You searched for:"Marilza Vieira Cunha Rudge"
We found (33) results for your search.Summary
Rev Bras Ginecol Obstet. 2003;25(6):445-448
DOI 10.1590/S0100-72032003000600010
Development of preeclampsia/eclampsia prior to 20 weeks of pregnancy should raise the suspicion of hydatidiform mole. We report a case of complete hydatidiform mole (CHM) concurrent with eclampsia in a 20-year-old patient with vaginal bleeding, anemia, large uterine size, and ovary cysts associated with hypertension and proteinuria. Plasmatic b-hCG levels were high and there was abnormal thyroid function. The ultrasonographic findings were compatible with CHM. After uterine evacuation, the patient had headache and visual alterations, followed by tonic-clonic seizures, which ceased with the administration of 50% magnesium sulfate. At post-molar follow-up, a gestational trophoblastic tumor (GTT) was diagnosed and promptly treated with chemotherapy. Association between CHM and eclampsia requires immediate uterine evacuation and strict post-molar follow-up, due to increased risk of GTT development.
Summary
Rev Bras Ginecol Obstet. 2013;35(11):477-482
DOI 10.1590/S0100-72032013001100001
PURPOSE: To evaluate the methodological and statistical design evolution of the publications in the Brazilian Journal of Gynecology and Obstetrics (RBGO) from resolution 196/96. METHODS: A review of 133 articles published in 1999 (65) and 2009 (68) was performed by two independent reviewers with training in clinical epidemiology and methodology of scientific research. We included all original clinical articles, case and series reports and excluded editorials, letters to the editor, systematic reviews, experimental studies, opinion articles, besides abstracts of theses and dissertations. Characteristics related to the methodological quality of the studies were analyzed in each article using a checklist that evaluated two criteria: methodological aspects and statistical procedures. We used descriptive statistics and the χ2 test for comparison of the two years. RESULTS: There was a difference between 1999 and 2009 regarding the study and statistical design, with more accuracy in the procedures and the use of more robust tests between 1999 and 2009. CONCLUSIONS: In RBGO, we observed an evolution in the methods of published articles and a more in-depth use of the statistical analyses, with more sophisticated tests such as regression and multilevel analyses, which are essential techniques for the knowledge and planning of health interventions, leading to fewer interpretation errors.
Summary
Rev Bras Ginecol Obstet. 2007;29(10):506-510
DOI 10.1590/S0100-72032007001000003
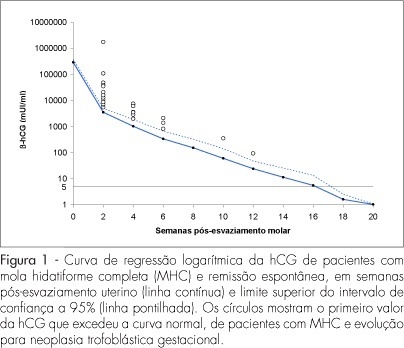
PURPOSE: to evaluate the usefulness of the normal human chorionic gonadotropin (hCG) regression curve in the early diagnosis of post-molar trophoblastic neoplasia (GTN). METHODS: a longitudinal study including 105 patients with complete hydatidiform mole (CHM) followed up at the Botucatu Center of Trophoblastic Diseases from 1998 to 2005. Serial serum hCG titers were measured fortnightly in all patients. Individual curves of the 105 patients were built. Comparison between the normal regression curve established at our center with individual hCG curves was used to screen and diagnose (plateau/rise) GTN. The number of weeks postevacuation when hCG levels exceeded the normal limits was compared with the number of weeks when hCG reached plateau/rise. RESULTS: among the 105 patients with CHM, 80 reached spontaneous remission (SR) and 25 developed GTN. Among the 80 SR patients, 7 (8.7%) initially showed hCG concentrations above normal but eventually achieved remission. All the 25 GTN patients showed deviation from the normal hCG curve at 3.84±2.57 weeks and reached plateau or rise at 8.40±2.94 weeks (p<0.001). CONCLUSIONS: the normal regression curve of post-molar hCG is useful in the early diagnosis of GTN.
Summary
Rev Bras Ginecol Obstet. 2003;25(1):53-59
DOI 10.1590/S0100-72032003000100008
PURPOSE: to study maternal (body composition and cardiovascular capacity) and perinatal (weight and prematurity) effects of hydrotherapy during pregnancy. METHODS: a prospective, random cohort study, with 41 low-risk pregnant women in their first pregnancy, practicing (study group, n=22) and not (control group, n=19) hydrotherapy. Anthropometric evaluation was used to assess lean mass, and absolute and relative body fat. Ergometric tests were used for maximum oxygen consumption (VO2max), stroke volume (SV) and cardiac output (CO). Perinatal results showed premature births and small for gestational age newborns. Initial and final indexes within and between groups were compared. Maternal variables were evaluated using the t test for dependent and independent values; the chi ² test was used to study proportions. RESULTS: there were no significant differences between the groups for maternal variables at the start and end of hydrotherapy. Comparison within each group confirmed the beneficial effect of hydrotherapy. In the study group, relative fat index was maintained at 29.0%; the control group showed an increase from 28.8% to 30.7%; the study group maintained VO2max at 35%, and increased SV from 106.6 to 121.5 and CO from 13.5 to 15.1; the control group showed a drop in VO2max and no change in SV and CO. There was no relationship between hydrotherapy and perinatal results. CONCLUSIONS: hydrotherapy adequately assisted metabolic and cardiovascular maternal adaptation to pregnancy and did not cause prematurity or weight loss in newborns.
Summary
Rev Bras Ginecol Obstet. 2000;22(9):567-572
DOI 10.1590/S0100-72032000000900005
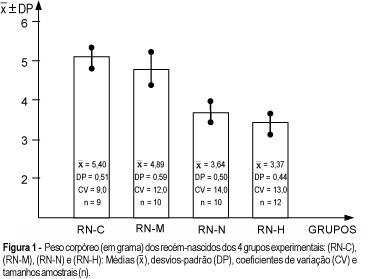
Purpose: to study the repercussion of arterial hypertension regarding body weight gain and body length, as well as liver and brain weight of offspring. Methods: a total of 82 animals in reproductive age were used. They were randomly assigned to 4 different groups (control, handled, nephrectomized and hypertensive). Renal hypertension was produced by a controlled constriction of the main left renal artery and contralateral nephrectomy, according to the technique described by Goldblatt (Goldblatt I: one kidney - one clip hypertension). Afterwards, they were distributed among nonpregnant and pregnant groups. The following newborn groups resulted from the pregnant groups: RN-C (control-newborn group of pregnant rats without surgical treatment), RN-M (manipulation-newborn group of the pregnant rats with surgical manipulation), RN-N (nephrectomized-newborn group of pregnant rats with nephrectomy) and Rn-H (hypertensive-newborn group of pregnant rats with hypertension). Results: the RN-N and RN-H groups showed body weight gain ( = 3,64 ± 0,50;
= 3,64 ± 0,50;  or = 3,37 ± 0,44), body length (
or = 3,37 ± 0,44), body length ( = 3,89 ± 0,36;
= 3,89 ± 0,36;  or = 3,68 ± 0,32) and brain weight (
or = 3,68 ± 0,32) and brain weight ( = 0,16 ± 0,01;
= 0,16 ± 0,01;  or = 0,16 ± 0,05), respectively, smaller than the control group (
or = 0,16 ± 0,05), respectively, smaller than the control group ( = 5,40 ± 0,51;
= 5,40 ± 0,51;  or = 4,95 ± 0,23 and
or = 4,95 ± 0,23 and  or = 0,22 ± 0,04, respectively). In addition, the RN-H group showed the lowest liver weight (
or = 0,22 ± 0,04, respectively). In addition, the RN-H group showed the lowest liver weight ( = 0,22 ± 0,03) compared with the other three groups. Conclusion: after statistical analysis, the results obtained showed that the arterial hypertension determined a reduction in body weight, body length, and liver and brain weight of the offspring.
= 0,22 ± 0,03) compared with the other three groups. Conclusion: after statistical analysis, the results obtained showed that the arterial hypertension determined a reduction in body weight, body length, and liver and brain weight of the offspring.
Summary
Rev Bras Ginecol Obstet. 2006;28(10):571-574
Summary
Rev Bras Ginecol Obstet. 2005;27(10):580-587
DOI 10.1590/S0100-72032005001000003
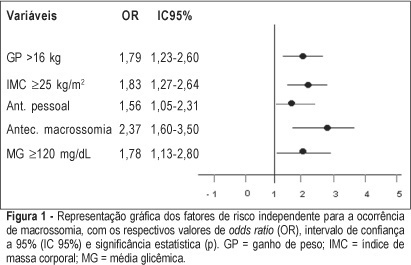
PURPOSE: to identify risk factors for fetal macrosomia in pregnant women with diabetes or daily hyperglycemia. METHODS: retrospective study, control-case, including 803 pairs of mothers and newborns belonging to this specific population, divided into two groups - macrosomic (cases, n=242) and non-macrosomic (controls, n=561). Variables regarding age, parity, weight and body mass index (BMI), weight gain (WG), diabetes history, high blood pressure and tabagism, diabetes type and classification, and glycemic control indicators in the third trimester were compared. The means were evaluated by the F test and the categorized variables were submitted to univariate analysis using the chi² test. The significative results were included in the multiple regression model for the identification of macrosomia independent risk considering OR, 95% CI and p value. The statistical significance limit of 5% was established for all analyses. RESULTS: there was a significative association between macrosomia and WG >16 kg, BMI >25 kg/m², personal, obstetric and macrosomic history, classification in the Rudge groups (IB and IIA + IIB), glycemic mean (GM) >120 mg/dL and postprandial glycemic mean >130 mg/dL in the third trimester. In the multiple regression analysis, WG >16 kg (OR=1,79; 95% CI: 1,23-1.60), BMI >25 kg/m² (OR=1.83; 95% CI: 1.27-2.64), personal history of diabetes (OR=1.56; 95% CI: 1.05-2.31) and of macrosomia (OR=2.37; 95% CI: 1.60-3.50) and GM >120 mg/dL in the third trimester (OR=1.78; 95% CI: 1.13-2.80) confirmed to be independent risk factors for macrosomia in these pregnancies. CONCLUSION: WG >16 kg, BMI >25 kg/m², GM >120 mg/dL in the third trimester and personal history of macrosomia and diabetes were identified as risk factors for fetal macrosomia in pregnant women with diabetes or daily hyperglycemia.