Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(4):295-298
DOI 10.1590/S0100-72032004000400005
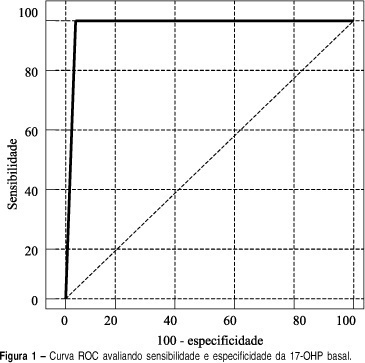
INTRODUCTION: adrenal hyperplasia is a common genetic disorder and 95% of the cases are due to a 21-hydroxylase deficiency. Clinical presentation varies from life-threatening salt-losing adrenal hyperplasia to simple androgenic states, which can be of late-onset and very similar to polycystic ovary syndrome. Diagnosis is usually made by synthetic ACTH provocative tests but efforts are being made to simplify this investigation. OBJECTIVE: to evaluate basal 17-hydroxyprogesterone as a predictor of the provocative test for the diagnosis of late-onset congenial adrenal hyperplasia. METHODS: A total of 122 patients under clinical suspicion of diagnosis of late-onset congenial adrenal hyperplasia were included and retrospectively evaluated in the study. Such suspicion included signs and/or symptoms of hyperandrogenism (hirsutism, acne, oily skin, menstrual irregularity etc.). All the patients were submitted to the 0.25mg synthetic ACTH provocative test (Synacthen®). After resting for 60 minutes, the samples were taken in the basal time and 60 minutes after the administration of 0.25mg synthetic ACTH, in order to assay 17-hydroxiprogesteron, the venous access being kept through a heparinized catheter. Radioimmuoessay was the method used to accomplish the assay of seric 17-hydroxiprogesteron. The sensitivity and specificity of the basal 17-hydroxiprogesteron were measured, assessing several cutoff points. ROC curves were made to analyze the test performance, using the software Medcalc®. RESULTS: ROC curve analysis showed that the best cutoff point was 181 ng/dl, which was very similar to the most common recommendation of 200 ng/dl of the literature. The cutoff point of 200 ng/dl shows positive and negative predictive values of 75 and 100%, and accuracy of 98,4% as a diagnostic test for late-onset adrenal hyperplasia. CONCLUSIONS: considering our data, we suggest that all hyperandrogenic patients should start the investigation with basal 17-hydroxyprogesteron and in case it is above 181 ng/dl, then they should do the synthetic 17-hydroxyprogesteron provocative test.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(4):289-294
DOI 10.1590/S0100-72032004000400004
OBJECTIVE: to study the relationship of biobehavioral factors, such as age, menarche, number of gestations, and age of first sexual intercourse, with changes in Langerhans'cells in women with negative hybrid capture for HPV. METHODS: thirty women referred due to abnormal cervical cytology or premalignant cervical lesions were studied and underwent colposcopy, guided biopsy and histopathological exams. The Langerhans' cells were identified by immunohistochemical (S100+) exams. Langerhans' cells visualized in brown color were counted using the software Cytoviewer. The nonparametric Wilcoxon rank-sum test was employed for statistical analysis. RESULTS: the number of Langerhans' cells in women who had menarche after 13 years old presented statistically significant difference (173.34 cell/mm²) compared to the group whose menarche occurred before 13 (271.41 cell/mm²). The age at the first sexual intercourse was associated with the low number of Langerhans' cells, 127.15 cell/mm² and 250.14 cell/mm², respectively, for the beginning of the sexual activity up to 17 years old and after 17 (p=0.03). Previous cauterizations of the uterine cervix have been related to a lower number of Langerhans' cells in the epithelium, with the average 120.30 cell/mm² as compared to 236.06 cell/mm² for those women who never underwent that procedure (p=0.05). Other factors such as the patient's age and the number of gestations showed no statistically significant differences in the density of Langerhans' cells. CONCLUSIONS: the present study reports the association of biobehavioral factors with decrease in the number of Langerhans' cell.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(4):277-287
DOI 10.1590/S0100-72032004000400003
OBJECTIVE: to compare the prevalence of DNA of human papillomavirus (HPV), in samples of normal endometrial tissue, and tissue with endometrial carcinoma of women submitted to surgical treatment (hysterectomy), or between endometrial carcinoma and benign disease, through the PCR technique. METHODS: this is an observational control-case study where 100 women (50 with endometrial carcinoma and 50 with normal endometrial tissue) were analyzed for the detection of HPV DNA in samples of endometrial tissue kept in paraffin blocks by the PCR technique. The cases of endometrial carcinoma with uncertain primary site of the lesion as well as the cases with previous or current history of pre-neoplasic lesions or carcinoma of the lower genital tract were excluded. Variables as age, smoking habit, endometrial trophism, squamous differentiation and degree of tumor differentiation were also evaluated. RESULTS: the estimated relative risk of the presence of HPV in the endometrial carcinoma and in the normal endometrial tissue was the same. HPV was detected in 8% of the cases of carcinoma and 10% in the normal endometrial tissue. In spite of HPV having been 3.5 times more detected in women with smoking habit in the group without carcinoma, there was no statistical difference. The presence of HPV was also not correlated with the women's age, endometrial trophism, squamous differentiation and degree of tumor differentiation. The HPV types 16 (5 cases) and 18 (4 cases) were the viruses most frequently found both in the normal endometrial tissue or in the tissue with carcinoma. No oncogenic low risk virus was detected in the samples. CONCLUSION: The same proportion of HPV is present in the endometrial tissue of women with endometrial cancer and with normal endometrium. It could not be demonstrated a possible correlation of DNA of HPV with the development of endometrial carcinoma.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(4):269-275
DOI 10.1590/S0100-72032004000400002
OBJECTIVE: to evaluate the performance of Pap smear, hybrid capture II (HC II), and visual inspection with acetic acid in the detection of pre-invasive and invasive cervical lesions. METHODS: a total of 2281 women were submitted to a clinical exam, including Pap smear, HC II for HPV DNA detection and visual inspection with 5% acetic acid (VIA). When at least one of the tests was positive, colposcopy was performed and targeted biopsies were taken from suspicious lesions. Colposcopy was also performed in 420 women with negative results. Test performance was evaluated, using colposcopy as the gold standard, with or without biopsy. RESULTS: Pap smear, VIA and HC II were positive in 9.2, 10.9 and 17.5% of all women screened, respectively. Although at least one positive test was found in 671 women (29.4%), only 82 (3.6%) presented histologically confirmed disease (50 NIC1, 20 NIC2, 7 NIC3, and 5 invasive carcinoma). VIA and HC II sensitivities were similar and significantly higher than Pap smear. Pap smear showed better specificity than VIA and than HC II. In women with a negative Pap smear result, VIA showed better performance than HC II. CONCLUSION: Pap smear combined with VIA performed better than Pap smear combined with HC II or than Pap smear alone.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(3):213-219
DOI 10.1590/S0100-72032004000300007
OBJECTIVE: to evaluate the effectiveness of the hygroscopic dilator in the colposcopic examination of the endocervical canal in patients with high-grade lesion in the cytopathology and unsatisfactory colposcopy. METHODS: prospective study, including 62 patients with unsatisfactory colposcopic examination and cytology compatible with high-grade intraepithelial lesion. The patients were submitted to dilation of the endocervical canal by means of a hygroscopic dilator. After dilation, the new colposcopic findings were recorded, and then conization was made through loop electrosurgical excision procedure. The incidence of neoplasic involvement of surgical margins was compared between patients with examinations modified toward satisfactory results and those that remained with unsatisfactory colposcopy. In order to compare the incidence of involved margins and the incidence of residual disease, two retrospective control-groups were used: the GinSat group (n = 35): patients with unsatisfactory colposcopy; GSat group (n = 38): patients with satisfactory colposcopy and endocervical atypy. RESULTS: 80.6% of the cases presented satisfactory colposcopic vision after dilation. 80.4% of those presented disease-free resection margins. The incidence of disease-free resection margins in patients with persistent unsatisfactory colposcopy after dilation was 36.3%. Affected surgical margins occurred in 28% of the group that had undergone dilation, 28.5% of the cases in GinSat group, and 31.5% in the Gsat group. Follow-up showed the incidence of residual disease in 7.5% of the patients under dilation, 28.5% in the GinSat group and 28.9% in the GSat group. CONCLUSION: the use of hygroscopic dilation improved visualization of lesions of difficult access to the colposcopic examination, thus permitting reduction in the percentage of residual neoplasic disease in patients with unsatisfactory colposcopy treated with loop electrosurgical excision procedure.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(3):233-240
DOI 10.1590/S0100-72032004000300010
OBJECTIVE: to evaluate the existence of intra and intercytophathologists disagreement in the analysis of cervical slides previously diagnosed as atypical skin cells with undetermined significance (ASCUS), and the degree of this disagreement. METHODS: a transversal study of 50 cervical slides of Pap smears previously diagnosed as ASCUS, collected in November 2000 in Contagem town. They were analyzed and classified by four cytopathologists according to the first Bethesda system review of 1991 (normal, atrophic alteration, inflammatory alteration, suggestive of LoSIL, suggestive of HiSIL, suggestive of invasive carcinoma and others). After the first analysis, the slides were renumbered in a random order and sent to the same cytophathologists for a new exam. The Kappa test and the weighted Kappa were used in the analysis of the results. RESULTS: there was a high degree of disagreement between the different analyses of the same cytopathologist, varying from 7.8 to 74.4% according to the Kappa test. When a weight of 20% was settled for each degree of disagreement, these values increased from 16.1% for the cytopathologist A to 81.08% for the cytopathologist B. Concerning the comparative analyses made by different examiners the Kappa test values obtained varied from 50.6% to 63.4% in the normal and weighted versions, respectively. CONCLUSIONS: this study confirms the existence of subjectivity in the analysis of the ASCUS category and imprecision in the analysis criteria by the same examiner.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(3):227-232
DOI 10.1590/S0100-72032004000300009
PURPOSE: to identify the risk factors associated with the occurrence of surgical site infection (SSI) in surgeries for the treatment of breast cancer. METHODS: the study was conducted on 140 women submitted to treatment of invasive breast cancer during the period from January 2001 to December 2002. SSI was defined as infection occurring up to 30 days after surgery and was related to the operation, according to the standard criteria adopted by the Centers for Disease Control and Prevention (CDC), USA. SSI were considered to be superficial when they involved only the skin and subcutaneous tissue and deep when they involved deep tissues at the site of incision, such as fascia and muscles. The risk factors related to patient were age, hormonal status, staging, body mass index (BMI) and hemoglobin, and the factors related to surgery were type of operation, time of hospitalization, duration of surgery, and formation of seroma and hematoma. Data concerning numerical nonparametric variables were analyzed by the Mann-Whitney test and quantitative variables were analyzed by the Fisher exact test. RESULTS: of the 140 patients studied, 29 (20.7%) presented SSI, which were superficial in 19 (13.6%) and deep in 10 (71%); 111 patients did not present SSI and represented the control group. The risk factors associated with the patient and the disease were locally advanced stage (odds ratio = 27; 95% CI: 1.1-6.5) and obesity, represented by a mean BMI of 32.2 kg/m² in the patients with SSI and a mean BMI of 27.2 kg/m² in the control group (p<0.0001). The factors related to treatment of the disease were the use of neoadjuvant chemotherapy (odds ratio = 2.7 (95% CI: 1.1-6.5), the duration of surgery, whose median value was 165 minutes for the patients who developed the infection and 137 minutes for the control group (p=0.02), and the number of days of use of the postoperative drain, whose median value was 6 days for the patients with SSI and 5 days for the control group (p=0.048). CONCLUSION: on the basis of the identification of risk factors such as advanced stage, neoadjuvant chemotherapy and obesity, preoperative care for these patients should be emphasized. The use of an accurate surgical technique may reduce the impact of other factors such as surgical time and time of use of the drain.