Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):420-426
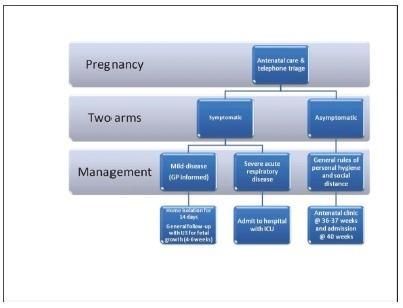
Since the World Health Organization (WHO) declared coronavirus infection (COVID-19) a Public Health Emergency of International Concern in January 2020, there have been many concerns about pregnant women and the possible effects of this emergency with catastrophic outcomes inmany countries. Information on COVID-19 and pregnancy are scarce and spread throughout a fewcase series, with no more than 50 cases in total. The present review provides a brief analysis of COVID-19, pregnancy in the COVID-19 era, and the effects of COVID-19 on pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):427-435
We performed a systematic review to assess the effectiveness and safety of Tribulus terrestris to treat female sexual dysfunction (FSD).
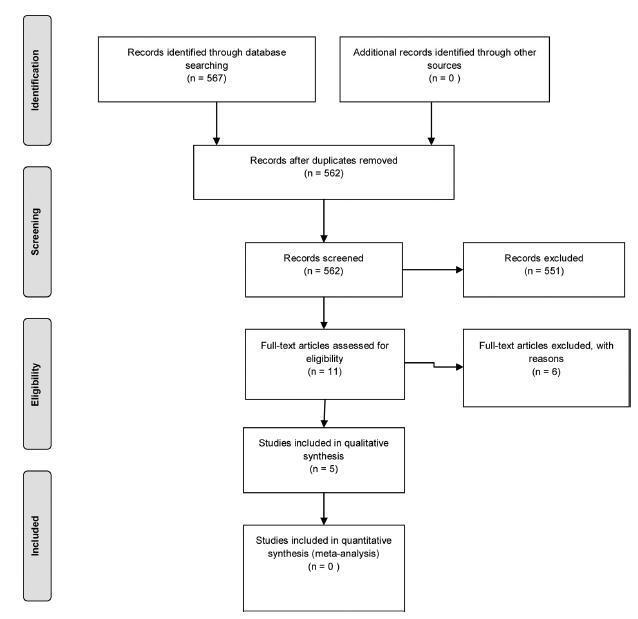
We performed unrestricted electronic searches in the MEDLINE, CENTRAL, EMBASE, LILACS, CINAHL, PsycINFO,WHO-ICTR, Clinicaltrials.gov and OpenGrey databases. Selection of studies We included any randomized controlled trials (RCTs) that compared T. terrestris versus inactive/active interventions. After the selection process, conducted by two reviewers, 5 RCTs (n = 279 participants) were included.
Data extraction was performed by two reviewers with a preestablished data collection formulary.
Due to lack of data and clinical heterogeneity, we could not perform meta-analyses. The risk of bias was assessed by the Cochrane Risk of Bias (RoB) tool, and the certainty of evidence was assessed with Grading of Recommendations, Assessment, Development and Evaluations (GRADE).
After 1 to 3 months of treatment, premenopausal and postmenopausal women randomized to T. terrestris had a significant increase in sexual function scores. Three months of treatment with T. terrestris showed a significant increase in the serum testosterone levels of premenopausal women. There was no report of serious adverse events, and none of the studies assessed health-related quality of life. The certainty of the evidence was very low, whichmeans that we have very little confidence in the effect estimates, and future studies are likely to change these estimates.
MoreRCTs are needed to supportor refute the use of T. terrestris. The decision to use this intervention should be shared with the patients, and the uncertainties around its effects should be discussed in the clinical decision-making process. Number of Protocol registration in PROSPERO database: CRD42019121130
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(6):356-364
The present paper reports on the local treatment of breast cancer from a historical perspective. A search for articles written in English was made in the Medline and EMBASE databases, and 40 papers were selected. Over the past 10 years, various randomized, controlled clinical trials on the local treatment of breast cancer indicated that patients with the samemolecular subtypemay receive different individualized surgical treatments aimed atoptimizing systemic adjuvant therapy. With a view to retaining the gainsmade in diseasefree and overall survival, surgical techniques have advanced from radical surgery to conservative mastectomies, thus reducing sequelae, while adjuvant and neoadjuvant therapies have contributed toward controlling the disease, both distant metastases and local recurrence. Current studies evaluate whether future breast cancer therapy may even succeed in eliminating surgery to the breast and axilla altogether.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(5):289-296
Intrauterine growth restriction (IUGR) is associated with poor perinatal prognosis and a higher risk of stillbirth, neonatal death, and cerebral palsy. Its detection and the evaluation of its severity by new Doppler velocimetric parameters, such as aortic isthmus (AoI), are of great relevance for obstetrical practice. The AoI is a vascular segment that represents a point of communication between the right and left fetal circulations. It is considered to be a functional arterial shunt that reflects the relationship between the systemic and cerebral impedances, and has recently been proposed as a tool to detect the status of hemodynamic balance and prognosis of IUGR in fetuses. In the present review, we noticed that in healthy fetuses, the AoI net flow is always antegrade, but in fetuses with IUGR the deterioration of placental function leads to progressive reduction in its flow until it becomes mostly retrograde; this point is associated with a drastic reduction in oxygen delivery to the brain. The more impaired the AoI flow is, the greater is the risk of impairment in the Doppler velocimetry of other vessels; and the alterations of the AoI Doppler seem to precede other indicators of severe hypoxemia. Although there seems to be an association between the presence of retrograde flow in the AoI and the risk of long-term neurologic disability, its role in the prediction of perinatal morbi-mortality remains unclear. The AoI Doppler seems to be a promising tool in the management of fetuses with IUGR, but more studies are needed to investigate its employment in clinical practice.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(4):218-227
To identify current strategies and recommendations for venous thromboembolism prophylaxis associated with the pregnancy-puerperal cycle, a condition of high morbidity and mortality among women.
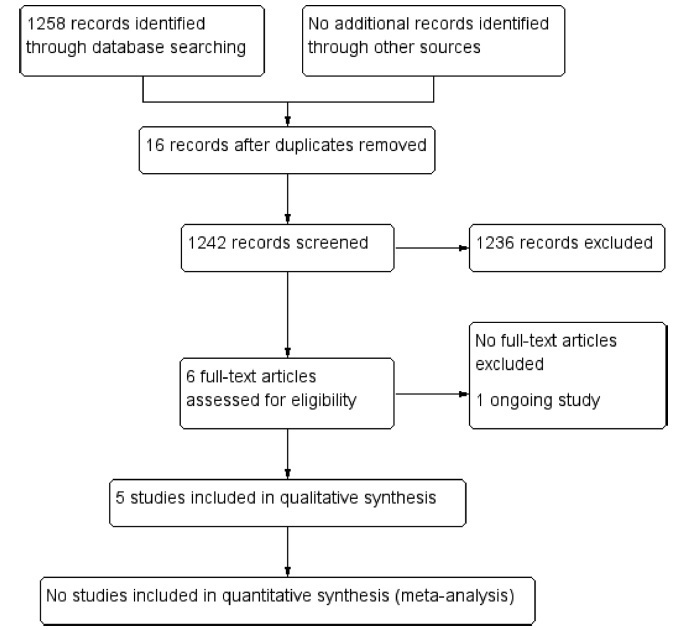
The literature search was performed between May and October 2019, using the PubMed database, including papers published in Portuguese, English and Spanish. The terms thromboembolism (Mesh) AND pregnancy (Mesh) OR postpartum (Mesh) were used as descriptors, including randomized controlled trials, meta-analyses, systematic reviews and guidelines published from 2009 to 2019, presenting strategies for prevention of thromboembolism during pregnancy and the postpartum.
Eight articles met the inclusion criteria. Many studies evaluated were excluded because they did not address prevention strategies. We compiled the recommendations from the American Society of Hematologists, the American College of Obstetricians and Gynecologists, the Royal College of Obstetricians and Gynecologists, the Society of Obstetricians and Gynaecologists of Canada, the American College of Chest Physicians and the Royal Australian and New Zealand College of Obstetricians and Gynaecologists.
There are some gaps in the research, and clinical studies with appropriate methodology are needed to support decisions made regarding the risk of thromboembolism in the perigestational period. Thus, the attention of the professionals involved in the care of pregnant and postpartum women is crucial, as it is a condition associated with high morbidity and mortality.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(3):160-164
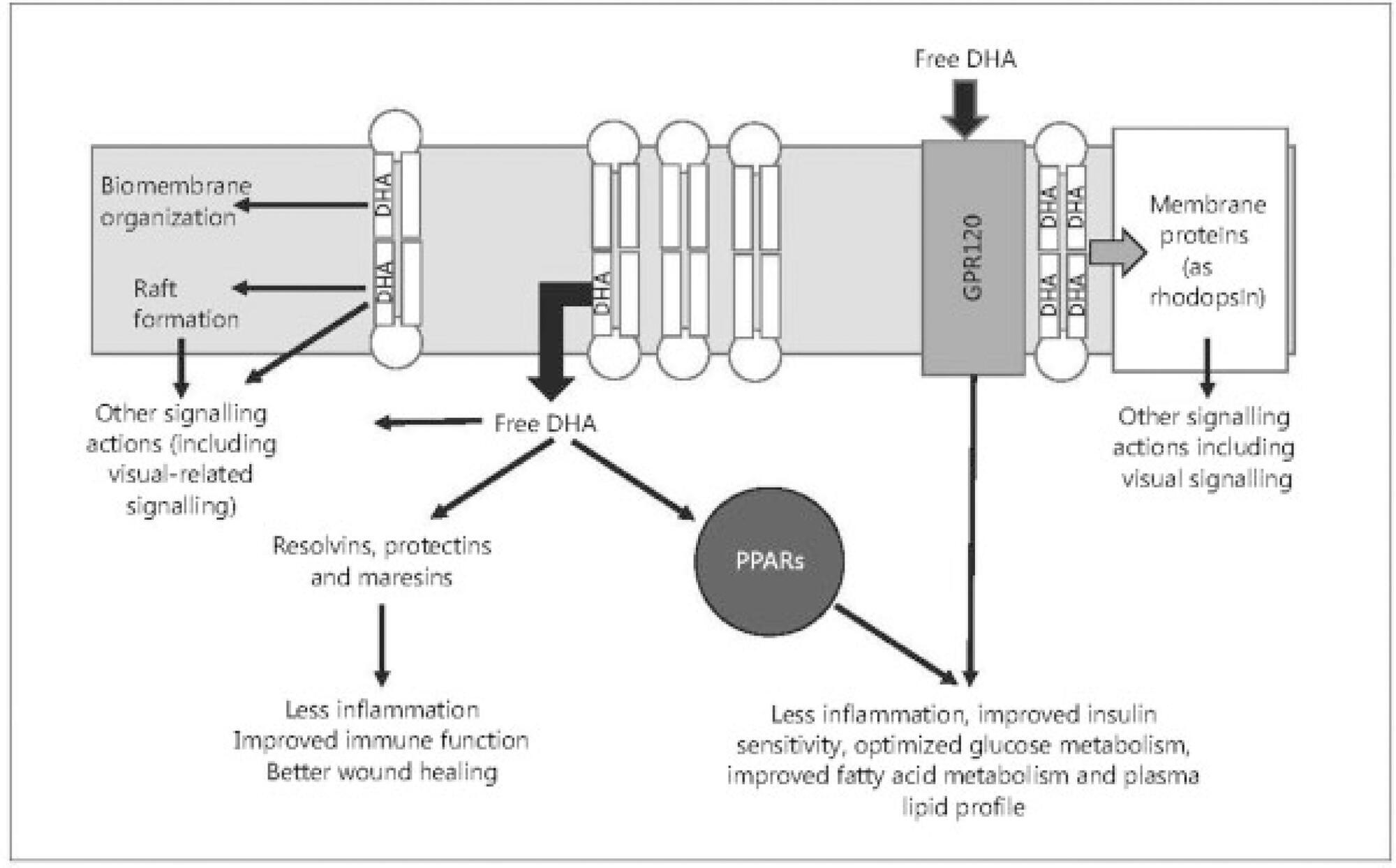
Long-chain omega-3 (n-3) polyunsaturated fatty acids (PUFAs), such as the eicosapentaenoic and docosahexaenoic acids, have been linked to human health in all stages of life, from fetal development to aging. These PUFAs act as precursors for various metabolites involved in the prevention of certain diseases. The recognizable effects of these supplements prior to pregnancy (oocyte maturation), during pregnancy (improvement in the risk of premature delivery, among others) and in the offspring (in terms of cognitive function and the approach to neurodevelopmental disorders) are described in the present narrative review. We concluded that the diffusion of these supplements may improve the prognosis of these patients in a simple, effective way, and with high safety rates.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(10):621-627
Antiphospholipid antibody syndrome (APS) is a systemic, autoimmune, prothrombotic disease characterized by persistent antiphospholipid antibodies (aPLs), thrombosis, recurrent abortion, complications during pregnancy, and occasionally thrombocytopenia. The objective of the present study was to review the pathophysiology of APS and its association with female infertility. A bibliographic review of articles of the past 20 yearswas performed at the PubMed, Scielo, and Bireme databases. Antiphospholipid antibody syndrome may be associated with primary infertility, interfering with endometrial decidualization and with decreased ovarian reserve. Antiphospholipid antibodies also have direct negative effects on placentation, when they bind to the trophoblast, reducing their capacity for invasion, and proinflammatory effects, such as complement activation and neutrophil recruitment, contributing to placental insufficiency, restricted intrauterine growth, and fetal loss. In relation to thrombosis, APS results in a diffuse thrombotic diathesis, with global and diffuse dysregulation of the homeostatic balance. Knowing the pathophysiology of APS, which is closely linked to female infertility, is essential for new therapeutic approaches, specialized in immunomodulation andinflammatory signaling pathways, to provide important advances in its treatment.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(9):564-574
To assess the efficacy of non-surgical treatment for adenomyosis.
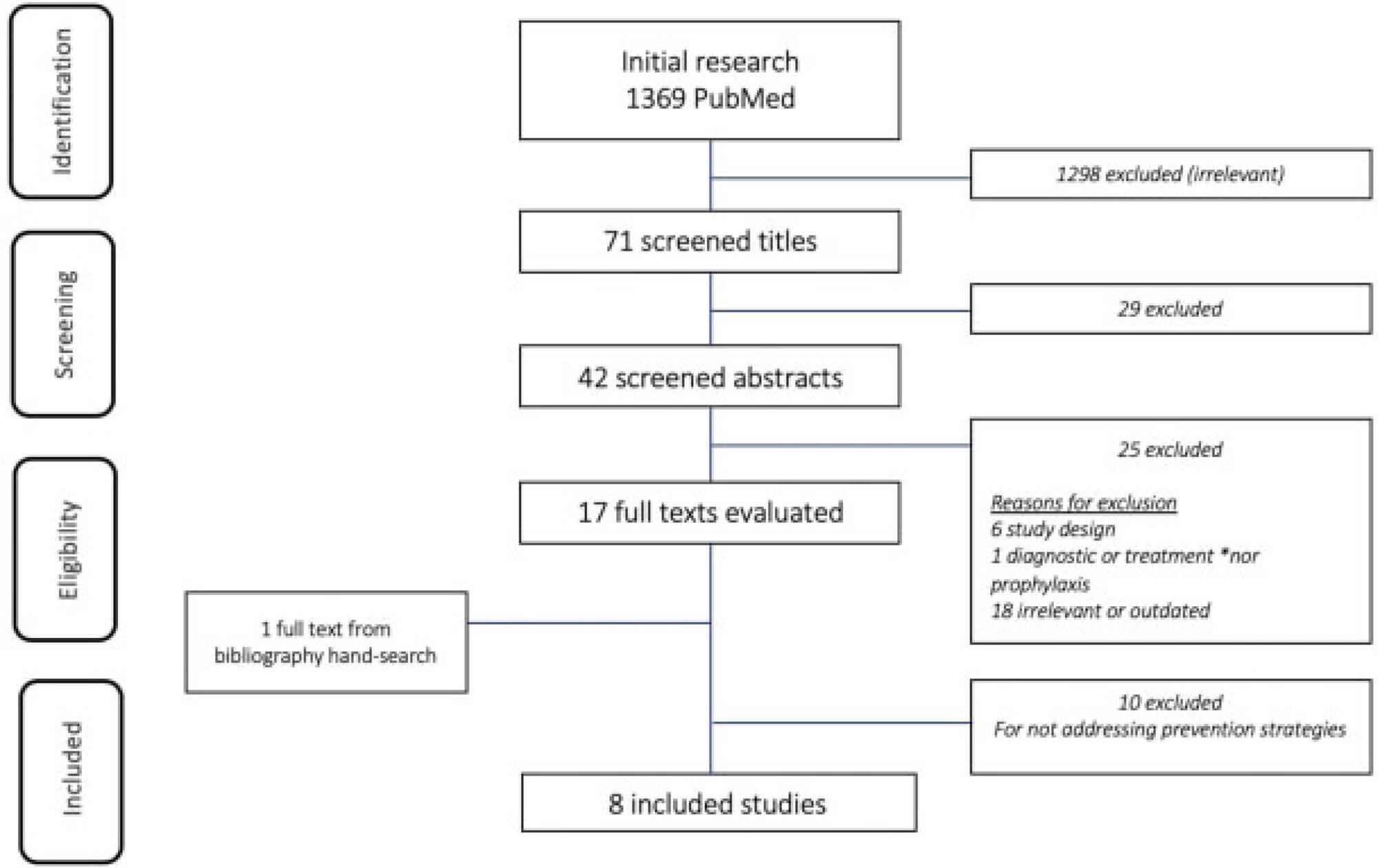
A search was performed by two authors in the Pubmed, Scopus, and Scielo databases and in the grey literature from inception to March 2018, with no language restriction.
We have included prospective randomized studies for treating symptomaticwomen with adenomyosis (abnormal uterine bleeding and/or pelvic pain) diagnosed by ultrasound or magnetic resonance imaging.
Studies were primarily selected by title and abstract. The articles that were eligible for inclusion were evaluated in their entirety, and their data was extracted for further processing and analysis.
From567retrieved records only 5 remained for analysis. The intervention groups were: levonorgestrel intrauterine system (LNG-IUS)(n= 2), dienogest (n= 2), and letrozole (n= 1). Levonorgestrel intrauterine system was effective to control bleeding when compared to hysterectomy or combined oral contraceptives (COCs). One study assessed chronic pelvic pain and reported that LNG-IUS was superior to COC to reduce symptoms. Regarding dienogest, it was efficient to reduce pelvic pain when compared to placebo or goserelin, but less effective to control bleeding than gonadotropin-releasing hormone (GnRH) analog. Letrozolewas as efficient asGnRHanalog to relieve dysmenorrhea and dyspareunia, but not for chronic pelvic pain. Reduction of uterine volumewas seen with aromatase inhibitors, GnRH analog, and LGN-IUD.
Levonorgestrel intrauterine system and dienogest have significantly improved the control of bleeding and pelvic pain, respectively, in women with adenomyosis. However, there is insufficient data from the retrieved studies to endorse eachmedication for this disease. Further randomized control tests (RCTs) are needed to address pharmacological treatment of adenomyosis.