You searched for:"José Guilherme Cecatti"
We found (51) results for your search.Summary
Rev Bras Ginecol Obstet. 2003;25(4):255-260
DOI 10.1590/S0100-72032003000400006
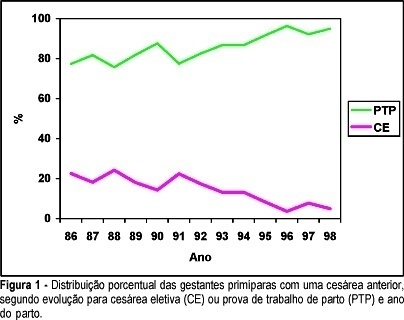
PURPOSE: to compare maternal morbidity, neonatal results and some clinical and epidemiological characteristics among primiparous women who had one previous cesarean section, according to the performance of elective cesarean (EC) section or trial of labor (TL) during the second delivery. PATIENTS AND METHODS: this is a retrospective cross-sectional study on the second delivery of women who previously had a cesarean section and were assisted at the Center for Integral Assistance to Women's Health (CAISM/UNICAMP), from 1986 to 1998. Data were collected from 2068 clinical records corresponding to 322 cases of EC and 1746 of TL. Data analysis was performed through percentage distribution of the EC and TL cases and also the distribution of variables between these two groups, using the chi2, chi2 for trend and Fisher exact tests to evaluate the statistical difference, with a significance level of 95%. RESULTS: the indication of EC decreased progressively with time, from 22.6% in 1986 to 5% in 1998. Maternal morbity was similar and low in both groups (1.24% and 1.21%). There was no significant difference between groups regarding Apgar score and stillbirths, but there was a significantly higher proportion of premature newborns and with birth weight below 2.500 g and above 4.000 g in the group who underwent EC. The prevalence of EC was significantly higher in women 35 or more years old, with previous or current history of hypertensive disorder, diabetes or with a first dead child, as well as with changes in the volume of amniotic fluid. CONCLUSIONS: performing TL progressively increased during this period of thirteen years, without any increase of maternal and/or neonatal morbidity. The indication for EC followed medical criteria related to unfavorable maternal and/or fetal clinical conditions for vaginal delivery.
Summary
Rev Bras Ginecol Obstet. 2000;22(1):27-32
DOI 10.1590/S0100-72032000000100005
Purpose: to identify and quantify the underreporting of maternal mortality, from death certificates (DC) in Campinas, São Paulo, from 1992 to 1994. Methods: a total of 216 DC whose causes of death were maternal (declared and/or presumed) were selected among the 1032 DC of 10 to 49-year-old women. A complementary investigation was performed on hospital records, at the death verifying units, and in households. Results: eight additional maternal deaths were identified among the 204 DC with presumed maternal death. This corresponded to an underreporting rate of 40% or to a correction factor of 1.67 for the official MMR. The first cause of underreporting was abortion (71.5% or 05/07) and indirect maternal deaths represented the second cause (66.6% or 02/03). Conclusions: the death certificate cannot be considered the only source to identify maternal death. Complementary investigation of the presumable causes of maternal death should be performed. Legislation, social and religious factors might influence the underreporting of abortion as the cause of maternal death.
Summary
Rev Bras Ginecol Obstet. 2006;28(1):3-9
DOI 10.1590/S0100-72032006000100002
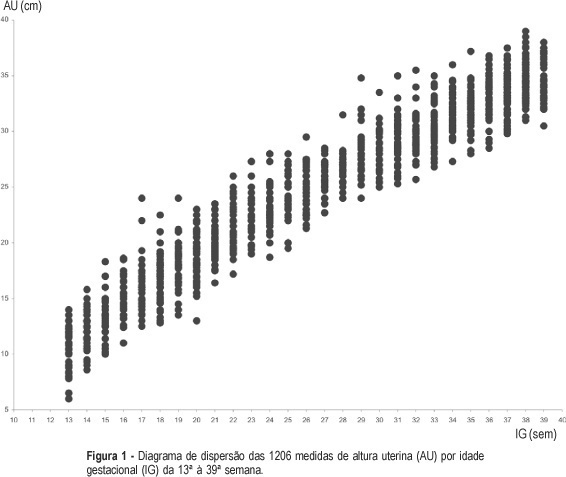
PURPOSE: to build a curve of fundal height according to gestational age among low-risk pregnant women and to compare it with the official standards used in Brazil. METHODS: a prospective observational study was carried out. A sample of 227 low-risk pregnant women with gestational age from 13 to 39 weeks was followed-up in the prenatal care sector of two public health services from João Pessoa, PB. Women with a known gestational age, a single live fetus, without malformation, with no known maternal-fetal pathological condition that could possibly affect fetal growth, with a normal body weight, and non-smokers were included in the study. Their fundal height was measured in a standard way, after a previous ultrasound done to confirm the gestational age. The same investigator performed 1206 measurements and each woman had a mean of 5.3 measurements. Statistical tests were performed with a significance level of 5%. Tables and graphs of fundal height were built according to the gestational age with the 10th, 50th and 90th percentiles. RESULTS: the values of percentiles 10, 50 and 90 of fundal height in each gestational age allowed the construction of a pattern curve of fundal height by gestational age among low-risk pregnant women. A clear visual difference was observed between this new and the official fundal height curve. Statistical analyses showed significant differences between them from the 19th week on. CONCLUSION: the results suggest different normal fundal height and fetal growth patterns among low-risk pregnant women on prenatal assistance compared to the used standard curve, thus with different performances when used for diagnosing fetal growth deviations. Future studies should validate the current fundal height curve by gestational age in order to possibly use it as a reference pattern.
Summary
Rev Bras Ginecol Obstet. 2006;28(5):310-315
DOI 10.1590/S0100-72032006000500008
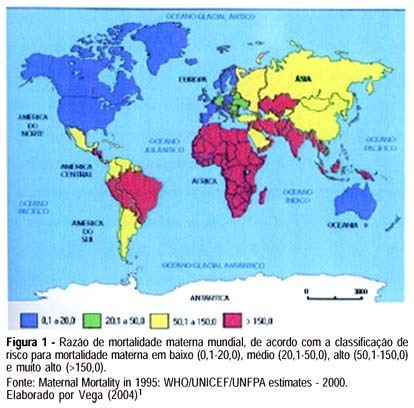
Maternal mortality rate (MM) is a health quality indicator that is directly influenced by the economic, cultural and technological level of a country. Official data of MM in Brazil, although underestimated, point to the lack of quality in pregnancy, childbirth and puerperium care services. This characteristic is common in developing countries, where poorer pregnant women as well as those facing greater difficulty to quality care access are found. Prenatal care cannot prevent major childbirth complications, which are important causes of MM; however, some interventions during the prenatal period can favor maternal prognosis and prevent MM. In this setting, this study brings a scientifically based update concerning effective interventions for maternal mortality prevention during the prenatal period. The most important strategies consist of a tripod with specific interventions related to maternal health promotion, risk prevention and assurance of nutritional support during gestation, in addition to criteria to investigate gestational risk and inclusion of the pregnant woman in the basic component of the prenatal care model. It ends with the definition of priorities in the prevention of MM related to eclampsia/preeclampsia and reinforces the importance of normalization of reference systems for obstetric emergency cases.
Summary
Rev Bras Ginecol Obstet. 1998;20(6):325-331
DOI 10.1590/S0100-72031998000600005
The purpose of the present study was to evaluate the efficacy and safety of the association bupivacaine with sufentanil for labor and delivery analgesia through a continuous epidural blockade, for both mother and the neonate. A randomized double blind prospective clinical trial was performed including sixty nulliparous women at the Maternity of CAISM/UNICAMP. When requesting analgesia, the women were randomly allocated to two groups: BS, receiving 12.5 mg of bupivacaine with adrenaline plus 30 µg of sufentanil and BP, receiving 12.5 mg of bupivacaine with adrenaline plus placebo. The parameters concerning the quality and duration of analgesia, duration of labor, and also possible effects on the neonate were evaluated. The results showed the superiority of the addition of sufentanil regarding the degree of analgesia during the time of action of the first dose of the local anesthetic. There was no increase in the duration of labor after the onset of analgesia when comparing both groups, nor any difference in the route of delivery. Concerning neonate evaluation, there were no differences between the two groups. It is concluded that the association of 30 µg of sufentanil with the first dose of bupivacaine is safe and efficacious. It improved the quality of analgesia, increased its duration, and did not affect the progress of labor and neonatal outcome.
Summary
Rev Bras Ginecol Obstet. 2003;25(1):35-40
DOI 10.1590/S0100-72032003000100006
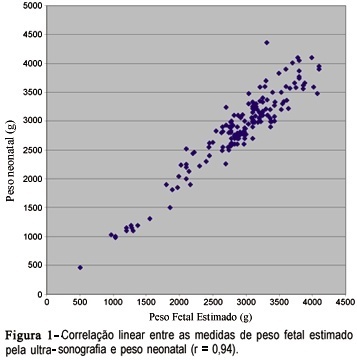
PURPOSE: tocompare the ultrasound estimation of fetal weight (EFW) with neonatal weight and to evaluate the performance of the normal EFW curve according to gestational age for the diagnosis of fetal/neonatal weight deviation and associated factors. METHODS: one hundred and eighty-six pregnant women who delivered at the institution from November 1998 to January 2000 and who had one ultra-sonographic evaluation performed until three days prior to delivery with estimation of the amniotic fluid index were included. EFW was calculated and classified in to small for gestational age (SGA), adequate for gestational age (AGA) and large for gestational age (LGA) through the normal EFW curve for this population. Neonatal weight was similarly classified. The variability of the measures and the degree of linear correlation between EFW and neonatal weight, as well as sensitivity, specificity and predictive values for the use of the normal EFW curve in the diagnosis of neonatal weight deviations were calculated. RESULTS: the difference between EFW and neonatal weight ranged from -540 to +594 g, with a mean of +46.9 g, and the two measures presented a linear correlation coefficient of 0.94. The normal EFW curve had a sensitivity of 100% and specificity of 90.5% in detecting SGA neonates and of 94.4 and 92.8%, respectively, in detecting LGA; however, the predictive positive values were low for both conditions. CONCLUSIONS:ultrasound EFW was in agreement with the neonatal weight, with a mean overweight of approximately 47 g, and its normal curve showed a good performance in the screening of SGA and LGA neonates.
Summary
Rev Bras Ginecol Obstet. 2005;27(6):357-365
DOI 10.1590/S0100-72032005000600011
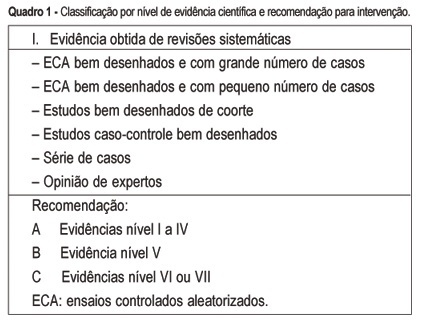
The multiple factors involved in maternal complications and maternal mortality make the task of their long-term control difficult and time-consuming. Professional care for pregnant women and/or those in labor certainly represents a key point for obtaining good outcomes, either maternal or perinatal. From the starting point that an adequate professional medical care for delivery has the capacity of decreasing the occurrence of complications associated with maternal morbidity and mortality, the evidence regarding some interventions included in this care is summarily presented. The evidence derived from studies performed with a strong methodological and scientific approach, mainly randomized controlled trials, on interventions to reduce complications and maternal mortality. These main interventions basically refer to: institutional care to is focused delivery, skilled professional care, use of traditional birth attendants in some contexts, use of appropriate technologies including partograph, place of birth, position for delivery, use of episiotomy, type of delivery, use of oxytocin during the active phase of labor, performance of push efforts during the second stage, active management of the third stage, and prophylaxis for post-partum hemorrhage. Although the effect of avoiding maternal death is difficult to be evaluated due to its low frequency, its rational and standardized use, through manuals and guidelines for intervention care, has a positive effect on the quality of care for childbirth. This is part of the human and technical context of the right that every woman has to the best possible care in this so special moment of her life.
Summary
Rev Bras Ginecol Obstet. 2019;41(6):379-386
Several factors might affect the health and the quality of life of women who had a severe maternal morbidity (SMM) or a maternal near-miss (MNM) episode. The objective of the present study was to explore the perspectives of the professionals on the repercussions of SMM or of MNM after interviewing women who survived such episodes.
Selected cases that captured the attention of professionals were reported. The professionals built individually 10 narratives, which were analyzed with the technique of content analysis.
According to the perspectives of the professionals, women surviving a severe maternal condition and their families experienced clinical and psychosocial consequences. Some cases portrayed the intense psychological distress in mourning for the loss of the fetus or of their reproductive capacity and changes in family dynamics generating emotional overload, depression, and gender violence.
The analysis of narratives may offer an idea on the complexity of the perception of care by professionals and on the need for an interdisciplinary follow-up of women surviving an SMM or an MNM episode.