Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(7):451-455
DOI 10.1590/S0100-72032001000700007
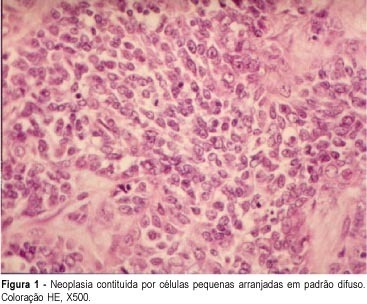
Purpose: to evaluate clinical findings, diagnosis and prognosis of three recent hypercalcemic small cell ovarian carcinoma (HSCC) cases treated in our institution. Methods: information concerning epidemiological data and clinical evolution was obtained from the medical record review. Diagnosis was confirmed through histologic evaluation by our Pathology Department. Results: patients were, at diagnosis, 26, 36 and 38 years old. Tumor diameter ranged from 8.8 cm to 23 cm (mean = 14 cm). All patients presented hypercalcemia with total calcium serum levels of 8.9, 10.8 and 16.7 mEq/dL (NV = 8.8 to 10.2) and ionic calcium levels of 1.26, 1.27 and 1.21 mEq/dL respectively (NV = 1.12 to 1.23). All three patients were submitted to surgical treatment and chemotherapy with platinum-based regimens. In two patients the chemotherapy was adjuvant to the primary surgical treatment. Both are alive and disease-free after 2 and 18 months of follow-up. The other patient had initially the diagnosis of granulosa cell tumor, receiving chemotherapy only after tumor recurrence. Now she is alive with tumor 32 months after diagnosis. Conclusion: the main prognostic factors, in the literature and our experience, are the tumor stage at diagnosis, patient's age, presence of hypercalcemia, large cells, tumor diameter, type of surgical treatment and delay of definitive therapy. The ideal treatment of the hypercalcemic small cell ovarian carcinoma remains unknown. Difficulties in determining a standard therapeutic strategy include rarity of the neoplasm, frequently inadequate initial staging, difficulties in histologic diagnosis and multiple therapeutic approaches.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(7):459-462
DOI 10.1590/S0100-72032001000700008
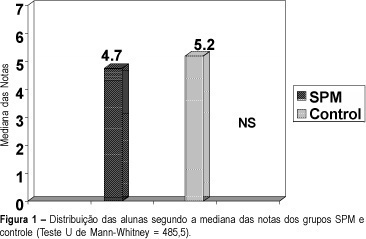
Purpose: to compare the performance in tests between students with and without premenstrual syndrome (PMS), and between students with PMS in and outside the premenstrual period. Methods: the present study had a before-after design (quasi-experimental), to which 40 control patients without PMS were added. A total of 40 students from high school and courses for admission to the University were evaluated using, a standardized questionnaire. The students were divided, according to the scores obtained, into three groups: A) PMS group in the premenstrual period; B) PMS group outside the premenstrual period; C) control group (no PMS). The marks obtained in Physics and Math tests by the groups with and without PMS were analyzed by the Mann-Whitney test. The marks of the group PMS in and outside the premenstrual period were evaluated by the signal test. Results: of 4438 questionnaires applied, 29 from students with PMS and 29 from controls were selected. Comparing the medians of the marks obtained by the students from the PMS group in and outside the premenstrual period, there was no significant difference. There was also no significant difference between the marks of the PMS and control groups. Also, when the scores were evaluated, there was no difference in and outside the period, in the PMS group. Conclusion: PMS was not able to modify significantly the students' marks or scores in this study.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(8):481-488
DOI 10.1590/S0100-72032001000800002
Purpose: to investigate leptin levels in patients with polycystic ovary syndrome (PCOS), and relationships with testosterone, estradiol, follicle-stimulating hormone (FSH) and insulin levels. Methods: transversal study on 40 patients with PCOS divided into two groups: Group I (n = 20)- obese women (body mass index - BMI > or = 28 kg/m²), and Group II (n = 20) - non obese women (BMI <28 kg/m²). Results: BMI was different between the two groups (p=0.04). We observed that leptin concentrations were significantly correlated with BMI (p<0.001). After adjusting for BMI, no correlation between leptin, insulin (p=0.194), FSH (p=0.793), and total (p=0.441) and free (p=0.422) testosterone was found. However, we only observed positive correlations between leptin and estradiol (p=0.043). Conclusions: there is a strong correlation between leptin levels, BMI and estradiol levels in women with PCOS.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(8):491-495
DOI 10.1590/S0100-72032001000800003
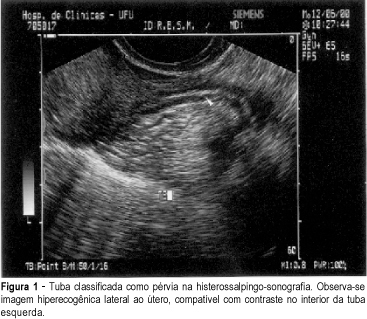
Purpose: to evaluate hysterosalpingo-contrast sonography as an alternative method in the study of tubal patency in a group of infertile women. Methods: this is a transversal clinic study, which analyzed hysterosalpingo-contrast sonography and compared it with hysterosalpingography, as a method for the study of tubal patency, in a group of 31 infertile patients. Hysterosalpingo-contrast sonography had a sensitivity of 93.6%, specificity of 75%, positive predictive value of 95.6%, negative predictive value of 66.7% and accuracy of 90%. The tubes were not accessible in 8.9%. The mean time to perform the examination was 12 minutes. Fourty-six percent of the patients did not report pain during the examination and 23% reported light, 19.2% moderate, and only 11.5% reported severe pain. Conclusion: hysterosalpingo-contrast sonography proved to be a safe, and tolerable method, of quick performance, with good sensitivity and specificity in the study of tubal patency in infertile women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(8):499-504
DOI 10.1590/S0100-72032001000800004
Purpose: to evaluate factors that might influence the results of nonphamacological treatment (verbal guidance) in women with clinical mastalgia. Methods: an uncontrolled study of the experimental type was conducted on a sample of 128 women with a clear history of clinical mastalgia treated with verbal guidance. A visual analogue scale for pain was used before and after treatment to evaluate pain intensity and mastalgia was classified into grade I (mild), grade II (moderate) and grade III (severe) according to pain intensity. The Cardiff Breast Score (CBS), modified, was also used to evaluate the clinical response to treatment. Data were analyzed statistically using the chi² test (Epi-Info 6.04). Results: we noted that factors such as parity, menarche, age at first term delivery and breast-feeding had no significant effect (p=0.19, p=0.31, p=0.80 and p=0.54, respectively) on the results of nonpharmacological treatment (verbal guidance). On the other hand, when age was taken into consideration, 26 patients (78.8%) aged 40 years or older were found to benefi more from verbal guidance, with a significant difference (p=0.01) when compared to younger women. Conclusion: reproductive factors such as parity, menarche, age at first term delivery and breast-feeding did not affect the results of nonpharmacological treatment (verbal guidance), whereas the age factor had a specific and significant effect on the results.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(8):507-513
DOI 10.1590/S0100-72032001000800005
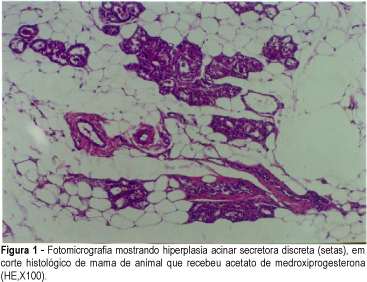
Purpose: to evaluate the effect of hormone replacement therapy on breast cell proliferation and on collagen and elastic fiber formation and to analyze the changes occurring in the breast parenchyma as a whole. Method: a total of 61 adult Wistar rats were divided into 5 groups. The standard group (12 rats) represented the normal hormonal ovarian status. The remaining 49 rats were oophorectomized and, starting on the 96th P.O. day, received the specific drug for 30 days. The CEE group received 50 mg/day conjugated equine estrogens (13 rats); the MPA group, 2.0 mg/day medroxyprogesterone acetate (12 rats); the CEE + MPA group, both drugs (12 rats), and the DW group, distilled water (12 rats). On the 31st day of medication, the animals were sacrificed and the inguinal mammary glands were removed for histological analysis. Cell proliferation was assessed at the ductal and acinar levels using anti-PCNA antibody. Mature collagen (type I) and immature collagen (type III) were quantified by Sirius-Red staining, and elastic fiber formation was quantified by Weigert staining. Anatomopathological analysis was performed by hematoxylin-eosin staining, with the determination of number of acini per terminal duct, number of ducts per field, presence of intraductal secretion, and intensity of intracytoplasmic vacuolization. Results: the CEE + MPA group presented a smaller percentage of proliferating ductal cells (46.1%) (p<0.0001) and a greater proliferation of acinar cells (66.3%), similar to those detected in the MPA group (p=0.075) but differing from those detected in the remaining groups (p<0.004). The CEE group showed the largest amount of immature collagen (33.6%) (p<0.01) and the MPA group showed the highest concentration of elastic fibers (11.7%) (p<0.0001). The CEE + MPA and MPA groups showed secretory acinar hyperplasia that was intense (91.7%) in the CEE + MPA group and mild (41.7%) or moderate (58.3%) in the MPA group, but differering in both cases from the remaining groups (p<0,097). Conclusions: conjugated equine estrogens in combination with medroxyprogesterone inhibit ductal cell proliferation and stimulate acinar cell proliferation causing secretory acinar hyperplasia; conjugated horse estrogens intensify the formation of immature (type III) collagen, and medroxyprogesterone acetate increases the formation of elastic fibers.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(8):517-521
DOI 10.1590/S0100-72032001000800006
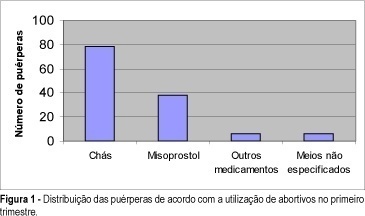
Purpose: to verify the association of the use of abortifacient drugs during the first 3 months of gestation with the occurrence of congenital malformations in live births. Patients and Methods: population-based case-control study through selection of the first six live births on a day, over the period of a year, at a public maternity in Salvador, Bahia, with a total of 800 cases. Studies were performed through investigation of birth records in the search of congenital malformation data, observation of selected malformed newborns, followed by interview with the mothers for collection of anamnesis data, by application of a questionnaire. Later on data were statistically evaluated by Epi-Info 5.0 software. Results: puerperae came from a low socialeconomic class (74.8%), without any or almost any schooling (61.1%). The general percentage of birth defects was estimated at 4.7%. Out of 800 puerperae, 16% reported abortifacient drug intake during the first 3 months of gestation and 10.9% of them had malformed babies. This incidence was 3.6% in children whose mothers denied the intake of any abortifacient drugs. Agents most commonly taken in those unsuccessful abortive attempts were misoprostol (Cytotec) and herbs, specially "alumã" (Vermonia baiensis Tol) and "espinho cheiroso" (Kanthoxilum shifolium Lam), which, according to the literature, do not really have any abortive effect. Conclusion: the study revealed the extension of intentional miscarriage in a low income population and showed that the occurrence of birth defects could be related to gestational exposure to misoprostol and herbal medicine intake.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(8):523-527
DOI 10.1590/S0100-72032001000800007
Purpose: to study perinatal outcome in asthmatic pregnant patients who required hospital admission to control acute exacerbations. Patients and Method: retrospective study of 12 pregnant asthmatic patients admitted at the Hospital das Clínicas, Department of Obstetrics and Gynecology, FMRP-USP, during the period between 1992 and 1996. The analyzed data included: maternal age, prenatal care, length of hospitalization, gestational age at delivery, type of delivery, neonatal weight and Apgar score. Results: among the 12 asthmatic pregnant patients 7 did not have prenatal care for acute exacerbation treatment before hospitalization. Three of 12 developed preeclampsia (one with premature rupture of membranes and infection of the amniotic cavity and one with premature separation of the placenta); 2 of 12 were diagnosed with premature placental aging (one with premature labor and twin-to-twin transfusion syndrome and one with oligohydramnios); 1 of 12 was diagnosed with oligohydramnios and fetal death and had pneumonia, and 1 of 12 was diagnosed with polyhydramnios. Among the infants, 3 were small for gestational age. Conclusions: perinatal complications were more frequent in asthmatic pregnant patients who required hospital care for the acute exacerbations. Chronic asthmatic patients in reproductive age should be advised before pregnancy about the prophylactic measures to reduce the incidence of acute crises and exacerbations during pregnancy should be treated promptly.