Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(2):96-105
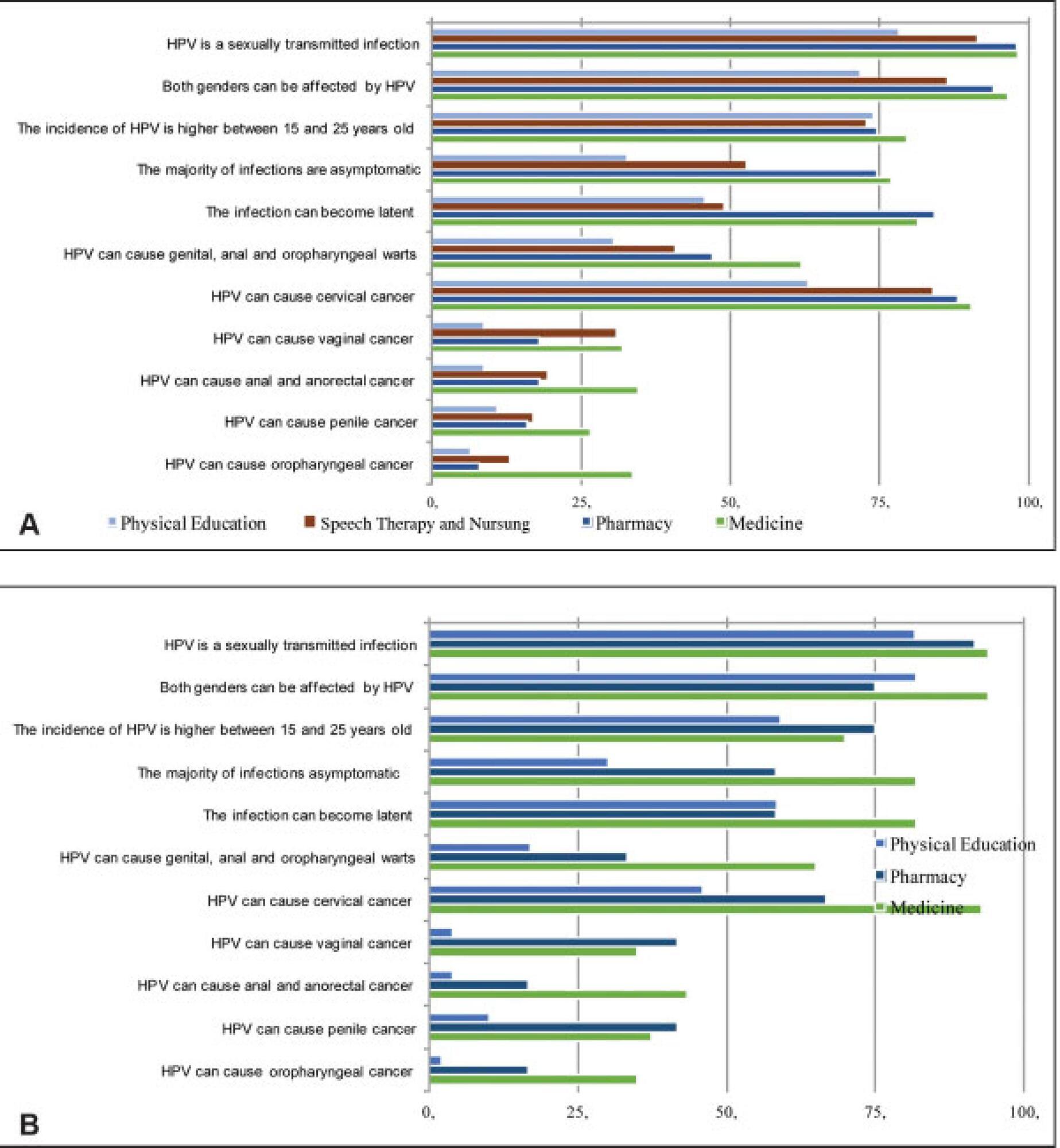
To evaluate the knowledge related to human papillomavirus (HPV) infection and the rate of HPV vaccination among undergraduate freshmen and senior students of medicine, pharmacy, speech therapy, nursing and physical education in a Brazilian university.
A questionnaire concerning sociodemographic aspects, sexual background, and knowledge about HPV and its vaccine was filled out by 492 students. Three months later, a second questionnaire, concerning the new rate of vaccination, was applied to 233 students.
Among the 290 women who answered the first questionnaire, 47% of the freshmen and 13% of the seniors stated they were not sexually active, as well as 11% of the 202 freshman and senior male students. Although the knowledge about HPV was higher among women, they reported a lower use of condoms. More than 83% of the women and 66% of the men knew that HPV can cause cervical cancer, but less than 30% of the students knew that HPV can cause vulvar, anal, penile and oropharyngeal cancer. Less than half of the students knew that HPV causes genital, anal and oropharyngeal warts. Comparing the students, the seniors had more knowledge of the fact that HPV is sexually transmitted, and that HPV infection can be asymptomatic. The rate of vaccination was of 26% for women, and of 8% for men, and it increased to 52% and 27% respectively among the 233 students evaluated in the second questionnaire.
As almost half of freshman women declared being sexually inactive, the investment in public health information programs and easier access to the HPV vaccine seem to be a useful strategy for undergraduate students.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(2):90-95
To describe clinical and sociodemographic characteristics of women with deep infiltrating endometriosis (DIE) and assess their quality of life (QOL) during 6 months of medical treatment.
A descriptive cross-sectional study of 60 women diagnosed with DIE either by surgery or image methods (ultrasound or magnetic resonance), who received clinical treatment for at least 6 months in the Universidade de Campinas, Campinas, state of São Paulo, Brazil. Both the SF-36 and the EHP-30 questionnaires were used to assess the quality of life.
The mean age of the patients was 37.7 ± 6.0 years old, with 50% presenting dysmenorrhea; 57% dyspareunia; and 50% chronic pelvic pain. The SF-36 and the EHP-30 revealed impaired quality of life. In the SF-36, the worst domains were limitation due to emotional aspects (40.2 ± 43.1) and self-esteem and disposition (46.1 ± 24.8), whereas in the EHP-30 they were social well-being (50.3 ± 30.6); infertility (48.0 ± 36.3); and sexual intercourse (54.0 ± 32.1).
Although clinically treated, women with deep endometriosis present impairment in different domains of quality of life regardless of the questionnaire used for evaluation.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(2):81-89
The present study aimed to analyze cardiac autonomic modulation via spectral and symbolic analysis of heart rate variability (HRV) in women with polycystic ovary syndrome (PCOS) who were subjected to two consecutive tilt tests.
A total of 64 women were selected and divided into 2 groups: control (without PCOS), and PCOS. Concentrations of follicle-stimulating hormone, luteinizing hormone, prolactin, estradiol, homocysteine, sex hormone-binding globulin, thyroid stimulating hormone, fasting insulin, testosterone, androstenedione, and 17-hydroxyprogesterone levels, triglycerides, free androgen index (FAI), and homeostasis assessment model (HOMA-IR) were assessed. Cardiac autonomic modulation was evaluated by spectral and symbolic analyses during two consecutive tilt tests (two moments) and supine moments before, between and after (three moments) the tilt tests.
Women with PCOS had higher fasting insulin, HOMA-IR indexes, testosterone and FAI. Additionally, we observed that the PCOS group had greater sympathetic autonomic cardiac modulation in supine 2, tilt 1, and supine 3 moments compared with controls.
Women with PCOS had higher autonomic sympathetic cardiac modulation even after a second tilt test. No adaptation to this provocative test was observed. Spectral analysis was more sensitive for identifying differences between groups than the symbolic analysis.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(2):74-80
To evaluate the impact of the presence of criteria for severe maternal morbidity and maternal near miss associated with hypertensive disorders on maternal and perinatal outcomes in a maternity school.
The present is a sub-analysis of a larger study involving 27 centers in Brazil that estimated the prevalence of serious maternal morbidity and near miss. It is an analytical and cross-sectional study with a quantitative approach, involving 928 women who were cared for at Maternidade Escola Assis Chateaubriand (MEAC, in Portuguese), Universidade Federal do Ceará (UFC, in Portuguese), from July 2009 to June 2010. The women were diagnosed with near miss according to the World Health Organization (WHO) criteria. The sample was divided into 2 groups: patients with (n = 827) and without hypertension (n = 101). The results were considered statistically significant when p < 0.05. The Pearson chi-squared and Fisher Exact tests were used for the categorical variables, and the Mann–Whitney U test was used for the continuous variables.
In total, 51 participants with maternal near miss criteria were identified, and 36 of them had hypertensive disorders. Of these, 5 died and were obviously excluded from the near miss final group. In contrast, we observed 867 cases with non-near miss maternal morbidity criteria. During this period, there were 4,617 live births (LBs) in the institution that was studied.
In the severe morbidity/maternal near miss population, the presence of hypertensive complications was prevalent, constituting a risk factor for both the mother and the fetus.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(2):67-73
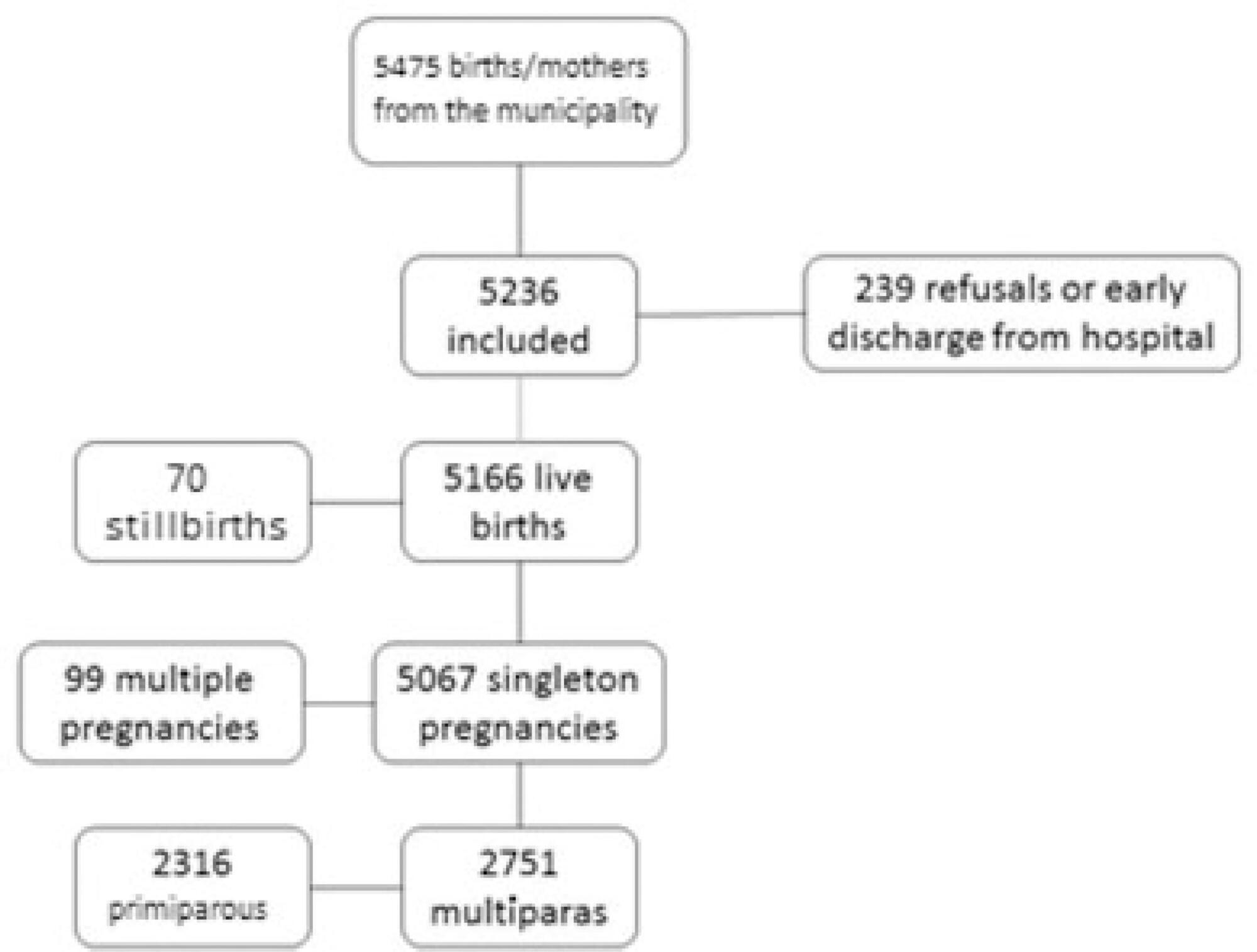
To determine the prevalence of inadequate birth interval and its associated factors in the BRISA study.
Cross-sectional study using data from the BRISA cohort. Birth interval was categorized into “adequate” (≥ 2 years or < 5 years between births), “short interval” (< 2 years) and “long interval” (≥ 5 years). The analysis of the factors associated with short and long birth intervals used multinomial logistic regression.
The prevalence of adequate birth intervals was 48.3%, of long intervals, 34.6%, and of short intervals, 17.1%. Skin color, age, education level, economic status, type of delivery, number of prenatal visits, parity, blood pressure, diabetes, and anemia (p-value was < 0.2 in the univariate analysis) proceeded to the final model. The variable ≥ 3 births (odds ratio [OR] = 1.29; confidence interval [CI]: 1.01–1.65) was associated with short intervals. Age < 20 years old (OR = 0.48; CI: 0.02–0.12) or ≥ 35 years old (OR = 2.43; CI: 1.82–3.25), ≥ 6 prenatal visits (OR = 0.58; CI: 0.47–0.72), ≥ 3 births (OR = 0.59; CI: 0.49–0.73), and gestational diabetes (OR = 0.38; CI: 0.20–0.75) were associated with long intervals.
Older mothers were more likely to have long birth intervals, and higher parity increases the chances of short birth intervals. Furthermore, gestational diabetes and adequate prenatal care presented higher chances of having adequate birth intervals, indicating that health assistance during pregnancy is important to encourage an adequate interval between gestations.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(12):718-725
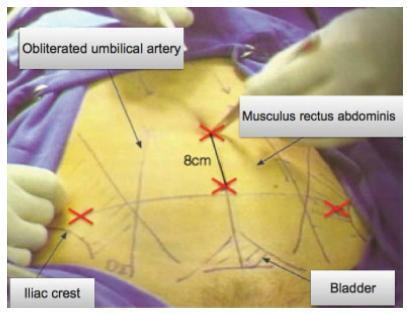
To evaluate the impact of systematic laparoscopic skills and suture training (SLSST) on the total laparoscopic hysterectomy intra- and postoperative outcomes in a Brazilian teaching hospital.
A cross-sectional observational study in which 244 charts of total laparoscopic hysterectomy (TLH) patients operated from 2008 to 2014 were reviewed. Patient-specific (age, parity, previous cesarean sections, abdominal surgeries and endometriosis) and surgery-related variables (hospital stay, operative time, uterine volume and operative complications) were analyzed in three different time-frame groups: 2008-09 (I-1) - TLHs performed by senior attending physicians; 2010-11 (I-2) - TLHs performed by residents before the implementation of the SLSST program; and 2012-14 (I-3) - TLHs performed by residents after the implementation of the SLSST program.
A total of 244 TLH patients (mean age: 45.93 years) were included: 24 (I-1), 55 (I-2), and 165 (I-3). The main indication for TLH was uterine myoma (66.4%). Group I-3 presented a decrease in surgical time compared to group I-2 (p=0.010). Hospital stay longer than 2 days decreased in group I-3 compared to group I-2 (p=0.010). Although we observed decreased uterine volume (154.2 cm3) in group I-2 compared to group I-1 (217.8 cm3) (p=0.030), logistic regression did not find any association between uterine volume and surgical time (p=0.103).
The total operative time for laparoscopic hysterectomy was significantly shorter in the group of patients (I-3) operated after the systematic laparoscopic skills and suture training was introduced in our hospital.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(12):710-717
To identify the biomarkers of response to neoadjuvant chemotherapy in early luminal breast cancer.
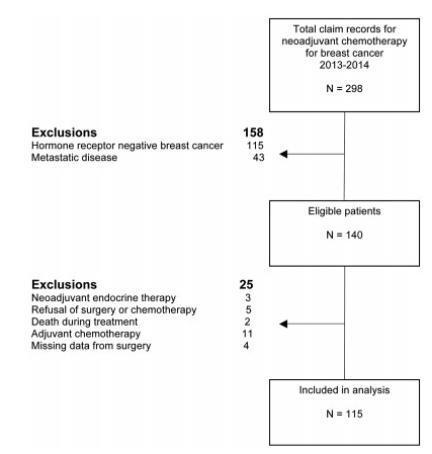
A cross-sectional study that included all patients with early or locallyadvanced luminal breast cancer submitted to neoadjuvant chemotherapy between 2013 and 2014. Demographic, clinic and pathologic data were retrieved from patient records. The expressions of the estrogen receptor (ER), the progesterone receptor (PR), and Ki67 were analyzed by immunohistochemistry (IHC). The status of the human epidermal growth factor receptor 2 (HER2) was evaluated by IHC and fluorescent in situ hybridization (FISH). Independent predictors of clinic and pathologic response were evaluated by stepwise logistic regression models and receiver operating characteristic (ROC) curve analysis.
Out of 298 patients identified, 115 were included in the analysis. Clinical complete response (cCR) was observed in 43.4% of the patients (49/113), and pathologic complete response (pCR) was observed in 7.1% (8/115) of the patients. The independent predictors of cCR were premenopausal status (p < 0.001), low PR expression (≤ 50% versus > 50%; p = 0.048), and Ki67 expression ≥ 14% (versus < 14%; p = 0.01). Patients with cCR were more commonly submitted to breast conserving surgery (34.7% versus 7.8%; p < 0.001). Increasing cut-off points for Ki67 expression were associated with an increase in specificity and a decrease in sensitivity to identify patients with cCR.
Premenopausal status, lower PR expression and higher Ki67 expression were associated with a higher rate of cCR to neoadjuvant chemotherapy in luminal breast cancer.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(12):697-702
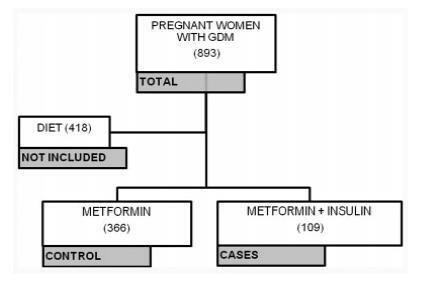
To evaluate the factors associated with the need for insulin as a complementary treatment to metformin in pregnant women with gestational diabetes mellitus (GDM).
A case-control study was performed from April 2011 to February 2016 with pregnant women with GDM who needed complementary treatments besides diet and physical exercise. Those treated with metformin were compared with those who, in addition to metformin, also needed the combination with insulin. Maternal characteristics and glycemic control were evaluated. Multinomial logistic regression models were developed to evaluate the influence of different therapies on neonatal outcomes.
A total of 475 pregnant women who needed pharmacological therapy were evaluated. Of these, 366 (77.05%) were submitted to single therapy with metformin, and 109 (22.94%) needed insulin as a complementary treatment. In the analysis of the odds ratio (OR), fasting glucose (FG)<90 mg/dL reduced the odds of needing the combination (OR: 0.438 [0.235-0.815]; p=0.009], as well as primiparity (OR: 0.280 [0.111-0.704]; p=0.007]. In obese pregnant women, an increased chance of needing the combination was observed (OR: 2,072 [1,063-4,039]; p=0,032).
Obesity resulted in an increased chance of the mother needing insulin as a complementary treatment to metformin, while FG<90 mg/dL and primiparity were protective factors.