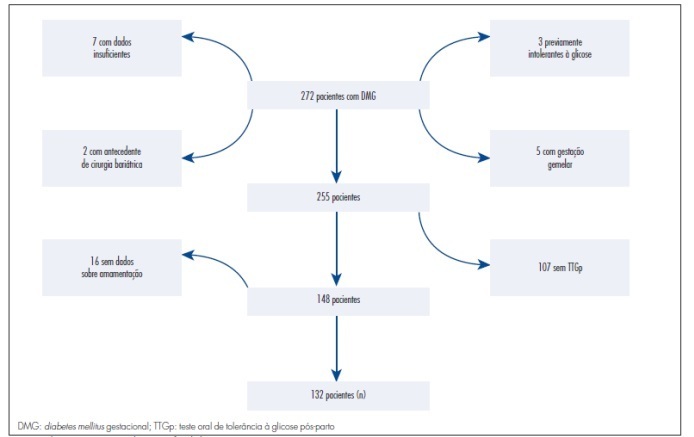
To determine the influence of breastfeeding on the results of a postpartum oral glucose tolerance test in women recently diagnosed with gestational diabetes mellitus.
The data were obtained from the electronic medical records of the Endocrinopathy Sector during pregnancy, HCMED laboratory system ofHospital das Clínicas of São Paulo , and by telephone. According to the inclusion criteria adopted, 132 patients were eligible for the study. For statistical analysis, the patients were divided into two groups according to whether or not they breastfed. The results were analyzed by the Student t-test and by the Mann-Whitney, Chi-square and Fisher's exact tests, depending on the variable analyzed, with the level of significance set at p<0.05.
Of the 132 patients included in the study, 114 breastfed and 18 did not. Most of the patients in both groups were overweight or obese. The breastfeeding group had a lower pre-pregnancy Body Mass Index than the non-breastfeeding group (p=0.006). Insulin was introduced earlier in the group that did not breastfeed (23.21±4.33 versus 28.84±6.17; p=0.04). The group that did not breastfeed had a higher mean postpartum fasting glucose value in the oral glucose tolerance test than the group that breastfed (91.3±8.7 versus 86.5±9.3; p=0.01). Breastfeeding acted as a protective factor against the development of glucose intolerance in the postpartum oral glucose tolerance test (OR=0.27; 95%CI 0.09-0.8). By logistic regression, breastfeeding was shown to be an independent protective factor.
There was a statistically significant relationship between breastfeeding and a decreased risk of developing glucose intolerance. Breastfeeding should be encouraged because it is an effective, low cost intervention easily accessible to all patients during the postpartum period.
Summary
Rev Bras Ginecol Obstet. 1999;21(10):569-576
DOI 10.1590/S0100-72031999001000002
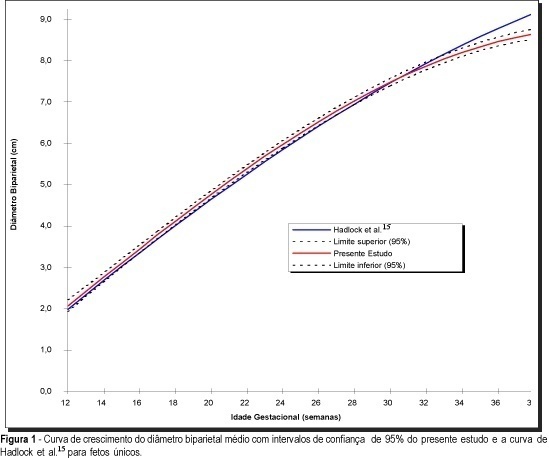
Purpose: to estimate growth curves and tables of average biparietal diameter and average head circumference of twin gestations and to compare them with published growth curves for singletons and twins. Methods: growth curves and tables of average biparietal diameter and average head circumference were obtained from sonographic examinations of 34 patients with twin gestations without maternal and fetal complications. Sonographic examinations were performed each 2 or 3 weeks by a single observer. The parameters were compared with existing growth curves for singletons and twins. Results: curves and tables of biparietal diameter and head circumference in relation to gestational age were obtained. The study revealed difference in growth pattern mainly regarding the 3rd trimester in relation to singletons (Hadlock et al.15). The difference between the average values were 6 mm (biparietal diameter) and 2.0 cm (head circumference) at the 39th week of gestation. Also, some differences were observed relative to the twin studies. Conclusion: this study revealed that growth curves for average biparietal diameter and average head circumference of singletons are not appropriate to determine gestational age in twin gestations of the studiced population principally at the 3rd trimester