-
Review Article
Efficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo18
04-30-2025
Summary
Review ArticleEfficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo18
04-30-2025Views56Abstract
Objective:
This umbrella review aimed to synthesize evidence from systematic reviews of clinical trials on the efficacy of tranexamic acid in gynecology and obstetrics procedures.
Methods:
We searched Medline, Embase, SciELO and Cochrane Database of Systematic Reviews on March 11, 2024, using the term "tranexamic acid". Four reviewers independently select studies and extract data. We assessed the quality of systematic review and the quality of evidence, using AMSTAR 2 and GRADE tools, respectively.
Results:
Of 651 systematic reviews identified, 16 reviews with 96663 patients were included. The surgical procedures were cesarean section, myomectomy, hysterectomy, and cervical intraepithelial neoplasia surgery. All reviews showed a statistically significant and clinically relevant reduction in intraoperative and post-procedure blood loss, associated with intravenous or topical use of tranexamic acid. Tranexamic acid resulted in a significant reduction in the need for blood transfusions and a less pronounced drop in postoperative hematocrit and hemoglobin levels in cesarean section. Several reviews addressed the same question, but the number of included trials varied substantially, which might indicate flaws in search and selection of studies of these reviews. The quality of systematic reviews was low or critically low, and the quality of evidence was moderate.
Conclusions:
This umbrella review shows that tranexamic acid can reduce blood loss and hemorrhage in gynecology and obstetrics procedures. High quality systematic reviews are still needed.
Key-words Blood transfusionCesarean sectionEfficacyGynecologic surgical procedureshematocritHemorrhageHysterectomyObstetric surgical proceduresTranexamic acidUterine cervical dysplasiauterine myomectomySee more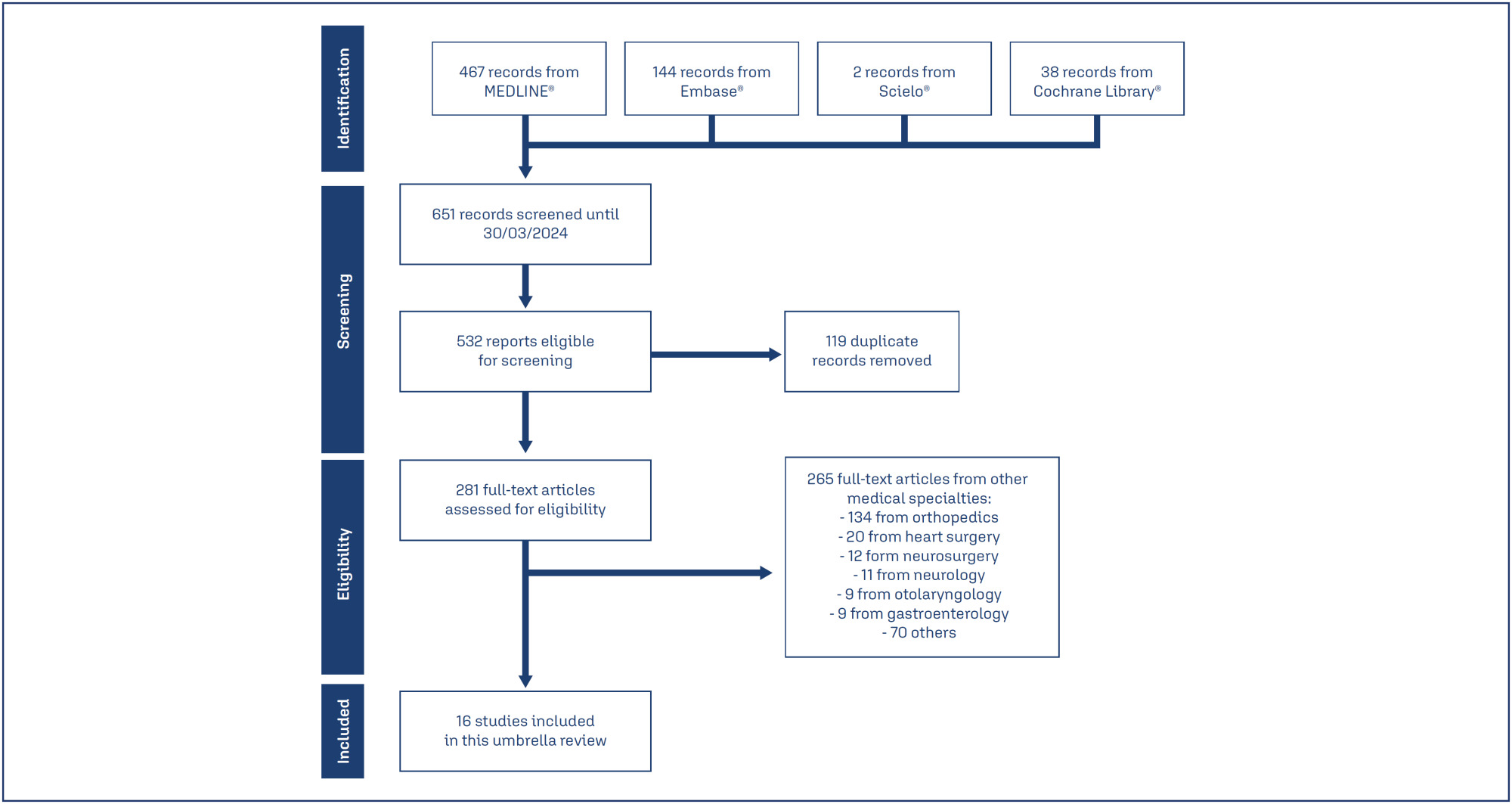
-
Review Article
Letrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
04-30-2025
Summary
Review ArticleLetrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
04-30-2025Views61Abstract
Objective:
We aimed to compare the efficacy and safety of letrozole and clomiphene versus letrozole alone for ovulation induction in patients with Polycystic Ovary Syndrome (PCOS).
Data Sources:
We systematically searched EMBASE, PubMed, and Cochrane databases on October 31, 2024.
Study selection:
We included studies of women with PCOS treated with a combination of clomiphene and letrozole or letrozole alone to induce ovulation that reported any of the outcomes of interest, namely rate of mature follicles and ovulation, ovulation, pregnancy, miscarriages, endometrial thickness, and number of mature follicles.
Data collection:
We pooled odds ratios (OR) and mean difference (MD) with 95% confidence intervals (CI) using a random effects model using R statistical software, version 4.2.1. Heterogeneity was assessed with I statistics, and a random effects model was used.
Data Synthesis:
Four RCTs and two observational studies comprising 592 patients were included. Combined therapy was associated with a higher rate of a mature follicle (OR 2.74; 95% CI 1.72-4.37; p< 0.001; I=0%) and ovulation (OR 2.55; 95% CI 1.57-4.12; p< 0.001; I=35.9%). The number of mature follicles, number of pregnancies, thickness of endometrial lining, and the incidence of adverse events, including headache, abdominal bloating, fatigue, back pain, breast discomfort, and night sweats, were similar between groups.
Conclusion:
In women with anovulatory infertility secondary to PCOS, letrozole and clomiphene citrate combined therapy was associated with improved mature follicle and ovulation rates, with a similar safety profile compared to letrozole alone. However, no significant impact was observed on pregnancy rates.
Key-words ClomipheneInfertility, femaleLetrozoleOvulationOvulation InductionPolycystic ovary syndromeSee more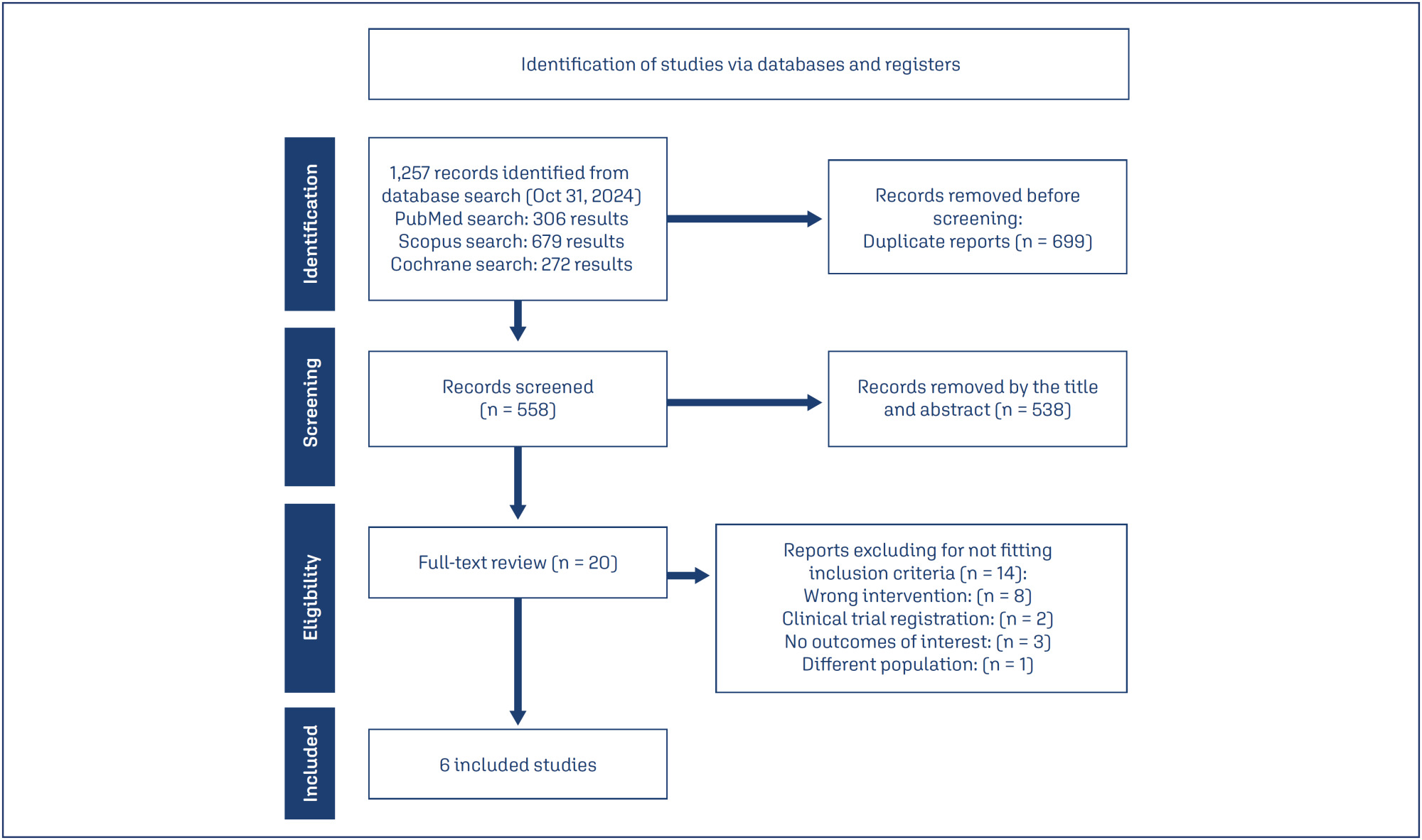
-
Review Article
Efficacy of vitamin C supplementation during pregnancy in the prevention of preterm birth: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo1
03-18-2025
Summary
Review ArticleEfficacy of vitamin C supplementation during pregnancy in the prevention of preterm birth: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo1
03-18-2025Views112Abstract
Objective:
Preterm birth is a leading global cause of neonatal mortality and morbidity, with oxidative stress playing a role in its pathogenesis. Vitamin C, a powerful antioxidant, may help reduce this risk. This study assessed the effectiveness of vitamin C supplementation, both alone and with vitamin E, in preventing preterm birth compared to a placebo.
Data source:
Databases were systematically searched in PubMed, Cochrane and Embase in December 2023 and updated in May 2024.
Study Selection:
Included RCTs evaluated vitamin C's effect on preterm birth and related neonatal outcomes.
Data collect:
Statistical analyses used a random-effects model for pooled risk ratios (RR) and 95% confidence intervals (CI). Heterogeneity was assessed with the I² statistic.
Data synthesis:
Seventeen RCTs (21,567 patients) were analyzed. Vitamin C supplementation showed no significant difference compared to placebo for preterm birth (RR 1.04; 95% CI 0.96, 1.14). No significant differences were observed for neonatal death (RR 0.77; 95% CI 0.55, 1.08), NICU admission (RR 1.03; 95% CI 0.95, 1.13), preterm PROM (RR 1.04; 95% CI 0.63, 1.71), or birth weight (MD 52.41; 95% CI −19.65, 124.47). A slight decrease in gestational age was observed (MD 0.26; 95% CI −0.02, 0.55).
Conclusion:
Vitamin C supplementation alone or in combination with vitamin E does not significantly prevent preterm birth or improve related neonatal outcomes.
Key-words Ascorbic acidFetal membranes, premature ruptureGestational ageIntensive care units, neonatalPregnancyPremature birthVitamin C supplementationVitamin ESee more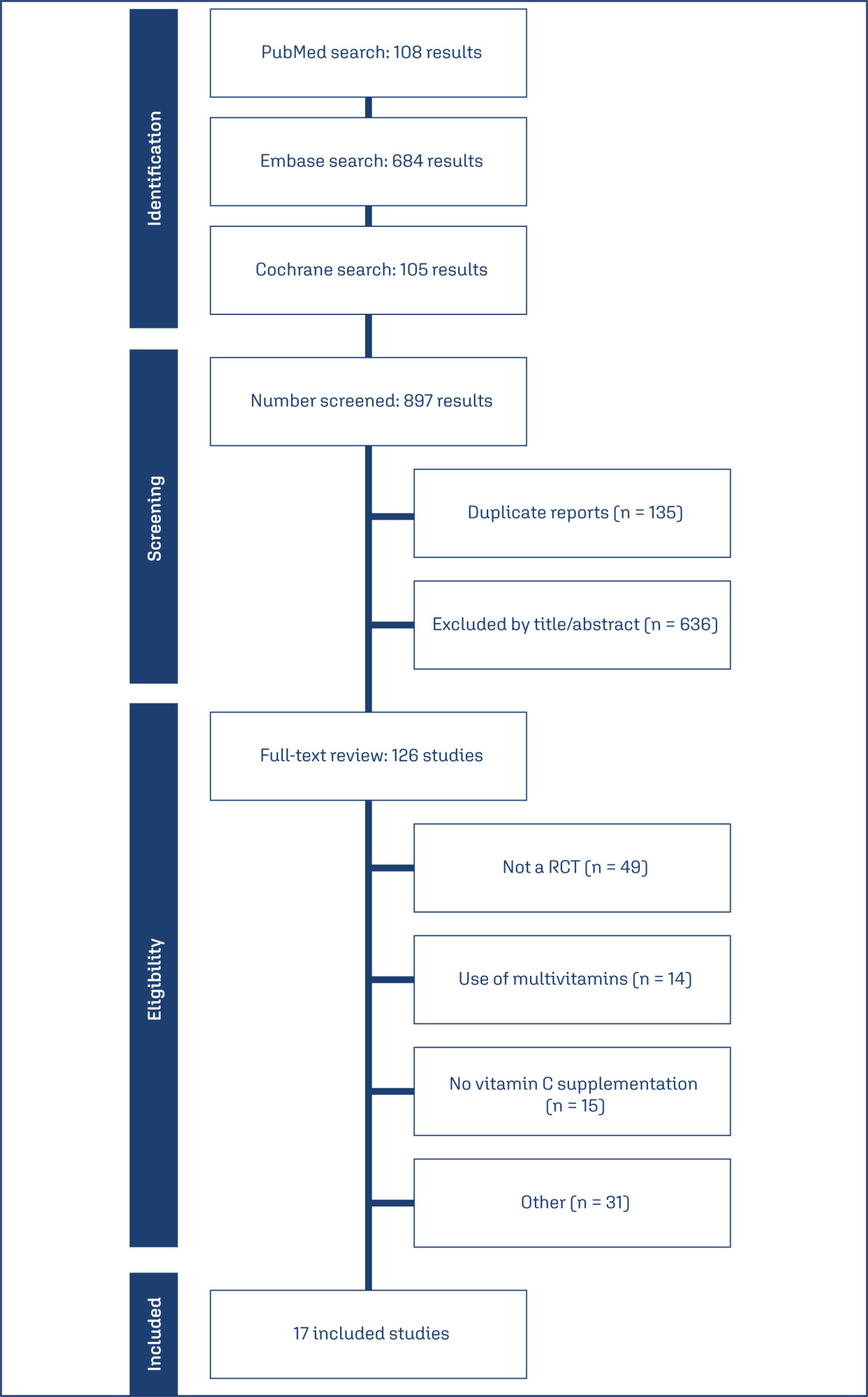
-
Review Article
Clinical repercussions of statin use during pregnancy: a review of the literature
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo2
03-18-2025
Summary
Review ArticleClinical repercussions of statin use during pregnancy: a review of the literature
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo2
03-18-2025Views107Abstract
Statins are the most widely used pharmacological class for treating hyperlipidemia, although they are contraindicated during pregnancy. This study aims to demonstrate the clinical effects of statins in pregnant women through an interactive review. Fifteen original articles were selected, in English or Portuguese, within of five years. Statins have not been associated with the development of fetal malformations and their use may be useful in preventing unfavorable cardiovascular outcomes, with the potential to reduce oxidative stress and angiogenic dysfunction. However, the use of statins to prevent pre-eclampsia in humans has not been properly clarified and further studies are needed. Pravastatin is considered safer than statins for use during pregnancy.
Key-words Antihypertensive agentsHydroxymethylglutaryl-CoA reductase inhibitorsPravastatinPre-eclampsiaPregnancyPregnant womanSee more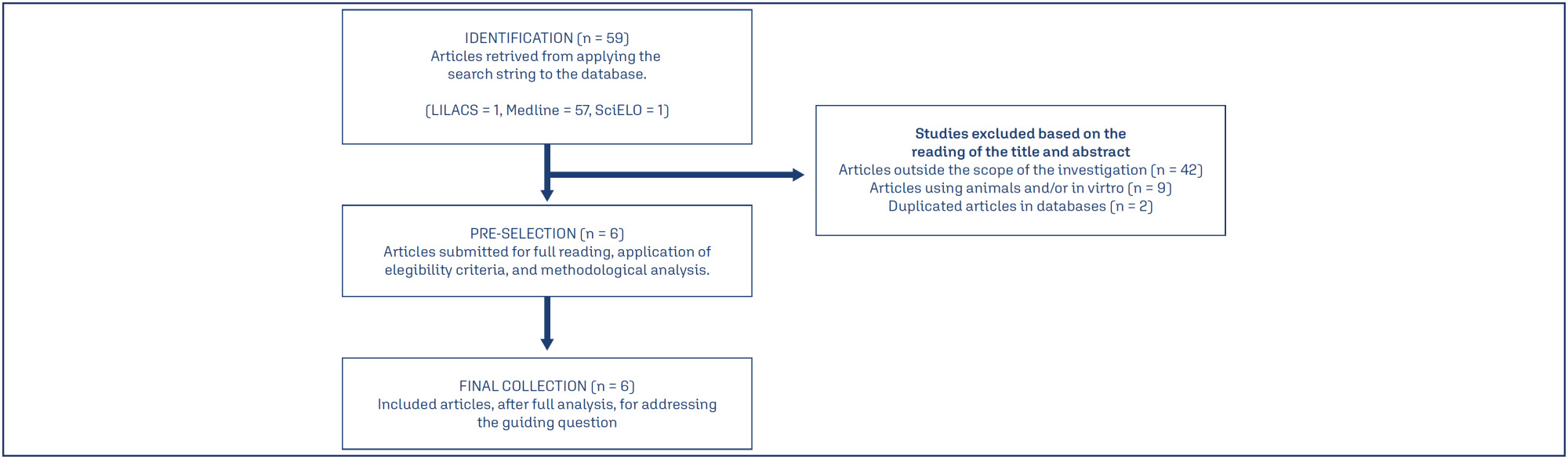
-
Review Article
Low-level laser therapy for nipple trauma and pain during breastfeeding: systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo3
03-18-2025
Summary
Review ArticleLow-level laser therapy for nipple trauma and pain during breastfeeding: systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo3
03-18-2025Views130Abstract
Objective:
This study aimed to investigate the effect of low-level laser therapy (LLLT) on nipple trauma and pain during breastfeeding through a systematic review with a meta-analysis of selected studies.
Source of the data:
A thorough search was conducted on March 22, 2022, using the databases PubMed, SciELO, LILACS, PEDro, CINAHL, EMBASE, ScienceDirect, Scopus, Google Scholar, MEDLINE, the Cochrane Library, Clinical Trials, Web of Science, TRIP, DARE, and ProQuest. The search terms included various combinations of low-level laser therapy, nipple pain, nipple trauma, and breastfeeding.
Studies selection:
Out of 107 articles identified, only three controlled and randomized clinical trials was included. The extracted data encompassed breast and trauma characteristics, treatment types, outcomes (pain and healing process), evaluation tools, LLLT usage, laser brand, and parameters.
Data collection:
Data extraction was performed using RAYYAN for systematic reviews. The risk of bias in the studies was evaluated.
Data synthesis:
Pain was measured using the visual analog scale (VAS). The included studies did not use validated tools for assessing physical conditions. All studies employed LLLT with a 660-nm wavelength, though there were variations in equipment power, energy dose, and application methods. The meta-analysis revealed an average difference of −0.60 points (95% CI: −1.52 to 0.31) in the VAS pain scores between the LLLT and control groups. No heterogeneity was observed among the studies (I2=0%), indicating no significant difference in pain relief between LLLT (red light) and control groups.
Conclusion:
LLLT may offer a promising option for managing breastfeeding-related complications, though further research is required.
Key-words Breast feedingLaser therapyLow level light therapyLow-level laserNipple painNipple traumaNipplesSee more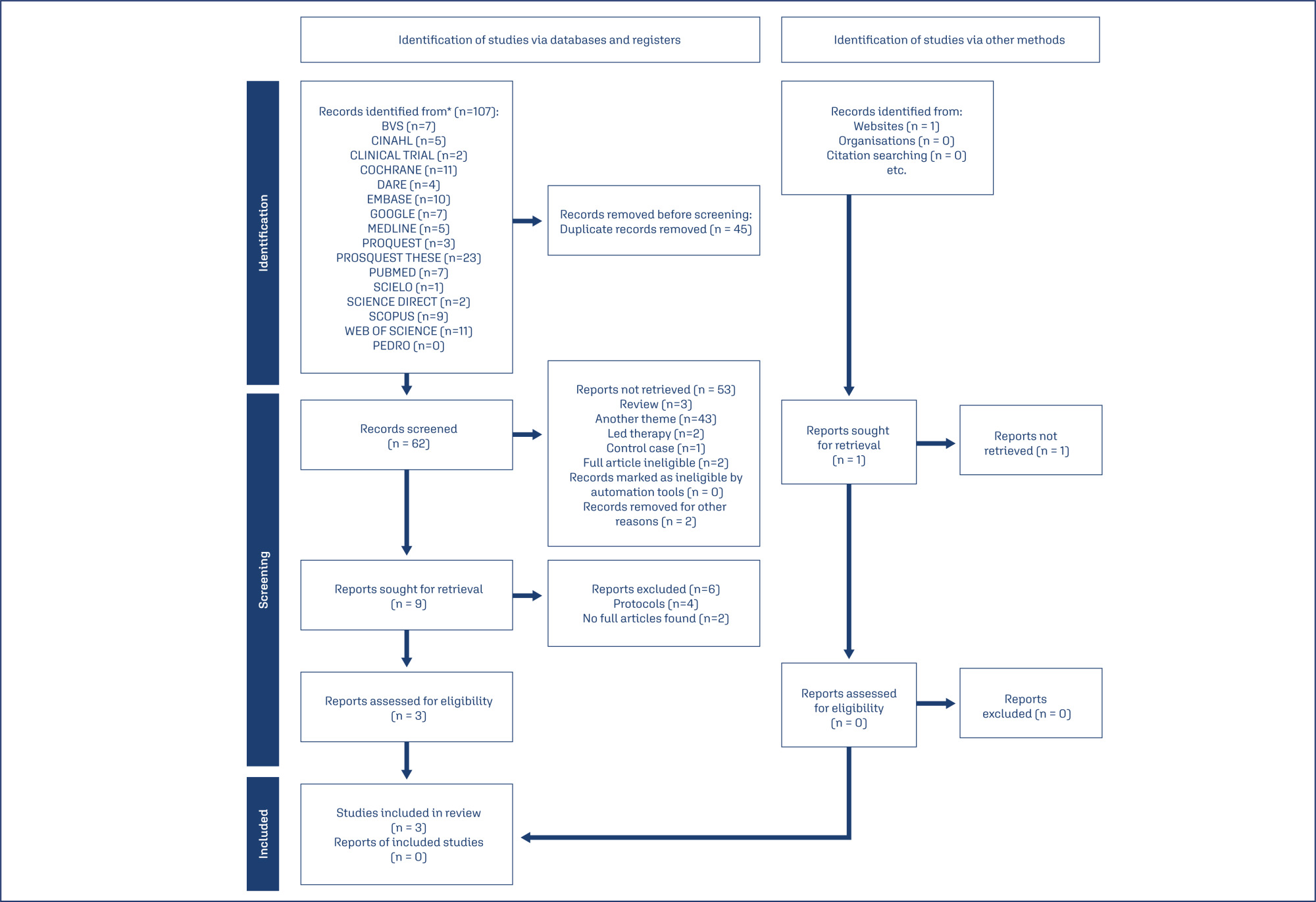
-
Review Article
Short cervix and use of cervical pessary for preventing preterm birth in singleton and twin pregnancies: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo10
03-18-2025
Summary
Review ArticleShort cervix and use of cervical pessary for preventing preterm birth in singleton and twin pregnancies: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo10
03-18-2025Views159See moreAbstract
Objective:
Preterm birth remains a significant contributor to neonatal morbidity and mortality. The use of cervical pessaries as an intervention for preventing preterm delivery in women with a short cervix has been a subject of interest. We evaluated the effectiveness of cervical pessary compared to standard care in preventing preterm delivery in women with a short cervix.
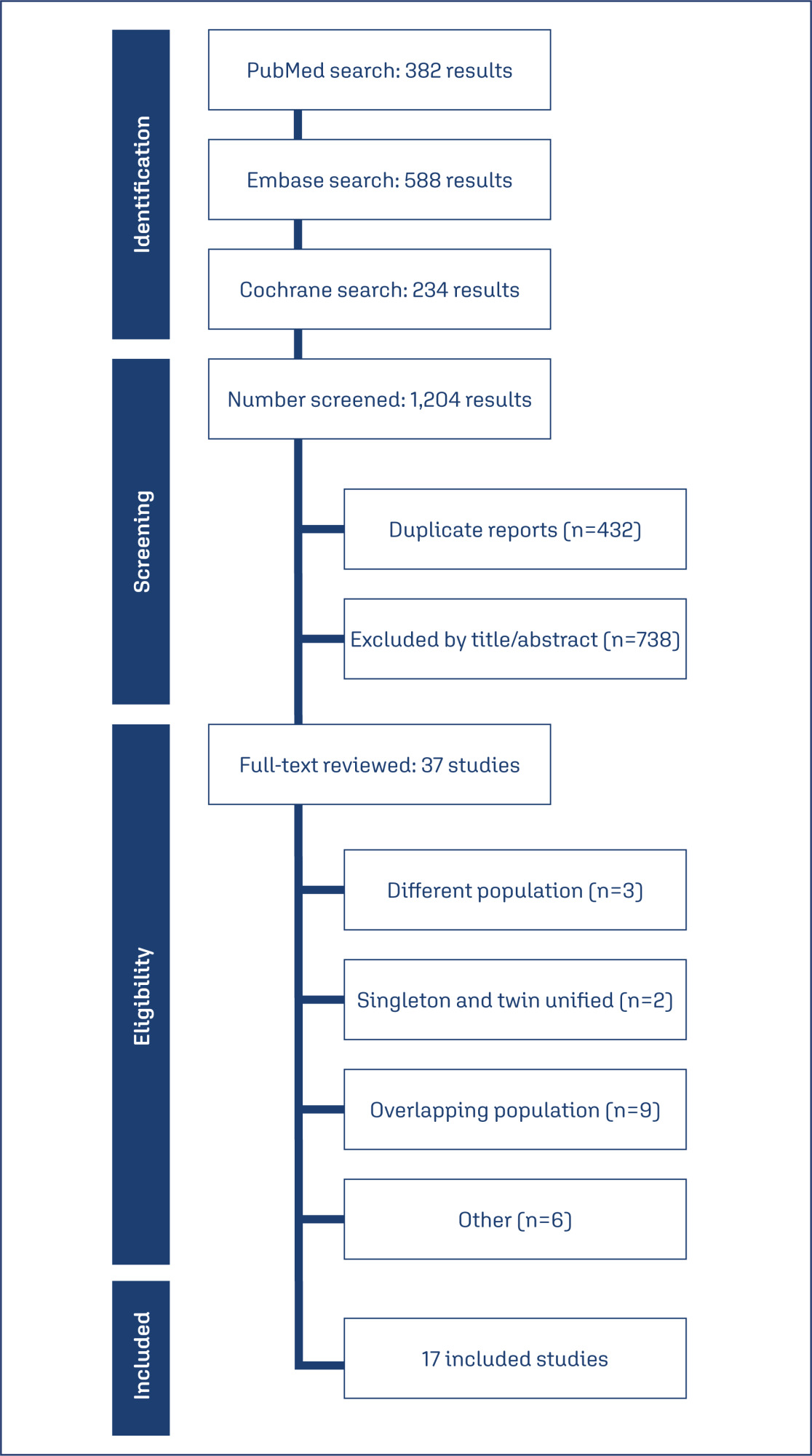
Data source:
Databases were systematically searched in PubMed, Cochrane, and Embase databases in December 2023.
Study selection:
Randomized clinical trials with the outcomes of interest were included.
Data collect:
We computed risk ratios for binary endpoints, with 95% confidence intervals. Heterogeneity was assessed using I2 statistics. Data were analyzed using R software (version 4.3.0). The primary outcomes of interest were preterm delivery before 37 weeks, and preterm delivery before 34 weeks.
Data synthesis:
Seventeen studies with 5,704 patients were included. The use of cervical pessary was associated with a decreased risk of preterm delivery before 37 (RR 0.88; 95% CI 0.81-0.96) and 34 weeks (RR 0.79; 95% CI 0.63-0.99) of gestation in twin pregnancies as compared to standard care without progesterone. There were no significant differences in preterm delivery in singleton pregnancy, neonatal outcomes, preterm premature rupture of the membranes or chorioamnionitis.
Conclusion:
The use of cervical pessary was associated with a significant reduction in preterm delivery at 34 and 37 weeks of gestation in twin pregnancies among patients with a short cervix compared to no treatment. No significant difference was found in singleton pregnancies or maternal outcomes.
-
Review Article
Zuranolone for postpartum depression: a systematic review and meta-analysis of two randomized studies
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo79
12-04-2024
Summary
Review ArticleZuranolone for postpartum depression: a systematic review and meta-analysis of two randomized studies
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo79
12-04-2024Views261See moreAbstract
Objective:
To evaluate the maternal outcomes in women with postpartum depression using zuranolone, the first oral medication indicated to treat postpartum depression.
Methods:
We conducted a systematic search in September 2023, on Pubmed, Embase and Cochrane Trials. We included randomized controlled trials comparing the effectiveness and safety of zuranolone versus placebo in women with postpartum depression. No time or language restrictions were applied. 297 results were retrieved, of which 11 papers were selected and fully reviewed by two authors. Review Manager 5 was used for statistical analysis and Cochrane Risk-of-bias tool for randomized trials was applied for quality assessment.
Results:
We included 2 studies, with 346 women, of whom 174 (50.2%) were treated with zuranolone. Zuranolone was significantly associated to an improvement of Clinical Global Impression response rate; Hamilton Depression Rating Scale 15 days and 45-day remission, 3-day, 15-day, and 45-day symptom remission, and reduction in the dose of antidepressants. As for safety outcomes, it was noticed that zuranolone increases sedation risk, which can be dose related. No significant differences were found for other adverse events.
Conclusion:
These findings suggest that zuranolone might present a safe and effective medication for out-of-hospital treatment of PPD. Sedation effects need to be further assessed.
-
Review Article
Female genital tract microbiome: the influence of probiotics on assisted reproduction
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo82
12-04-2024
Summary
Review ArticleFemale genital tract microbiome: the influence of probiotics on assisted reproduction
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo82
12-04-2024Views199Abstract
Assisted reproductive technology (ART) has been evolving since 1978, with the number of techniques performed increasing over the years. Despite continued advances, some couples continue to have difficulties getting pregnant, and it has recently been considered that the microbiome of the female genital tract (FGT) may influence embryo implantation and the establishment of pregnancy. This review aims to evaluate the role of probiotics on reproductive outcomes in infertile women on ART. A search throughout medical databases was performed, and six articles met the criteria. Five studies showed improvements in pregnancy rates, with only one demonstrating statistical significance. One article showed no improvement but reported a statistically significant reduction in the miscarriage rate in the probiotic group. Further research is needed to evaluate the true potential of probiotics, namely to assess whether they effectively modulate the FGT microbiome and if these changes are maintained over time.
Key-words Abortion, spontaneousEmbryo implantationGenitalia, femaleInfertility, femalePregnancy outcomePregnancy rateProbioticsReproductive techniques, assisted, MicrobiotaSee more


