You searched for:"Julisa Chamorro Lascasas Ribalta"
We found (11) results for your search.Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(1):26-31
A vulvar squamous intraepithelial lesion is deemed to be a preceding lesion to vulvar cancer, especially in women aged under 40 years, holders of an acquired or idiopathic immunosuppression. Several treatments have been used to treat these lesions. One of the aesthetically acceptable therapeutic methods is the CO2 laser vaporization.
In a transversal study, 46 records of immunosuppressed women bearing a vulvar low grade and/or high grade squamous intraepithelial lesion were selected out of the retrospective analysis, computing age, date of record, date of vulvar lesion treatment with CO2 laser, the time elapsed between the first and the last visit (in months), the number of visits, the presence or absence of condylomatous lesions in other female lower genital tract sites and whether or not recurrences and persistence of intraepithelial lesions have been noticed during the follow-up.
Patients bearing vulvar high-grade squamous intraepithelial lesion and immunosuppressed (serumpositive forhumanimmunodeficiency virus [HIV] or with solid organs transplantation) have shown a higher level of persistence of lesions and a higher chance of having other areas of the female lower genital tract involved.
While the CO2 laser vaporization is the most conservative method for the treatment of vulvar high-grade intraepithelial lesions, it is far frombeing the ideal method, dueto the intrinsic infection features considered. The possibility of persistence, recurrences and spontaneous limited regression indicates that a closer surveillance in the long-term treated cases should be considered, in special for immunosuppressed patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(12):726-730
DOI 10.1590/S0100-72032005001200004
PURPOSE: to study the influence of the use of oral contraceptives (OC) on the number of Langerhans' cells in women without cervical infection by human papillomavirus (HPV). METHODS: thirty women who presented abnormal cervical cytology and colposcopy-guided biopsy with samples of uterine cervix negative for HPV were selected. The absence of HPV DNA was confirmed by hybrid capture. Langerhans' cells were identified by immunohistochemistry using anti-S100 antigens. The cells visualized in light microscopy were counted using the Cytoviewer software. The nonparametric Wilcoxon rank sum test was employed for statistical analysis. RESULTS: the average number of Langerhans' cells in OC users was 320.7/mm² and in non-users 190.7/mm², this difference being statistically nonsignificant. In the intermediary layer of the cervical epithelium a tendency towards the increase of these cells was observed, with the averages 192.1/mm² for OC users and 93.4/mm² for non-users (p=0.05). CONCLUSIONS: the present study reports a tendency towards the increase in the number of the Langerhans' cells among OC users. This result suggests the OC may induce alterations in the number of Langerhans' cells, but considering the limited number of cases, more studies should be developed for a definitive conclusion.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(4):289-294
DOI 10.1590/S0100-72032004000400004
OBJECTIVE: to study the relationship of biobehavioral factors, such as age, menarche, number of gestations, and age of first sexual intercourse, with changes in Langerhans'cells in women with negative hybrid capture for HPV. METHODS: thirty women referred due to abnormal cervical cytology or premalignant cervical lesions were studied and underwent colposcopy, guided biopsy and histopathological exams. The Langerhans' cells were identified by immunohistochemical (S100+) exams. Langerhans' cells visualized in brown color were counted using the software Cytoviewer. The nonparametric Wilcoxon rank-sum test was employed for statistical analysis. RESULTS: the number of Langerhans' cells in women who had menarche after 13 years old presented statistically significant difference (173.34 cell/mm²) compared to the group whose menarche occurred before 13 (271.41 cell/mm²). The age at the first sexual intercourse was associated with the low number of Langerhans' cells, 127.15 cell/mm² and 250.14 cell/mm², respectively, for the beginning of the sexual activity up to 17 years old and after 17 (p=0.03). Previous cauterizations of the uterine cervix have been related to a lower number of Langerhans' cells in the epithelium, with the average 120.30 cell/mm² as compared to 236.06 cell/mm² for those women who never underwent that procedure (p=0.05). Other factors such as the patient's age and the number of gestations showed no statistically significant differences in the density of Langerhans' cells. CONCLUSIONS: the present study reports the association of biobehavioral factors with decrease in the number of Langerhans' cell.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(3):213-219
DOI 10.1590/S0100-72032004000300007
OBJECTIVE: to evaluate the effectiveness of the hygroscopic dilator in the colposcopic examination of the endocervical canal in patients with high-grade lesion in the cytopathology and unsatisfactory colposcopy. METHODS: prospective study, including 62 patients with unsatisfactory colposcopic examination and cytology compatible with high-grade intraepithelial lesion. The patients were submitted to dilation of the endocervical canal by means of a hygroscopic dilator. After dilation, the new colposcopic findings were recorded, and then conization was made through loop electrosurgical excision procedure. The incidence of neoplasic involvement of surgical margins was compared between patients with examinations modified toward satisfactory results and those that remained with unsatisfactory colposcopy. In order to compare the incidence of involved margins and the incidence of residual disease, two retrospective control-groups were used: the GinSat group (n = 35): patients with unsatisfactory colposcopy; GSat group (n = 38): patients with satisfactory colposcopy and endocervical atypy. RESULTS: 80.6% of the cases presented satisfactory colposcopic vision after dilation. 80.4% of those presented disease-free resection margins. The incidence of disease-free resection margins in patients with persistent unsatisfactory colposcopy after dilation was 36.3%. Affected surgical margins occurred in 28% of the group that had undergone dilation, 28.5% of the cases in GinSat group, and 31.5% in the Gsat group. Follow-up showed the incidence of residual disease in 7.5% of the patients under dilation, 28.5% in the GinSat group and 28.9% in the GSat group. CONCLUSION: the use of hygroscopic dilation improved visualization of lesions of difficult access to the colposcopic examination, thus permitting reduction in the percentage of residual neoplasic disease in patients with unsatisfactory colposcopy treated with loop electrosurgical excision procedure.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(2):97-102
DOI 10.1590/S0100-72032004000200003
PURPOSE: to correlate the type of cervical lesion diagnosed by Pap smear with CD4 cell counts and HIV-RNA viral load in HIV-positive patients. METHODS: one hundred and fifteen HIV patients were evaluated retrospectively in the present study, during the period from January 2002 to April 2003, at a university hospital. Eighty-three patients presented cervical intraepithelial neoplasia (CIN) in Pap smear, in comparison with thirty-two with no lesions. Patients were divided into three groups, according to CD4 counts: CD4 more than 500 cells/mm³, between 200 and 500 cells/mm³, and less than 200 cells/mm³, and other three groups, according to HIV viral load: less than 10,000 HIV-RNA copies/mL, between 10,000 and 100,000 HIV-RNA copies/mL, or more than 100,000 HIV-RNA copies/mL. Correlation was investigated by the Fisher test. RESULTS: of the eighty-three patients with CIN, 73% presented CD4 counts less than 500 cells/mm³. In all CD4 groups, more than 50% of the patients presented CIN. According to the viral load, 71.7% of the patients with less than 10,000 HIV-RNA copies/mL presented CIN I, compared with 11.3% that showed CIN III. In the group with higher viral load (>100.000 HIV-RNA copies/mL), 61.5% showed CIN I and 30.8% presented CIN III. CONCLUSION: association between viral load and CIN was established (p=0.013), which was not observed with CD4 cell counts and CIN. Concomitant cervicovaginal infection was considered a potential confounding factor.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(6):339-345
DOI 10.1590/S0100-72032000000600004
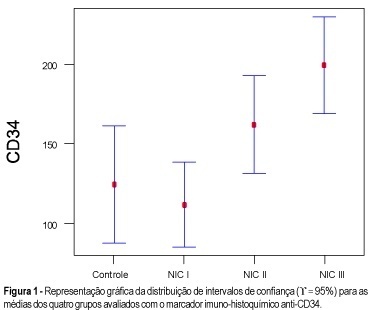
Purpose: to quantify the vessels and epithelial proliferation, applying immunohistochemical staining with anti-CD34 as well as anti-PCNA markers, in intra-epithelial neoplasia of the uterine cervix. Methods: in the present study, 16 patients with CIN III, 16 with CIN II, 21 with CIN I and 11 with normal cervix (control group) were investigated. Slide analysis was performed at the same time by two observers, in 10 consecutive sites using 100X and 400X magnification, both in the highest vascularization (CD34) and proliferative activity sites (PCNA). Results: the means obtained with the use of anti-PCNA in intraepithelial neoplasias were: 78.2% (CIN III), 52.1% (CIN II), 33.3% (CIN I) and 4.6% (control group), while 199.1 vessels (CIN III), 162.0 vessels (CIN II), 111.7 vessels (CIN I) and 124.4 vessels (control group) were quantified using anti-CD34 as a vascular marker. Conclusion: the results showed that both markers, anti-PCNA and anti-CD34, are useful for investigating proliferative and angiogenic activity, respectively. However, anti-PCNA showed better and more accurate results than anti-CD34 in differentiating intraepithelial neoplasias.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(4):209-215
DOI 10.1590/S0100-72032001000400003
Purpose: to evaluate a populational sample of the screening proposed by the National Program of Uterine Cervical Cancer Control (PNCC), regarding the following issues: frequency of unsatisfactory cytologic results, cytologic frequency of atypical squamous or glandular cells of undetermined significance (ASCUS, AGCUS), low- or high-grade squamous intraepithelial lesions (SIL), comparing the cytologic results with anatomicopathological results of colposcopically directed biopsies. Methods: through the written, broadcasting television and oral midia, women between 35 and 49 years were requested to have a preventive cytopathological test, to be collected by the authorized public health or other institutions accredited by SUS. The slides were analyzed by the program-authorized laboratories and all those patients from the populational sample from the municipality of Naviraí in the State of Mato Grosso do Sul with cellular alterations were submitted to colposcopy and directed biopsy. Results: the frequency of cytologic alterations of the ASCUS, AGCUS and SIL types was 3.3%, an index that is close to that predicted by the PNCC (4%); the percentage of samples that were unsatisfactory for evaluation was high (12.5%); among the ASCUS, AGCUS or low grade-SIL patients, 27.3% presented intraepithelial lesions of a high grade in the anatomicopathological study; while patients with cytology compatible with high grade-SIL, the directed biopsy revealed that 12.5% presented low-grade intraepithelial lesions. Conclusions: the choice of oncological cytology as the only method for the screening in the program allowed high indexes of false-negatives (27.3%) and of false-positives (12.5%). In the screening of cervical neoplasms, colposcopy has shown to be an important and indispensable method to guide the therapeutical management to be adopted.