You searched for:"Rodrigo Aquino Castro"
We found (8) results for your search.Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(8):493-500
To examine women with pelvic floor dysfunction (PFDs) and identify factors associated with sexual activity (SA) status that impacts quality of life (QoL).
We conducted a cross-sectional study that includedwomen> 18 years old who presented with at least one PFD symptom (urinary incontinence [UI] and/or pelvic organ prolapse [POP]), in outpatient clinics specializing in urogynecology and PFD in Fortaleza, state of Ceará, Brazil, using a service evaluation form and QoL questionnaires.
The analysis of 659 women with PFD included 286 SA (43.4%) women and 373 non-sexually active (NSA) (56.6%) women, with a mean age of 54.7 (±12) years old. The results revealed that age (odds ratio [OR]= 1.07, 95% confidence interval [CI] 1.03-1.12) and post-menopausal status (OR= 2.28, 95% CI 1.08-4.8) were negatively associated with SA. Being married (OR= 0.43, 95% CI 0.21-0.88) was associated with SA. Pelvic organ prolapse (OR= 1.16, 95% CI 0.81-1.68) and UI (OR= 0.17, 95% CI 0.08-0.36) did not prevent SA. SF-36 Health Survey results indicated that only the domain functional capacity was significantly worse in NSA women (p= 0.012). Two King’s Health Questionnaire domains in NSA women, impact of UI (p= 0.005) and personal relationships (p< 0.001), were significantly associated factors. Data from the Prolapse Quality-of-life Questionnaire indicated that NSA women exhibited compromised QoL.
Postmenopausal status and age negatively affected SA. Being married facilitated SA. Presence of POP and UI did not affect SA. However, NSAwomen with POP exhibited compromised QoL.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):225-231
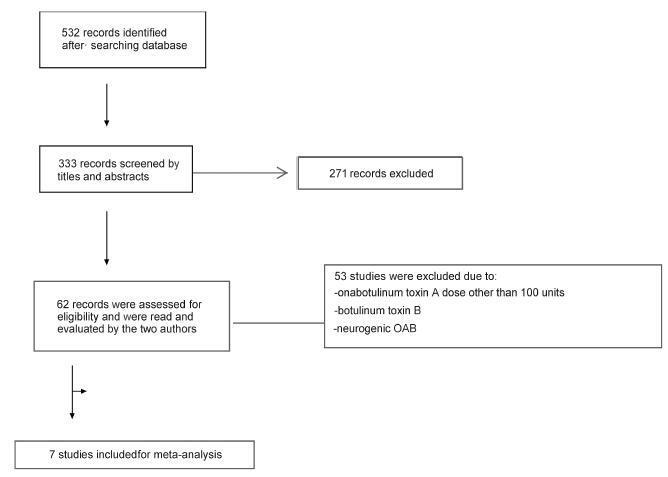
We performed a systematic review and meta-analysis of randomized placebo-controlled trials that studied non-neurogenic overactive bladder patients who were treated with 100 units of onabotulinumtoxinA or placebo. The primary purpose of our study was to evaluate the clinical effectiveness with regard to urinary urgency, urinary frequency, nocturia, and incontinence episodes. Our secondary purpose consisted of evaluating the adverse effects. Our initial search yielded 532 entries. Of these, seven studies met all the inclusion criteria (prospective, randomized, placebo-controlled studies, ≥ 3 points on the Jadad scale) and were selected for analysis. For all primary endpoints, the toxin was more effective than placebo (p < 0.0001; 95% confidence interval [95CI]), namely: urgency (mean difference = -2.07; 95CI = [-2.55-1.58]), voiding frequency (mean difference = - 1.64; 95CI = [-2.10-1.18]), nocturia (mean difference = -0.25; 95CI = [-0.39-0.11]) and incontinence episodes (mean difference = -2.06; 95CI= [-2.60-1.52]). The need for intermittent catheterization and the occurrence of urinary tract infection (UTI) were more frequent in patients treated with onabotulinumtoxinA than in patients treated with placebo (p < 0.0001). Compared with placebo, onabotulinumtoxinA had significantly and clinically relevant reductions in overactive bladder symptoms and is associated with higher incidence of intermittent catheterization and UTI.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):564-575
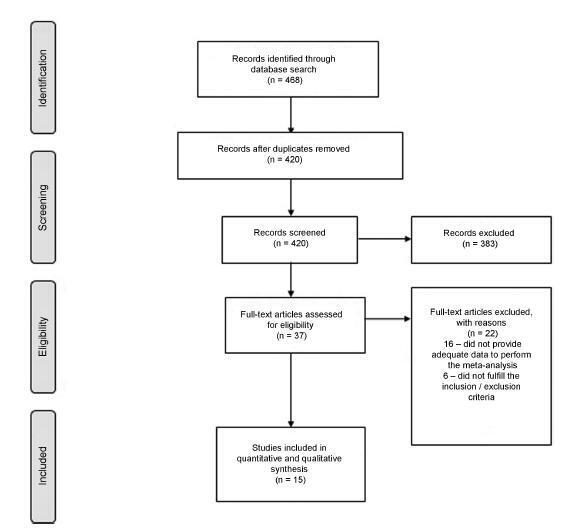
The overactive bladder (OAB) has a significant negative impact on the quality of life of patients. Antimuscarinics have become the pharmacological treatment of choice for this condition. The objective of this systematic review and meta-analysis is to examine the evidence from randomized clinical trials about the outcomes of the antimuscarinic drugs available in Brazil on OABs. We searched MEDLINE and the Cochrane Central Register of Controlled Trials from the inception of these databases through to September 2015. The primary outcome measures were the mean decrease in urge urinary incontinence episodes and the mean decrease in the frequency of micturition. The results suggest that there is a moderate to high amount of evidence supporting the benefit of using anticholinergic drugs in alleviating OAB symptoms when compared with placebo. It is still not clear whether any of the specific drugs that are available in Brazil offer advantages over the others. These drugs are associated with adverse effects (dry mouth and constipation), although they are not related to an increase in the number of withdrawals.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(11):505-510
DOI 10.1590/S0100-72032012001100005
PURPOSE: To investigate the effect of adding biofeedback (BF) to the training of pelvic floor muscles (PFMT) for the treatment of stress urinary incontinence (SUI). METHODS: A prospective pilot study, randomized and controlled with women with SUI without sphincter deficiency, detected by urodynamic study and who performed the correct PFM contraction. Women with neuromuscular disorders and grade III and IV genital prolapse were excluded. Forty women were randomized into a Control Group and BF Group. The PFMT protocol with BF equipment consisted of three sets of ten slow contractions (tonic), with a holding time of six to eight seconds at each contraction followed by a rest period of equal duration. After each sustained contraction, they performed three to four fast contractions (phasic) in the supine and standing position twice a week, for a total of 12 sessions. We evaluated the effect of adding BF to PFMT on quality of life using King's Health Questionnaire (KHQ) regarding urinary symptoms based on a voiding diary and regarding the function of pelvic floor muscles by digital palpation. The evaluation was performed initially and after 12 treatment sessions. Data are reported as mean and standard deviation. The Mann-Whitney test was used for the analysis of homogeneity and to determine differences between groups, and the Wilcoxon test was used to determine possible differences between the times of observation, with the level of significance set at 0.05. RESULTS: A significant decrease in the scores of the domains assessed by the KHQ was observed in the comparison between groups, except for the general health domain (BF Group: 32.8±26.9 versus Control Group: 48.4±29.5, p<0.13). Accordingly, there was improvement in PFM function after treatment in the BF Group, regarding power (4.3±0.8, p= 0.001), endurance (6.0±2.2, p<0.001) and fast (9.3±1.9, p=0.001). When comparing the groups, the BF Group showed a positive result regarding power (BF Group 4.3±0.8 versus Control Group 2.5±0.9, p<0.001), endurance (6.0±2.2 BF Group versus Control Group 2.7±1.9, p<0.001) and fast (BF Group 9.3±1.9 versus Control Group 4.6 ± 3.2, p<0.001). Reduction of nocturnal urinary frequency (1.2±1.2 versus 0.7±0.9, p=0.02) and of effort urine loss (1.5±1.4 versus 0.6±0.8, p=0.001) was observed in the BF Group. CONCLUSION: The addition of BF to the PFMT for the treatment of SUI, applied according to the protocol described, improved PFM function, reduced urinary symptoms, and improved of the quality of life.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(8):201-206
DOI 10.1590/S0100-72032011000800006
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(9):447-452
DOI 10.1590/S0100-72032009000900005
PURPOSE: to compare the effects of functional electrostimulation of the pelvic floor and therapy with cones in women with stress urinary incontinence (SUI). METHODS: randomized clinical study for which 45 patients with SUI were selected. The effects of functional electrostimulation of the pelvic floor were evaluated in the SUI treatment of 24 women, with the use of clinical data (micturition diary, pad test and a questionnaire about quality of life - I-QoL). The patients were submitted to two 20' weekly sessions for four consecutive months, under the supervision of a physiotherapist. The electrode used had 10 cm length and 3.5 cm width with a double metallic ring and a cylindrical shape, positioned in the medium third of the vagina. The electric parameters used were: intensity varying from 10 to 100 mA and 50 Hz of fixed frequency, with pulse duration of 1 ms. Also, we evaluated 21 patients who were submitted to vaginal cone treatment. The cone therapy was done with two 45 minute sessions per week. The cones' weight varied from 20 to 100 gr. RESULTS: there was no difference between the outcomes of electrostimulation of the pelvic floor and the vaginal cones for the treatment of SUI (p>0.05). After four months, there was a significant improvement in the I-QoL index of the patients treated both with electrostimulation (40.3 versus 82.9) or with the cones (47.7 versus 84.1). There was a significant decrease in pad weight in both groups, measured before and after the treatment (28.5 and 32 g versus 2.0 and 3.0 g for the electrostimulation and cone group, respectively). Finally, there was a significant decrease in the number of urinary leakage evaluated by the micturition diary in both groups (p<0.0001). CONCLUSIONS: both electrostimulation and vaginal cones were effective in the treatment of women with SUI.