You searched for:"Sophie Françoise Mauricette Derchain"
We found (27) results for your search.Summary
Rev Bras Ginecol Obstet. 2002;24(7):447-452
DOI 10.1590/S0100-72032002000700004
Purpose: to compare the size of locally advanced breast tumors through clinical examination, mammography, and ultrasound, and describe the parameters of color Doppler ultrasound evaluated before and after primary chemotherapy. Methods: it was a prospective and descriptive clinical study. Eighteen women with the diagnosis of breast carcinoma, with clinical primary tumors of 50 mm or larger, were submitted to palpation, mammography, ultrasound and color Doppler ultrasound at the moment of diagnosis and after 3 cycles of chemotherapy. The response was considered present when there was a clinical decrease of 50% or more and an ultrasonographic decrease of 25% or more, and absent when there was a clinical decrease less than 50% and ultrasonographic decrease less than 25%. A descriptive statistical analysis and Wilcoxon test were used. Results: regarding the size of the tumors, the method whose results were closer to pathological examination was the clinical examination after chemotherapy, when compared with sizes on ultrasound and mammography. The mammography helped to evaluate 44% of the cases before chemotherapy (8/18). In the cases where the response was absent, the Doppler showed a significant increase of the flow and a decrease of resistance and pulsatility index. In the cases where the response was present (9 cases), the Doppler did not show any significant change regarding the studied parameters. Conclusion: clinical examination was the most efficient method to evaluate the decrease of the volume of tumors submitted to neoadjuvant chemotherapy when compared with ultrasound and mammographic examinations. Doppler showed increase of the flow in the cases of absent response.
Summary
Rev Bras Ginecol Obstet. 2004;26(6):457-462
DOI 10.1590/S0100-72032004000600006
OBJECTIVE: to assess the ability of Pap smear and hybrid capture II (HCII) to detect clinically significant cervical lesions (CIN2/3) in women referred to hospital due to atypical squamous cells of unknown significance (ASCUS) or low-grade squamous intraepithelial lesions (LSIL). METHODS: a cross-sectional study comprising 161 women referred to the Taubaté University Hospital due to ASCUS/LSIL, between August 2000 and September 2002. All women responded to a questionnaire regarding sociodemographic and reproductive characteristics and were subjected to gynecological examination with specimen collection for Pap test and HCII, along with colposcopy and eventual cervical biopsy. The relationship between HCII results and age, use of condom, oral hormonal contraception, and smoking were evaluated by the chi-square test. The sensitivity, specificity, positive and negative predictive values of both Pap test and HCII were calculated. All calculations were performed within 95% confidence intervals. RESULTS: sixty-seven percent of the women that tested positive for HPV were less than 30 years old. Pap smear and HCII showed the same 82% sensitivity in detecting CIN2/3 when the threshold for a positive Pap result was ASCUS, LSIL or HSIL. Pap smear specificity and positive predictive values were substantially increased when only HSIL results were considered as positive (from 29 to 95% and 12 to 50%, respectively). These figures were superior to those of HCII, but at the expense of an expressive loss of sensitivity (from 82% to 41%). CONCLUSIONS: our results substantiate the potential of HCII in detecting CIN2/3 among women referred due to ASCUS/LSIL.
Summary
Rev Bras Ginecol Obstet. 2009;31(9):461-467
DOI 10.1590/S0100-72032009000900007
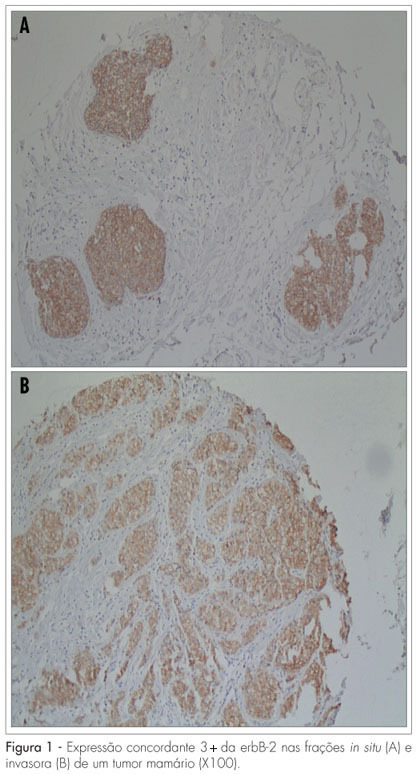
PURPOSE: to evaluate the expression of erbB-2 and of the estrogen and progesterone (ER/P) hormonal receptors in the transition regions between the in situ and the invasive fractions of ductal breast neoplasia (ISDC and IDC, respectively). METHODS: Eighty-five cases of breast neoplasia, containing contiguous ISDC and IDC areas, were selected. Histological specimens from the ISDC and the IDC areas were obtained through the tissue microarray (TMA) technique. The erbB-2 and the ER/PR expressions were evaluated through conventional immunohistochemistry. The McNemar's test was used for the comparative analysis of the expressions of erbB-2 protein and the ER/PR in the in situ and invasive regions of the tumors. The confidence intervals were set to 5% (p=0.05). Intraclass correlation coefficients (ICC) were calculated to assess the cross-tabulation agreement of the erbB-2 and the ER/PR expression in the ISDC and the IDC areas. RESULTS: the erbB-2 expression has not differed between the ISDC and the IDC areas (p=0.38). Comparing the two areas in each case, there was agreement in the expression of erbB-2 (ICC=0.64), PR (ICC=0.71) and ER (ICC=0.64). Restricting the analysis to tumors with the in situ component harboring necrosis (comedo), the ICC for erbB-2 was 0.4, compared to 0.6 for the whole sample. In this select group, the ICC for PR/ER did not differ substantially from those obtained with the complete dataset: as for the ER, ICC=0.7 (versus 0.7 for the entire sample) and for PR, ICC=0.7 (versus 0.6 for the entire sample). CONCLUSIONS: our findings suggest that the erbB-2 and the ER/PR expressions do not differ in the contiguous in situ and invasive components of breast ductal tumors.
Summary
Rev Bras Ginecol Obstet. 2005;27(9):534-540
DOI 10.1590/S0100-72032005000900006
PURPOSE: to evaluate the role of morphological (12) and Doppler velocimetry (17) ultrasonographic features, in the detection of lymph node metastases in breast cancer patients. METHODS: 179 women (181 axillary cavities) were included in the study from January to December 2004. The ultrasonographic examinations were performed with a real-time linear probe (Toshiba-Power Vision-6000 (model SSA-370A)). The morphological parameters were studied with a frequency of 7.5-12 MHz. A frequency of 5 MHz was used for the Doppler velocimetry parameters. Subsequently, the women were submitted to level I, II and III axillary dissection (158), or to the sentinel lymph node technique (23). Sensitivity, specificity, and positive and negative predictive values were calculated for each parameter. The decision tree test was used for parameter association. The cutoff points were established by the ROC curve. RESULTS: at least one lymph node was detected in 173 (96%) of the women by the ultrasonographic examinations. Histological examination detected lymph node metastases in 87 women (48%). The best sensitivity among the morphological paramenters was found with the volume (62%), the antero-posterior diameter (62%) and the fatty hilum placement (56%). Though the specificity of the extracapsular invasion (100%), border regularity (92%) and cortex echogenicity (99%) were high, the sensitivity of these features was too low. None of the Doppler velocimetry parameters reached 50% sensitivity. The decision tree test selected the ultrasonographic parametners: fatty hilum placement, border regularity and cortex echogenicity, as the best parameter association. CONCLUSION: the detection of axillary cavity lymph node stage by a noninvasive method still remains an unfulfilled goal in the treatment of patients with breast cancer.
Summary
Rev Bras Ginecol Obstet. 2007;29(11):580-587
DOI 10.1590/S0100-72032007001100006
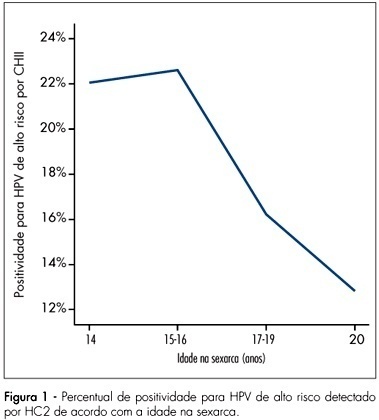
PURPOSE: to investigate women’s age at their first sexual intercourse and its correlation with their present age, human papillomavirus (HPV) infection and cytological abnormalities at Pap smear. METHODS: women from the general population were invited to be screened for cervical cancer and pre-malignant lesions. After answering a behavior questionnaire, they were submitted to screening with cervical cytology and high-risk HPV testing with Hybrid Capture 2 (HC2). This report is part of the Latin American Screening (LAMS) study, that comprises centers from Brazil and Argentina, and the data presented herein refer to the Brazilian women evaluated at the cities of Porto Alegre, São Paulo and Campinas. RESULTS: from 8,649 women that answered the questionnaire, 8,641 reported previous sexual activity and were included in this analysis. The mean age at the interview was 38.1±11.0 years and the mean age at the first sexual intercourse was 18.5±4.0 years. The age at the first sexual intercourse increased along with the age at the interview, i.e., younger women reported they had begun their sexual life earlier than older women (p<0.001). From the total of women who had already begun having sexual intercourse, 3,643 patients were tested for high-risk HPV infection and 17.3% of them had positive results. In all the centers, it became clear that the women with the first sexual intercourse at ages below the mean age of all the population interviewed presented higher rates of HPV infection (20.2%) than the women with the first sexual intercourse at ages above the mean (12.5%) - Odds Ratio (OR) 1.8 (IC95% 1.5-2.2;p<0,001). According to the cytology, the women with first sexual intercourse at ages under the mean, presented higher percentage of abnormal cytology > or = ASC-US (6.7%) than the women with the first sexual intercourse at ages above the mean (4.3%) - OR 1.6 (IC95% 1.3-2.;p<0.001). CONCLUSIONS: the high-risk HPV infection and cytological abnormalities identified during the asymptomatic population screening were significantly associated to the women’s age at the first sexual intercourse. Additionally, we have also identified that the women’s age at the first sexual intercourse has decreased during the last decades, suggesting an important contribution to the increase of HPV infection and the subsequent cervical lesions.
Summary
Rev Bras Ginecol Obstet. 2000;22(2):65-70
DOI 10.1590/S0100-72032000000200002
Purpose: to evaluate conization by the loop electrosurgical excision procedure (LEEP) for the diagnosis and treatment of cervical intraepithelial neoplasms (CIN), the importance of the margins and follow-up of these women. Methods: 95 women who underwent conization by LEEP for CIN and microinvasive carcinoma from January 1996 to December 1997 were evaluated. For statistical analysis, we used the kappa agreement coefficient and the tendency test of Cochran Armitage. Results: among 63 cases who underwent colposcopically directed biopsy before the conization, the cone presented the same grade of lesion in 20 and no residual disease in 8. The cone lesion presented a higher grade in 24 cases and one of them was a microinvasive carcinoma. Among the 25 women who underwent the cone biopsy with a previous biopsy suggestive of cervicitis or CIN 1, 56% had CIN 2 or 3 in the cone. Among the 32 women without previous biopsy, 15 had CIN 2 or 3, and four had microinvasive carcinoma in the cone. Regarding the margins of the cone, 25 cases presented some grade of CIN in the endocervical margins and 2/10 who underwent a second procedure presented residual disease on histological analysis. Among the 70 women with free cone margins, 2/4 who underwent a second procedure had residual disease on histological analysis. Conclusion: conization by LEEP without previous directed biopsy depends on the experience of the colposcopist. The second resection after LEEP for the diagnosis and treatment of CIN depends not only on the presence of disease in the cone margins but also on the follow-up. A second histological analysis is recommended in cases with microinvasive carcinoma and glandular lesion and affected margins.
Summary
Rev Bras Ginecol Obstet. 2019;41(12):710-717
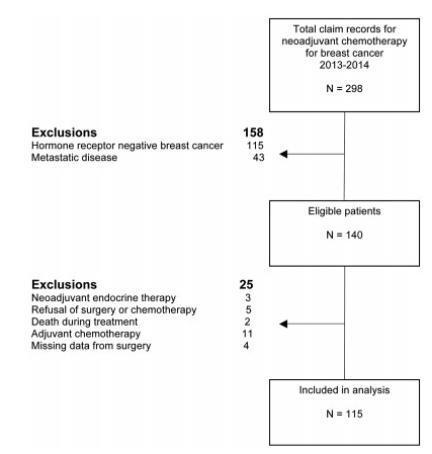
To identify the biomarkers of response to neoadjuvant chemotherapy in early luminal breast cancer.
A cross-sectional study that included all patients with early or locallyadvanced luminal breast cancer submitted to neoadjuvant chemotherapy between 2013 and 2014. Demographic, clinic and pathologic data were retrieved from patient records. The expressions of the estrogen receptor (ER), the progesterone receptor (PR), and Ki67 were analyzed by immunohistochemistry (IHC). The status of the human epidermal growth factor receptor 2 (HER2) was evaluated by IHC and fluorescent in situ hybridization (FISH). Independent predictors of clinic and pathologic response were evaluated by stepwise logistic regression models and receiver operating characteristic (ROC) curve analysis.
Out of 298 patients identified, 115 were included in the analysis. Clinical complete response (cCR) was observed in 43.4% of the patients (49/113), and pathologic complete response (pCR) was observed in 7.1% (8/115) of the patients. The independent predictors of cCR were premenopausal status (p < 0.001), low PR expression (≤ 50% versus > 50%; p = 0.048), and Ki67 expression ≥ 14% (versus < 14%; p = 0.01). Patients with cCR were more commonly submitted to breast conserving surgery (34.7% versus 7.8%; p < 0.001). Increasing cut-off points for Ki67 expression were associated with an increase in specificity and a decrease in sensitivity to identify patients with cCR.
Premenopausal status, lower PR expression and higher Ki67 expression were associated with a higher rate of cCR to neoadjuvant chemotherapy in luminal breast cancer.
Summary
Rev Bras Ginecol Obstet. 2004;26(9):721-725
DOI 10.1590/S0100-72032004000900008
PURPOSE: to analyze the association between bacterial vaginosis (BV), high-risk HPV DNA, and Pap smear abnormalities in women submitted to diathermic conization for the treatment of high-grade cervical intraepithelial neoplasia (CIN 2 or 3). METHODS: a descriptive clinical study with 81 women submitted to diathermic conization for the treatment of CIN 2 or 3. Initial Pap smear was performed by the time of the biopsy and was also used to verify the presence of BV. Prior to conization, samples for the detection of high-risk HPV DNA through hybrid capture II (HC II) were collected. A control visit was scheduled for four months after the conization to repeat these tests. Twenty-seven women were found to have BV and 54 were not. Statistical analysis comprised odds ratios (OR) to assess the correlations between BV and HPV detection before and after diathermic conization and cytological abnormalities. All analyses were performed with a 95% confidence interval (95% CI). RESULTS: high-risk HPV DNA detection before conization was identical in both groups (89%). After conization, HPV DNA detection decreased to 26 and 18% in the groups with and without BV, respectively (OR=1.5; 95% CI 0.5 to 4.6). In addition, 41% of the women with BV and 20% without BV showed Pap smear abnormalities (OR=2.7; 95% CI 1.0 to 7.4). Regarding these 22 women with Pap smear abnormalities approximately four months after the diathermic conization, 83% of the BV group tested positive for HPV DNA compared with 50% in the group without BV (OR=5.0; IC 95% 0.5 a 52.9). CONCLUSION: women with BV presented more Pap smear abnormalities after conization when compared to the women without BV, although this was not statistically significant. This association was not related to high-risk HPV DNA.