Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):207-215
05-24-2021
The evaluation of the available evidence on vertical transmission by severe acute respiratory syndrome coronavirus 2 (SARS-CoV)-2.
An electronic search was performed on June 13, 2020 on the Embase, PubMed and Scopus databases using the following search terms: (Coronavirus OR COVID-19 OR COVID19 OR SARS-CoV-2 OR SARS-CoV2 OR SARSCoV2) AND (vertical OR pregnancy OR fetal).
The electronic search resulted in a total of 2,073 records. Titles and abstracts were reviewed by two authors (WPM, IDESB), who checked for duplicates using the pre-established criteria for screening (studies published in English without limitation regarding the date or the status of the publication).
Data extraction was performed in a standardized way, and the final eligibility was assessed by reading the full text of the articles. We retrieved data regarding the delivery of the potential cases of vertical transmission, as well as themain findings and conclusions of systematic reviews.
The 2,073 records were reviewed; 1,000 duplicates and 896 clearly not eligible records were excluded. We evaluated the full text of 177 records, and identified only 9 suspected cases of possible vertical transmission. The only case with sufficient evidence of vertical transmission was reported in France.
The risk of vertical transmission by SARS-CoV-2 is probably very low. Despite several thousands of affected pregnant women, we have identified only one case that has fulfilled sufficient criteria to be confirmed as a case of vertical transmission. Well-designed observational studies evaluating large samples are still necessary to determine the risk of vertical transmission depending on the gestational age at infection.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(12):686-691
12-01-2017
To verify if pethidine is safe for the conceptus when used during labor.
Systematic review in the Capes Periodicals/PubMed and MEDLINE/Virtual Health Library (BVS, in the Portuguese acronym) databases.
A total of 17 studies published from January 1st, 2000, to September 2nd, 2016, with a total of 1,688 participants involved were included in the present review. There was no record of conceptus vitality decrease associated with low doses of pethidine being administered to mothers during labor.
Intramuscular (IM) or intravenous (IV) pethidine at low doses, of up to 50 mg, is safe to administer during labor.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):622-631
11-01-2017
Preeclampsia, a multifactorial disease with pathophysiology not yet fully understood, is a major cause of maternal and perinatal morbidity and mortality, especially when preterm. The diagnosis is performed when there is an association between arterial hypertension and proteinuria or evidence of severity. There are unanswered questions in the literature considering the timing of delivery once preterm preeclampsia has been diagnosed, given the risk of developingmaternal complications versus the risk of adverse perinatal outcomes associated with prematurity. The objective of this systematic review is to determine the best timing of delivery for women diagnosed with preeclampsia before 37 weeks of gestation.
Systematic literature review, performed in the PubMed database, using the terms preeclampsia, parturition and timing of delivery to look for studies conducted between 2014 and 2017. Studies that compared the maternal and perinatal outcomes of women who underwent immediate delivery or delayed delivery, in the absence of evidence of severe preeclampsia, were selected.
A total of 629 studies were initially retrieved. After reading the titles, 78 were selected, and their abstracts, evaluated; 16 were then evaluated in full and, in the end, 6 studies (2 randomized clinical trials and 4 observational studies) met the inclusion criteria. The results were presented according to gestational age range (< 34 weeks and between 34 and 37 weeks) and by maternal and perinatal outcomes, according to the timing of delivery, considering immediate delivery or expectant management. Before 34 weeks, thematernal outcomeswere similar, but the perinatal outcomes were significantly worse when immediate delivery occurred. Between 34 and 37 weeks, the progression to severe maternal disease was slightly higher among women undergoing expectant management, however, with better perinatal outcomes.
When there is no evidence of severe preeclampsia or impaired fetal wellbeing, especially before 34 weeks, the pregnancy should be carefully surveilled, and the delivery, postponed, aiming at improving the perinatal outcomes. Between 34 and 37 weeks, the decision on the timing of delivery should be shared with the pregnant woman and her family, after providing information regarding the risks of adverse outcomes associated with preeclampsia and prematurity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):632-639
11-01-2017
Axillary web syndrome is characterized as a physical-functional complication that impacts the quality of life of women who have undergone treatment for breast cancer. The present study aims to verify the physiotherapy treatment available for axillary web syndrome after surgery for breast cancer in the context of evidence-based practice. The selection criteria included papers discussing treatment protocols used for axillary web syndrome after treatment for breast cancer. The search was performed in the MEDLINE, Scopus, PEDro and LILACS databases using the terms axillary web syndrome, lymphadenectomy and breast cancer, focusing on women with a previous diagnosis of breast cancer who underwent surgery with lymphadenectomy as part of their treatment. From the 262 studies found, 4 articles that used physiotherapy treatment were selected. The physiotherapy treatment was based on lymphatic drainage, tissue mobilization, stretching and strengthening. The four selected articles had the same outcome: improvement in arm pain and shoulder function and/or dissipation of the axillary cord. Although axillary web syndrome seems to be as frequent and detrimental as other morbidities after cancer treatment, there are few studies on this subject. The publications are even scarcer when considering studies with an interventional approach. Randomized controlled trials are necessary to support the rehabilitation resources for axillary web syndrome.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):235-248
05-01-2017
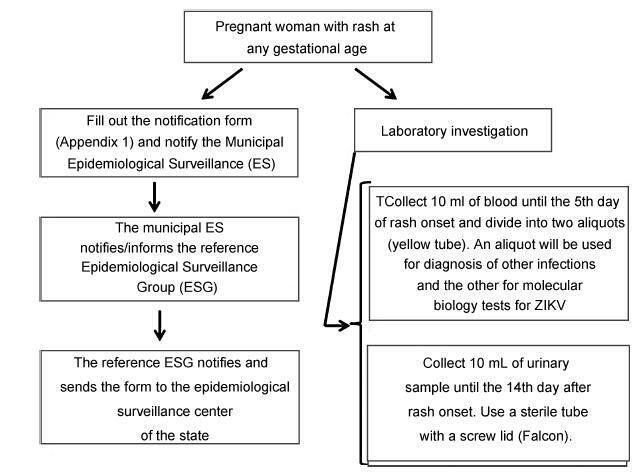
From the discovery of the Zika virus (ZIKV) in 1947 in Uganda (Africa), until its arrival in South America, it was not known that it would affect human reproductive life so severely. Today, damagetothe central nervous system is known to be multiple, and microcephaly is considered the tip of the iceberg. Microcephaly actually represents the epilogue of this infection’s devastating process on the central nervous system of embryos and fetuses. As a result of central nervous system aggression by the ZIKV, this infection brings the possibility of arthrogryposis, dysphagia, deafness and visual impairment. All of these changes of varying severity directly or indirectly compromise the future life of these children, and are already considered a congenital syndrome linked to the ZIKV. Diagnosis is one of the main difficulties in the approach of this infection. Considering the clinical part, it has manifestations common to infections by the dengue virus and the chikungunya fever, varying only in subjective intensities. The most frequent clinical variables are rash, febrile state, non-purulent conjunctivitis and arthralgia, among others. In terms of laboratory resources, there are also limitations to the subsidiary diagnosis. Molecular biology tests are based on polymerase chain reaction (PCR)with reverse transcriptase (RT) action, since the ZIKV is a ribonucleic acid (RNA) virus. The RT-PCR shows serum or plasma positivity for a short period of time, no more than five days after the onset of the signs and symptoms. The ZIKVurine test is positive for a longer period, up to 14 days. There are still no reliable techniques for the serological diagnosis of this infection. If there are no complications (meningoencephalitis or Guillain-Barré syndrome), further examination is unnecessary to assess systemic impairment. However, evidence is needed to rule out other infections that also cause rashes, such as dengue, chikungunya, syphilis, toxoplasmosis, cytomegalovirus, rubella, and herpes. There is no specific antiviral therapy against ZIKV, and the therapeutic approach to infected pregnant women is limited to the use of antipyretics and analgesics. Anti-inflammatory drugs should be avoided until the diagnosis of dengue is discarded. There is no need to modify the schedule of prenatal visits for pregnant women infected by ZIKV, but it is necessary to guarantee three ultrasound examinations during pregnancy for low-risk pregnancies, and monthly for pregnant women with confirmed ZIKV infection. Vaginal delivery and natural breastfeeding are advised.