You searched for:"Edmund Chada Baracat"
We found (71) results for your search.Summary
Rev Bras Ginecol Obstet. 2005;27(9):524-528
DOI 10.1590/S0100-72032005000900004
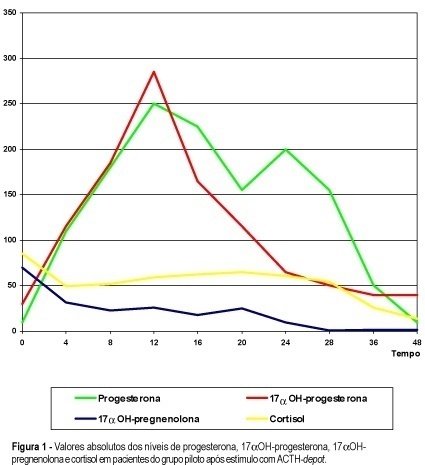
PURPOSE: to evaluate the morphological changes in murine lacrimal glands by metoclopramide-induced hyperprolactinemia during the proestrus phase or pregnancy. METHODS: forty adult mice were divided into two groups: CTR1 (control) and MET1 (treated with metoclopramide). After fifty days, half of the mice were sacrificed. The remaining animals were mated, and then labeled as pregnant controls (CTR2). Part of these animals were treated with metoclopramide and constituted the metoclopramide-treated pregnant (MET2) group. The CTR2 and MET2 groups were sacrificed on the 6th day of pregnancy. The blood was collected for determination of the hormonal levels of estradiol and progesterone by a chemoluminescent method. The lacrimal glands were then removed, fixed in 10% formaldehyde and stained with HE. The morphometric analysis was performed using the Axion Vision program (Carl Zeiss) to measure acinar nuclear and cellular volumes. RESULTS: the nuclear and cellular volumes of the lacrimal glands in the MET1-(152.2±8.7; 6.3±1.6 µm³) and MET2-(278.3±7.9; 27.5±0.9 µm³) treated groups were lower than those in CTR1 (204.2±7.4; 21.9±1.3 µm³) and CTR2 (329.4±2.2; 35.5±2.0 µm³), respectively. There was a significant hormonal level reduction in the animals that received metoclopramide compared to controls (CTR1: estradiol = 156.6±42.2 pg/ml; progesterone = 39.4±5.1 ng/ml; MET1: estradiol = 108.0±33.1 pg/ml; progesterone = 28.0±6.4 ng/ml; CTR2: estradiol = 354.0±56.0 pg/ml; progesterone = 251.0±56.0 ng/ml; MET2: estradiol = 293.0±43.0 pg/ml, progesterone = 184.0±33.0 ng/ml). CONCLUSION: metoclopramide-induced hyperprolactinemia produced morphological signs of reduction of cellular activity in lacrimal glands during the proestrus phase and pregnancy. It is hypothesized that this effect might be related to the hyperprolactinemia-induced decrease in the hormonal production of estrogen and progesterone.
Summary
Rev Bras Ginecol Obstet. 2010;32(11):530-535
DOI 10.1590/S0100-72032010001100003
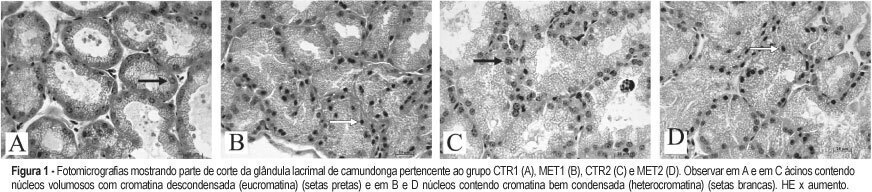
PURPOSE: to evaluate the effectiveness of uterine fibroid embolization (UFE) in patients with giant fibroids, with regard to both clinical outcomes and size reduction. METHODS: twenty-six patients with a mean age of 36.5 years, carrying symptomatic fibroids with a volume over 1,000 cm³, were referred for UFE. All patients had indication for percutaneous treatment. The procedures were performed under epidural anesthesia and sedation, using an institutional protocol. By unilateral femoral access, selective catheterization of uterine arteries and infusion of calibrated microspheres through microcatheter were carried out. Clinical evaluation was performed by means of regular outpatient gynecology consultation. All patients underwent magnetic resonance imaging (MRI) before the procedure and 15 patients underwent control MRI after 6 months. RESULTS: technical success was 100%. There was no complication related to the procedures. Mean uterine volume of the 15 patients studied was 1,401 cm³ before embolization (min 1,045 cm³, max 2,137 cm³) and 799 cm³ after 6 months (525 cm³ min, max. 1,604 cm³), resulting in a total reduction of 42.9%. Clinical improvement was observed in 25 of 26 patients. One woman with uterine volume of 1,098 cm³ who developed necrosis and partial fibroid expulsion underwent myomectomy. Another patient was submitted to myomectomy six months after the procedure because she wanted to become pregnant, despite partial fibroid size reduction. One patient with a uterine volume of 2,201 cm³ required a second intervention to achieve an adequate angiographic result. No patient underwent hysterectomy. On average, 9.2 microsphere syringes were used per patient. CONCLUSION: embolization of giant uterine fibroids is a feasible procedure with acceptable clinical and radiological outcomes. It can be considered an option for patients who desire to preserve the uterus, and it may serve as adjuvant therapy for high-risk myomectomy.
Summary
Rev Bras Ginecol Obstet. 1998;20(9):533-536
DOI 10.1590/S0100-72031998000900007
Purpose: to evaluate the effects of tamoxifen (TAM) on plasma levels of estradiol, progesterone, prolactin, luteinizing hormone (LH), follicle-stimulating hormone (FSH) and steroid hormone-binding globulin (SHBG) when given to premenopausal women in the doses of 10 and 20 mg/day for 22 days. Patients and Methods: a randomized double-blind study was performed with 43 premenopausal eumenorrheic women. The patients were divided into three groups: A (N = 15, placebo); B (N = 15, TAM 10 mg/day) and C (N = 13, 20 mg/day). They started taking an oral dose of TAM or placebo on the very first day of the menstrual cycle. Two hormone determinations were performed, both on the 22nd day of the menstrual cycle: the first in the cycle that preceded the use of the drug and the second, in the following cycle, after 22 days of using the medication. We used the Levine and Student tests in order to evaluate the homogeneity of the sample and the variation of the hormone determinations respectively. Results:serum levels of estradiol, progesterone and SHBG increased significantly in groups B and C. In group C, we also observed increase in serum level of FSH (p < 0.0045) and a fall in prolactin level (p < 0.0055). Conclusions: TAM promoted a significant increase in serum concentrations of estradiol, progesterone and SHBG either in the doses of 10 or 20 mg/day. However, significant increase in FSH and decrease in prolactin were obtained only with the dose of 20 mg/day.
Summary
Rev Bras Ginecol Obstet. 2006;28(1):54-62
DOI 10.1590/S0100-72032006000100010
Female lower urinary tract symptoms are nonspecific and a clinical evaluation is required to establish the correct diagnosis. Such evaluation should consist of a structured micturition history or questionnaire, physical examination, micturition diary, pad test, and urodynamic evaluation. Urodynamic investigation was developed as an extension of patient history and physical examination in order to reveal the etiology of the patient's complaints. The goal of the present article is to review clinical and subsidiary diagnosis of urinary incontinence.
Summary
Rev Bras Ginecol Obstet. 2006;28(9):545-550
DOI 10.1590/S0100-72032006000900007
PURPOSE: to evaluate muscular strength of the pelvic floor and the periurethral vessels of postmenopausal women before and after six months of soybean extract treatment. METHODS: the study was conducted on 30 postmenopausal women before and after six consecutive months of soyabean extract (100 mg/day) administration. Urinary loss and muscular strength of the pelvic floor were investigated through digital perineometer and functional evaluation. Digital color Doppler in the periurethral region was used to count the number of vessels. For statistical analysis, the paired Student t test was applied to compare the results before and after the treatment. RESULTS: twenty women reported urinary incontinence before the treatment period. The amelioration of this symptom was observed in 15 (75%) women after the treatment. Vaginal pressure (muscular strength of the pelvic floor) was 12.95±1.73 and 15.86±1.86 Sauers, before and after the treatment, respectively (p<0.001). Twenty-two women (73.3%) presented an increase in the pressure at the end of this study. In relation to the function evaluation, 18 (60%) had improvement in muscular strength and 12 women did not present any change. On ultrasonography (Doppler), the number of vessels was 2.20±0.15 blood vessels/field in the beginning of this study and 3.46±0.25 blood vessels/field at the end of the treatment (p<0.001). An increase in the number of periurethral vessels was detected in 21 women (70%). CONCLUSION: it is important to emphasize that these are preliminary results. A double blind randomized and placebo-controlled clinical trial with a high number of participants is necessary. However, the treatment with concentrated soybean extract (100 mg per day) for six consecutive months may determine an improvement in pelvic floor muscular strength and an increase in the number of periurethral vessels in postmenopausal women.
Summary
Rev Bras Ginecol Obstet. 2002;24(9):573-577
DOI 10.1590/S0100-72032002000900002
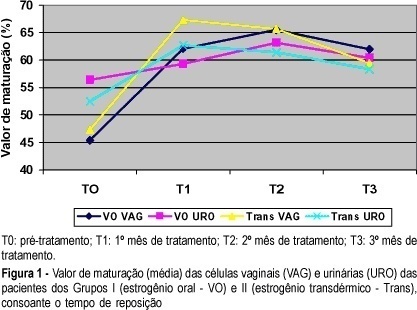
Objective: to study the effects of oral or transdermal estrogen replacement on the lower urinary tract and vagina in postmenopausal women. Methods: we studied 25 postmenopausal women evaluating the oral or transdermic estrogen replacement effects on the vaginal cells and urinary sediment during 3 months. The patients were randomly distributed into 2 groups: Group I, n = 14, treated orally with 0.625 mg equine conjugated estrogen plus 5 mg medroxyprogesterone acetate, daily for 3 months; Group II, n = 11, treated transdermally with 50 mug 17-ß-estradiol, once a week, plus 5 mg medroxyprogesterone. Daily, for 3 months, urinary samples were collected from the first miction in the morning after urogenital antisepsis into sterile tubes. The sample was centrifuged and the sediment was smeared. Vaginal and urinary smears were then fixed in absoluted alcohol and stained by the method of Shorr. Results: the patients who used the oral route presented maturation of the vaginal cells (from 45.4 to 65.5% after 2 months of treatment, maintaing 62% afterwards) but this did not occur with urinary cells (56.4 before treatment versus 60.4% at the end of the period). The transdermal route promoted maturation of vaginal and urinary cells. Conclusion: we have concluded that transdermal estrogens have satisfactory effects both on vaginal and urethral sites. However, with the oral route we did not find the expected results in the urinary tract in all cases.
Summary
Rev Bras Ginecol Obstet. 2022;44(6):578-585
It is known that the single embryo transfer (SET) is the best choice to reduce multiples and associated risks. The practice of cryopreserving all embryos for posterior transfer has been increasingly performed for in vitro fertilization (IVF) patients at the risk of ovarian hyperstimulation syndrome or preimplantation genetic testing for aneuploidy. However, its widespread practice is still controverse. The aim of this study was to evaluate how effective is the transfer of two sequential SET procedures compared with a double embryo transfer (DET) in freeze-only cycles.
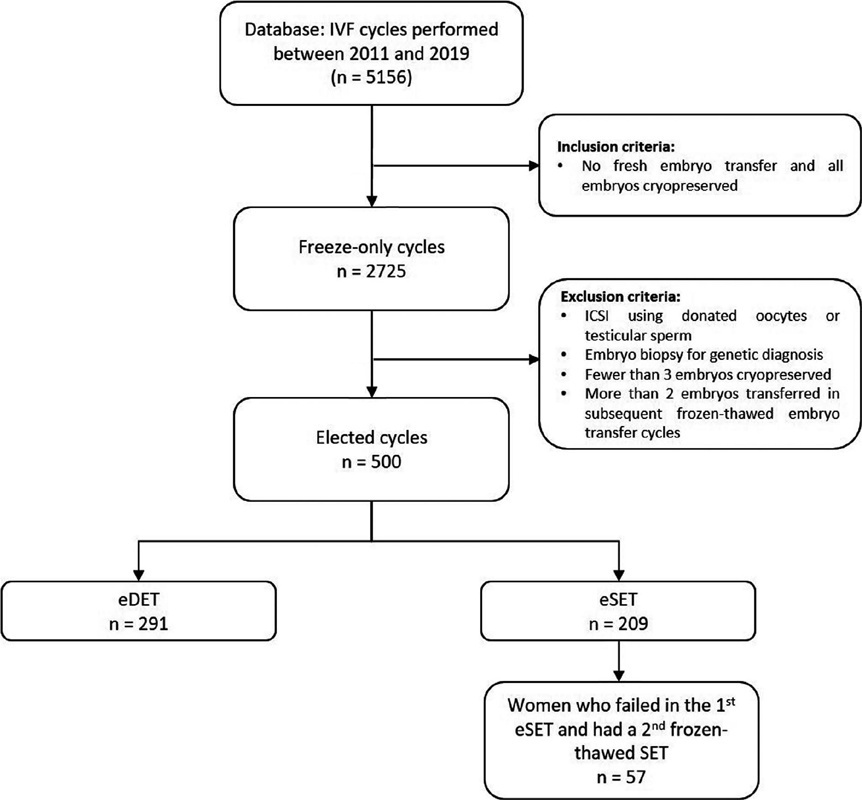
This retrospective study reviewed 5,156 IVF cycles performed between 2011 and 2019, and 506 cycles using own oocytes and freeze-only policy with subsequent elective frozen-thawed embryo transfers (eFET) were selected for this study. Cycles having elective SET (eSET, n = 209) comprised our study group and as control group we included cycles performed with elective DET (eDET, n = 291). In the eSET group, 57 couples who had failed in the 1st eSET had a 2nd eFET, and the estimated cumulative ongoing pregnancy rate was calculated and compared with eDET.
After the 1st eFET, the ongoing pregnancy rates were similar between groups (eSET: 35.4% versus eDET: 38.5%; p =0.497), but the estimated cumulative ongoing pregnancy rate after a 2nd eFET in the eSET group (eSET + SET) was significantly higher (48.8%) than in the eDET group (p < 0.001). Additionally, the eSET +SET group had a 2.7% rate of multiple gestations, which is significantly lower than the eDET group, with a 30.4% rate (p < 0.001).
Our study showed the association of freeze-only strategy with until up to two consecutive frozen-thawed eSETs resulted in higher success rates than a frozenthawed DET, while drastically reducing the rate of multiple pregnancies.
Summary
Rev Bras Ginecol Obstet. 2000;22(9):585-591
DOI 10.1590/S0100-72032000000900008
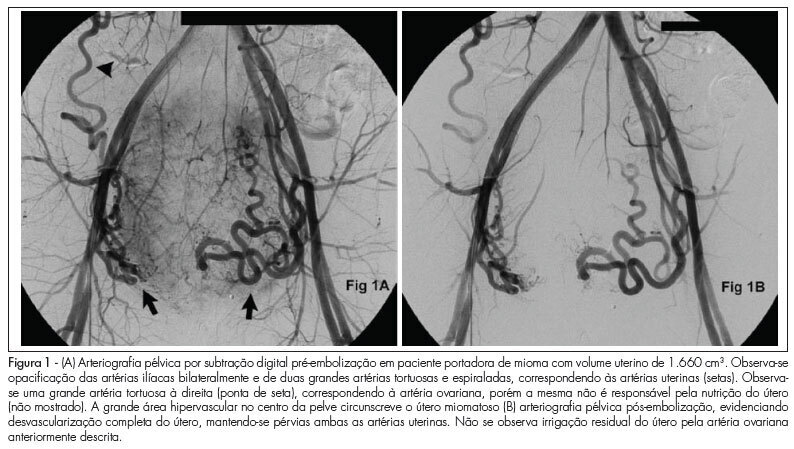
Purpose: to test the adrenal function by a potent stimulus to its reticular layer verifying 3beta-hydroxysteroid dehy-drogenase (3beta-HSD) and 21-hydroxylase (21OH) enzymatic activities. Methods: plasma concentrations of 17alphaOH-pregneno-lone, 17alphaOH-progesterone, cortisol, progesterone, androstenedione, dehydroepiandrosterone (DHEA), dehydroepiandrosterone sulfate (SDHEA) and free testosterone were determined in 39 women, 13 of whom were normal (2 of them used in a pilot study) and 26 had idiopathic hirsutism, 0, 12 and 24 h after injection of ACTH-depot. Results: among hirsute women, we identified different responses that could diagnose any blockage in the steroid pathways leading to the diagnosis of a mild/moderate decreased adrenal function. The 17alphaOH-pregnenolone concentrations varied from 2.0 to 24.6 ng/mL, cortisol values increased from 2.1 to 45.3 and 38.4 mug/dL, 17alphaOH-progesterone levels varied from 50.7 to 346 and 218 ng/mL and progesterone increased from 0.3 to 4.4 and 2.2 ng/mL. Among the reticular layer hormones a rise of SDHEA from 274.7 to 495.5 and 505.8 mg/dL, and of androsterone from 1.1 to 4.0 and 4.5 ng/mL was observed, the levels of free testosterone increased from 1.3 to 1.8 and 2.7 pg/mL and the DHEA levels from 2.4 to 4.7 and 8.5 ng/mL. One patient showed 3beta-HSD deficiency and two others a possible 21OH deficiency. Conclusions: these findings suggest that the ACTH-depot test could be used to exclude the adrenal gland as the possible source of hyperandrogenism in women with idiopathic hirsutism.