Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(8):485-492
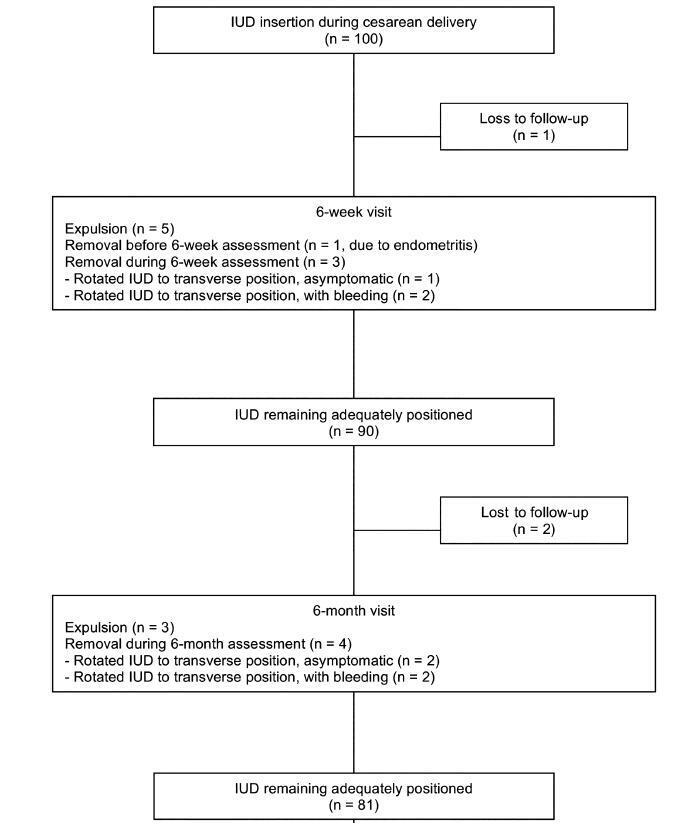
Themoment of admission for deliverymay be inappropriate for offering an intrauterine device (IUD) to women without prenatal contraception counseling. However, in countries with high cesarean rates and deficient prenatal contraception counseling, this strategy may reduce unexpected pregnancies and repeated cesarean sections.
This was a prospective cohort study involving 100 women without prenatal contraception counseling. Postplacental IUD was offered after admission for delivery and placed during cesarean. The rates of IUD continuation, uterine perforation, and endometritis were assessed at 6 weeks and 6 months, and the proportion of women continuing with IUD at 6 months was assessed with respect to the number of previous cesareans.
Ninety-seven women completed the follow-up. The rate of IUD continuation was 91% at 6 weeks and 83.5% at 6 months. The expulsion/removal rate in the first 6 weeks was not different from that between 6 weeks and 6 months (9 vs 9.1%, respectively). There were 2 cases of endometritis (2.1%), and no case of uterine perforation. Among 81 women continuing with intrauterine device after 6-months, 31% had undergone only the cesarean section in which the IUD was inserted, 44% had undergone 2 and 25% had undergone 3 or more cesarean sections.
Two thirds of the women who continued with IUD at 6 months had undergone 2 ormore cesarean sections. Since offering trial of labor is unusual after 2 or more previous cesareans, we believe that offering IUD after admission for delivery may reduce the risk of repeated cesarean sections and its inherent risks.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(8):476-484
Labor induction does not always result in vaginal delivery, and can expose both the mother and the fetus to the risks inherent to the induction procedure or a possible cesarean section. Transvaginal sonography (TVS) of the cervix is a useful tool to predict prematurity; in the present study, this tool was used to evaluate postterm induction.
We evaluated the ultrasound characteristics of the cervix (cervical length, cervical funneling, internal os dilation, the presence or absence of the cervical gland area [CGA], and the morphological changes of the cervix as a result of applying fundal pressure) before the onset of labor induction among women with postterm pregnancy to identify the possible predictors of failed labor induction. The Bishop score (BS) was used for comparison purposes. Three groups were evaluated: successful versus unsuccessful induction; vaginal delivery versus cesarean delivery (excluding cases of acute fetal distress [AFD]); and vaginal delivery versus cesarean delivery (including cases of AFD). A fourth group including only the primiparous women from the three previous groups was also evaluated.
Based on the studied characteristics and combinations of variables, a cervical length ≥ 3.0 cm and a BS ≤ 2 were the best predictors of induction failure.
Although TVS is useful for screening for induction failure, this tool should not be used as an indication for cesarean section.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(8):469-475
The aim of this study was to investigate the knowledge concerning gestational weight gain (GWG), nutrition, and physical exercise (PE) in pregnant women, and how to put them into practice.
A cross-sectional study with 61 pregnant women above 26 weeks of gestation, at the Woman’s Hospital, CAISM, University of Campinas. Questionnaires regarding the knowledge of healthy habits (HH) during pregnancy, sociodemographic data, and previous obstetric outcomes were applied. An educational guide with advice on HH during pregnancy and in the postpartum period was offered.
The average age of women was 28.7 ± 6.23 years, with 85% of them being married; 32% nulliparous; the average body mass index (BMI) before pregnancy was 25.4 ± 9.8 kg/m2, and themean number of years of schoolingwas 11.2 ± 3.8. Only 61%of the subjects had received any previous information about GWG during their antenatal care and were aware as to howmany pounds they should gain during pregnancy. Among the 61 women, 85% understood that they did not need to “eat for 2” and 99% knew that PE had benefits for their body and was safe for their baby. Half of the women practiced PE prior to pregnancy; however, only 31% continued the practice of PE during the pregnancy.
Despite understanding the need for HH during pregnancy, women still need encouragement to practice PE during pregnancy, as well as more information about GWG.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):249-255
The present study aimed to examine which development indicators are correlated with cervical cancer (CC) mortality rates in Brazil.
This was an ecological study that correlatedmortality rates and indicators, such as human development index (HDI), gross domestic product (GDP) per capita, illiteracy rate, fertility rate, screening coverage, proportion of private health insurance use, density of physicians, and density of radiotherapy centers. Themortality rateswere obtained fromthe Brazilian national registry, while the indicators were based on official reports from the Ministry of Health. Univariate and multivariate linear regression was used.
Among the states of Brazil, the average age-specific CC mortality rate from 2008 to 2012 varied from 4.6 to 22.9 per 100,000 women/year. In the univariate analysis, HDI, proportion of private health insurance use, density of physicians, and density of radiotherapy centers were inversely correlated with the mortality rates. Fertility rate was positively correlated with the mortality rates. In the multivariate analysis, only fertility rate was significantly associated with the CC mortality rate (coefficient of correlation: 9.38; 95% confidence interval [CI]: 5.16-13.59).
A decrease in the fertility rate, as expected when the level of development of the regions increases, is related to a decrease in the mortality rate of CC. The results of the present study can help to better monitor the quality assessment of CC programs both among and within countries.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):242-248
To analyze the factors associated with health-related quality of life (HRQoL) in women with cervical cancer (CC) in a single center in Rio de Janeiro, state of Rio de Janeiro, Brazil.
A cross-sectional study in women with a diagnosis of CC followed-up in the gynecology outpatient clinic of the Hospital do Câncer II (HCII, in the Portuguese acronym) of the Instituto Nacional de Câncer (INCA, in the Portuguese acronym). The data were collected from March to August 2015. Women with palliative care, communication/cognition difficulty, undergoing simultaneous treatment for other types of cancer, or undergoing chemotherapy and/or radiation therapy were excluded. For the evaluation of the HRQoL, a specific questionnaire for women with CC was used (Functional Assessment of Cancer Therapy - Cervix Cancer [FACT-Cx]). The total score of the questionnaire ranges from 0 to 168, with higher scores indicating a better HRQoL.
A total of 115 women were included in the present study, with a mean age of 52.64 years old (standard deviation [SD] = 12.13). The domains of emotional (16.61; SD = 4.55) and functional well-being (17.63; SD = 6.15) were those which presented the worst scores. The factors that had an association with better HRQoL in women with CC were having a current occupation, a longer time since the treatment and diagnosis, and women who had undergone hysterectomy.
Considering the domains of HRQoL of the women treated for cervical cancer, a better score was observed in the domains of physical and social/family wellbeing. For most domains, better scores were found between those with a current occupation, with a longer time after the diagnosis and treatment, and among those who had undergone a hysterectomy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):236-241
To compare sexual function and quality of life (QOL) among intrauterine contraceptive (copper-intrauterine device [Cu-IUD] or the 52-mg 20 μg/day levonorgestrel- releasing intrauterine system [LNG-IUS]) users.
This was part of a cross-sectional study. Women aged between 18 and 49 years old, in a heterosexual relationship, reporting sexual intercourse in the previous 4 weeks, using Cu-IUD (Group 1) or LNG-IUS (Group 2) responded to a questionnaire with sociodemographic information, to the Female Sexual Function Index (FSFI), to the World Health Organization QOL Questionnaire Abbreviated Version (WHOQOL-BREF), and to a questionnaire about the contraceptive method used. The Student t-test, the Pearson χ2 test or the Fisher exact test, and the Mann-Whitney test were used for the analysis. For the adjusted comparison, we have used the analysis of covariance (ANCOVA). A multiple regression analyzing factors related to FSFI 26.55 was done. Significance was established at p < 0.05.
A total of 347 women in Group 1 (mean age of 32.3 ± 7.5 years old) and of 298 in Group 2 (mean age of 32.7 ± 6.4 years old) completed the questionnaires.Most women had ≥ 8 years of schooling, were in amonogamous relationship, and had had ≤ 2 pregnancies. A total of 122 Cu-IUD and of 87 LNG-IUS users scored ≤ 26.55 on the FSFI. Significant lower scores in physical, environmental, and overall QOL domains in the WHOQOL-BREF questionnaire were found in Group 1. More women using the Cu- IUD were not satisfied with the method.
We did not find significant differences in sexual function; there was a lower score in some domains of QOL among women who used the Cu-IUD. It was not possible to ensure that those differences were related to the contraceptive method.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):230-235
To assess the perinatal and maternal outcomes of pregnant women with cystic fibrosis (CF) and severe lung impairment.
This was a series of cases aiming to review the maternal and fetal outcomes in cases of singleton pregnant women with a diagnosis of CF. We have included all of the cases of singleton pregnancy in patients with CF who were followed-up at the obstetrics department of the Medical School of the Universidade de São Paulo, between 2003 and 2016. The exclusion criteria were the unattainability of the medical records of the patient, and delivery at other institutions. A forced expiratory volume in 1 second < 50% was considered as severe lung impairment. We have also analyzed data regarding maternal hospitalization and respiratory exacerbations (REs).
Pregnant women with CF and severe lung impairment did not present an association with spontaneous prematurity, fetal growth restriction or fetal demise. All of the cases involved multiple RE episodes requiring antibiotic therapy. The median (range) of events per patient was of 4 (2-4) events.
Cystic fibrosis patients with severe lung impairment may achieve successful term pregnancies. However, pregnancies of women with CF are frequently complicated by REs, and this population may require hospital admission during the course of the pregnancy. Cystic fibrosis patients should be followed by a specialized team with experience in treating respiratory diseases.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):213-219
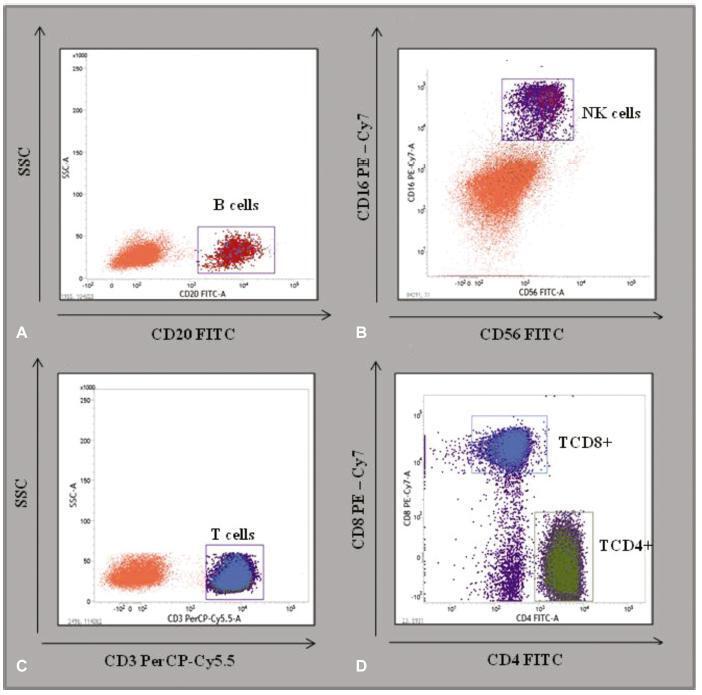
To describe the immunological and hematological reference intervals of low-risk pregnant women.
A cross-sectional retrospective database analysis of a basic and translational study analyzing the hematological evaluation blood counts and immunophenotyping of TCD3 + , TCD4 + , TCD8 + , B, and natural killer (NK) cells of the peripheral blood in 79 low-risk pregnant women and of 30 control women from the state of Pernambuco, Brazil, was performed.
No significant differences were detected between the hematological profiles of the 2nd and 3rd trimesters. Nevertheless, the median level of B cells decreased significantly in the 2nd (174 x 103 μL; p < 0.002) and 3rd trimesters (160 x 103 μL; p < 0.001), compared with the control group (296 x 103 μL). Similarly, the median level of NK cells was lower in the 2nd (134 x 103 μL; p < 0.0004) and 3rd trimesters (100 x 103 μL, p < 0.0004), compared with the control group (183 x 103 μL). In contrast, relative TCD4+ and TCD8+ levels increased in the 2nd and 3rd trimesters compared with the controls (TCD4 + : 2nd trimester = 59%; p < 0.001; 3rd trimester = 57%; p < 0.01; control = 50%; and TCD8 + : 2nd trimester = 31%; p < 0.001; 3rd trimester = 36%; p < 0.01; control = 24%).
Low-risk pregnant women have ~ 40% less B and NK cells in the peripheral blood, compared with non-pregnant women. These parameters may improve health assistance for mothers and contribute to define reference values for normal pregnancies.