You searched for:"Sophie Françoise Mauricette Derchain"
We found (27) results for your search.Summary
Rev Bras Ginecol Obstet. 2002;24(5):315-320
DOI 10.1590/S0100-72032002000500005
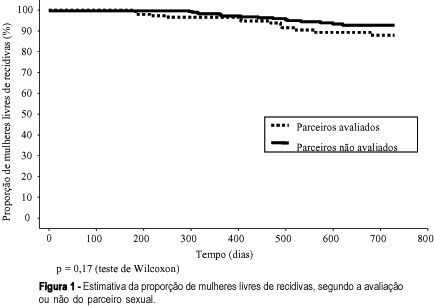
Purpose: to study the association between the evaluation or not of the male partner and relapses in women treated for HPV lesions. Methods: a reconstituted cohort study with 144 women with HPV lesions and whose partners had been evaluated, compared with 288 women whose partners had not been examined, controlled regarding date of attendance, age, lesion degree and treatment, attended between July 1993 and March 2000. We evaluated similarity between the groups, the association between the evaluation or not of the partners or the diagnosis of lesions with the occurrence and relapse lesion degree in the women and the disease-free interval (DFI). Results: the groups were similar regarding the control variables. Relapses occurred in 9.0 % of the women whose partners had been evaluated and in 5.9% of those whose partners had not been evaluated (p=0.23). When lesions were diagnosed in the men, 12.5% of their partners had relapses, against 7.3% of the women whose partners had no lesions (p=0.23), but there was no correlation with the relapse lesion degree and DFI. When the men reported a time of monogamous conjugal relationship <12 months, we observed 14.9% relapses in women, against 6.2% for the women whose partners reported a longer time (p=0.08). Conclusions: evaluation of the man did not decrease the relapse risk of HPV lesions in his partner. The presence of lesions in the male partners did not correlate with the occurrence and relapse degree in women and DFI. This study does not support the hypothesis that nonevaluated men would be an important cause of relapses in their partners.
Summary
Rev Bras Ginecol Obstet. 2010;32(7):315-320
DOI 10.1590/S0100-72032010000700002
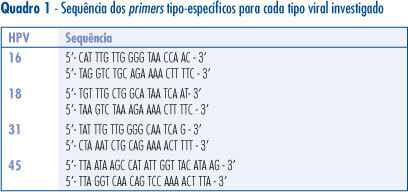
PURPOSE: to determine the prevalence of HPV 16, 18, 31 and 45 in cervical screening samples of women with cellular changes and/or colposcopy suggestive of persistent high grade or low grade lesion who were submitted to conization. METHODS: a total of 120 women were included in the study. Histological analysis of the cervical cones revealed 7 cases of cervicitis, 22 of CIN1, 31 of CIN2, 54 of CIN3, and 6 invasive carcinomas. The cervical screening samples were analyzed before conization for the presence of HPV-DNA by PCR using the consensus primers PGMY09/11. HPV-DNA-positive samples were tested for the presence of HPV16, 18, 31 and 45 using type-specific primers for these HPV. RESULTS: HPV-DNA was detected in 67.5% of the studied women. HPV 16 (40%) was the most prevalent type in most ilesions, followed by HPV 31 (13.3%), 45 (13.3%), and 18 (4.1%). Multiple infections occurred in 15% of the cases and infections with other HPV types were detected in 14% of the sample. CONCLUSIONS: HPV 16 and 18 infections do not always occur as a single infection, and may be associated with other HPV types on different occasions.
Summary
Rev Bras Ginecol Obstet. 2003;25(5):365-370
DOI 10.1590/S0100-72032003000500010
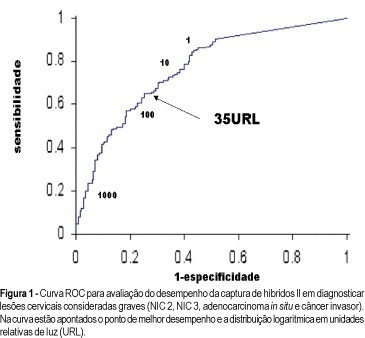
PURPOSE: to assess the performance of hybrid capture II (HCII) HPV viral load in predicting the grade of cervical lesions. METHODS: between August 2000 to November 2002, 309 women admitted due to an abnormal Pap smear result were recruited. Histological disease confirmation was done in all women and cervical intraepithelial neoplasia (CIN) grade 2 or above was considered as severe disease. HCII was done for high-risk HPV types and viral load was estimated in relative light units (RLU). Receiver operating characteristics analysis was used to test the performance of HCII. RESULTS: histological findings included 140 (45.3%) cervicitis or CIN 1 and 199 (54.7%) CIN 2/3, in situ adenocarcinoma or invasive cancer. The best cutoff for HCII in detecting severe disease was 35 RLU, showing a sensitivity of 69% and a specificity of 70%. Association of high-grade cervical lesions at Pap smear and HCII at 35 RLU showed a positive predictive value of 88.2% in diagnosis of CIN 2 or above. On the other hand, 95.7% of the women with low grade lesion at cytology and HCII below 1 RLU presented no severe histological disease. CONCLUSIONS: the best performance of HCII in diagnosing CIN 2 or above was found at 35 RLU. Association of cytology and HCII in different settings provided very high positive and negative predictive values.
Summary
Rev Bras Ginecol Obstet. 2002;24(1):37-43
DOI 10.1590/S0100-72032002000100006
Purpose: to determine the factors associated with the detection of a microinvasive carcinoma in the cervical cone of women with a previous colposcopically directed biopsy compatible with cervical intraepithelial neoplasia (CIN) 3 and to evaluate the proportion of involved margins. Patients and methods: we reviewed the medical records of 385 women (mean age: 39 years) submitted to cold conization or conization by high frequency surgery (HFS) with a loop during the period from January 1993 to July 2000. These procedures were indicated on the basis of a biopsy compatible with (CIN) 3. Results: the diagnosis of the cone was compatible with (CIN) 3 in 243 (63%) women and with (CIN) 2 in 13 (3%). Only 10 presented HPV/CIN 1 (3%) and eight had no residual disease in the cone. However, 101 (26%) women presented a microinvasive carcinoma in the cone and 10 (3%) presented a frankly invasive carcinoma. Age, menstrual status and number of deliveries were not related to the severity of the cone lesion. Women with oncologic colpocytology changes suggestive of invasion presented a significantly higher risk of having a microinvasive or invasive carcinoma as determined by final histology (p<0.01), although 52 of the 243 women with CIN 2 or CIN 3 in the cone also showed a suggestion of invasion at colpocytology. Among the women with CIN 2 or 3, the epithelium was white in 44%, dotted in 21%, and mosaic-like in 17%. This proportion was similar for women with a microinvasive or invasive carcinoma, with these images being detected in 37%, 23% and 21% of the cases, respectively. Involvement of the cone margins was significantly higher among women submitted to HFS (49%) than among those submitted to cold conization (29%). Conclusion: the absence of independent clinical and colposcopic factors associated with the detection of a microinvasive carcinoma in women submitted to conization on the basis of a biopsy compatible with (CIN) 3 justifies the conical excision of the squamocolumnar junction in high grade cervical lesions.
Summary
Rev Bras Ginecol Obstet. 2019;41(6):394-399
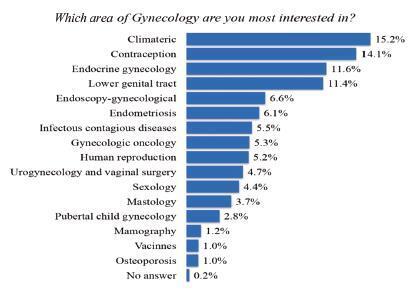
The present study aims to obtain basic demographic information, the level of interest and of training in gynecology oncology among Brazilian obstetricians and gynecologists (OB-GYNs) to create a professional profile.
An online questionnaire was sent to 16,008 gynecologists affiliated to the Brazilian Federation of Associations of Gynecology and Obstetrics (FEBRASGO, in the Portuguese acronym). We considered gynecologists dedicated to gynecologic oncology (OB-GYNs ONCO) those who self-reported that > 50% of their daily practice consists in working with women’s cancer care.
A total of 1,608 (10%) of 16,008 FEBRASGO members responded. The OBGYNs are concentrated in the southern and southeastern states of Brazil. Gynecologic oncology was considered the 8th greatest area of interest in gynecology among the OBGYNs. A total of 95 (5.9%) of the OB-GYNs were considered OB-GYNs ONCO. Obstetricians and gynecologists are actively engaged in cancer care: > 60% of them dedicate up to 25% of their daily practice to oncology. The role of the physicians in screening and prevention, diagnosis, in the treatment of precancerous lesions, and in low complexity surgical procedures is notably high. Gynecologists dedicated to gynecologic oncology in Brazil have a heterogeneous, nonstandardized and short training period in gynecologic oncology. These professionals had a more significantly role in performing medium- and high-complexity operations compared with OB-GYNs (65.2% versus 34%, and 47.3% versus 8.4%, respectively).
The role of OB-GYNs and of OB-GYNs ONCO appears to be complementary. Obstetricians and gynecologists actmore often in screening and prevention and in low-complexity surgical procedures, whereas OB-GYNs ONCO are more involved in highly complex cases. Strategies to raise standards in cancer training and to encourage the recognition of gynecologic oncology as a subspecialty should be adopted in Brazil.
Summary
Rev Bras Ginecol Obstet. 2005;27(7):425-433
DOI 10.1590/S0100-72032005000700010
Cervical cancer is nowadays a disease amenable to secondary prevention. Methods for the detection of its precursor lesions and human papillomavirus infection, such as cervical cytology and molecular biology, achieved widespread use worldwide. However, there is still too much controversy regarding the use of these methods in gynecological practice. Which is the best examination or the best association of examinations, and the most adequate time intervals to proceed with screening, are still pending questions, generating anxiety in patients and doctors. On the other hand, the management of women who have been diagnosed with viral infection and/or cervical intraepithelial neoplasia is not yet consensual, and several factors may affect the clinical decision on how to treat them. Therapeutic options are dependent upon the type of viral infection, severity of the cervical intraepithelial neoplasia and its histological type. The aim of the present article was to review the several aspects of cervical cancer screening and its viable treatment.
Summary
Rev Bras Ginecol Obstet. 1999;21(8):431-437
DOI 10.1590/S0100-72031999000800002
Purpose: to evaluate risk factors and papillomavirus (HPV) associated lesions in male partners of women with genital intraepithelial neoplasia. Patients and Methods: three hundred and thirty-seven men were evaluated by urethral cytology, peniscopy, and biopsy, if necessary. We analyzed the results and the relations to age, educational level, smoking, contact time with the present partner, age at first intercourse, number of partners, previous sexually transmitted diseases (STD), circumcision, peniscopic findings, and female lesion grade. Results: peniscopy was positive in 144 (42,7%) and HPV infection was diagnosed in 105 (31,2%). Smoking, contact time with the present partner up to 6 months, and more than one previous sexual partner were associated with HPV lesions (p<0,05). The urethral cytology was suspect in 4,2% and smoking, positive peniscopy or biopsy and partners of women with high-grade lesion (p<0,05) were associated with the diagnosis. 72.1% of 229 biopsies were positive, independently of the peniscopic findings and women's lesion grade. Conclusions: HPV infection was diagnosed in 31.2% and was associated with smoking, contact time with the present partner up to 6 months and more than one previous sexual partner, but not with the female lesion grade, educationa level, previous STD, circumcision and peniscopic findings.
Summary
Rev Bras Ginecol Obstet. 2018;40(8):433-436