Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(8):485-492
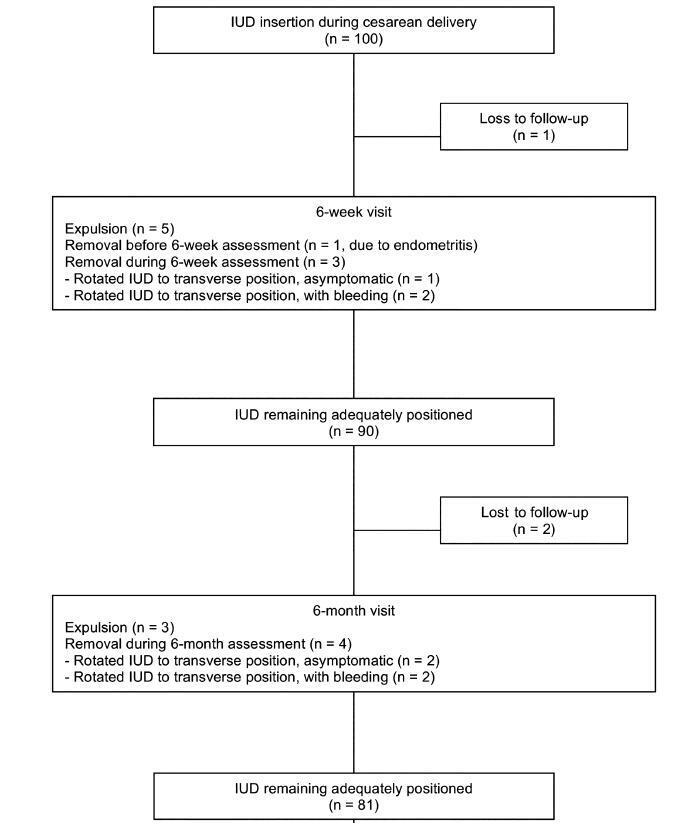
Themoment of admission for deliverymay be inappropriate for offering an intrauterine device (IUD) to women without prenatal contraception counseling. However, in countries with high cesarean rates and deficient prenatal contraception counseling, this strategy may reduce unexpected pregnancies and repeated cesarean sections.
This was a prospective cohort study involving 100 women without prenatal contraception counseling. Postplacental IUD was offered after admission for delivery and placed during cesarean. The rates of IUD continuation, uterine perforation, and endometritis were assessed at 6 weeks and 6 months, and the proportion of women continuing with IUD at 6 months was assessed with respect to the number of previous cesareans.
Ninety-seven women completed the follow-up. The rate of IUD continuation was 91% at 6 weeks and 83.5% at 6 months. The expulsion/removal rate in the first 6 weeks was not different from that between 6 weeks and 6 months (9 vs 9.1%, respectively). There were 2 cases of endometritis (2.1%), and no case of uterine perforation. Among 81 women continuing with intrauterine device after 6-months, 31% had undergone only the cesarean section in which the IUD was inserted, 44% had undergone 2 and 25% had undergone 3 or more cesarean sections.
Two thirds of the women who continued with IUD at 6 months had undergone 2 ormore cesarean sections. Since offering trial of labor is unusual after 2 or more previous cesareans, we believe that offering IUD after admission for delivery may reduce the risk of repeated cesarean sections and its inherent risks.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(8):493-499
To compare the Latin American and European assisted reproductive technology (ART) registries regarding data accessibility and quality, treatment utilization, effectiveness, safety, and quality of services.
We performed an ecological study using data from scientific publications of Latin American and European registries that report cycles initiated during 2013 (the most recent registries available until December of 2017). The summarized data are presented as frequencies, percentages, minimum-maximum values, and absolute numbers.
Reporting clinics and cycle treatments were unevenly distributed between the participating countries for both registries, although access to ART is 15 times greater in Europe. In Latin America, individual services participate voluntarily reporting started cycles until cancellation, birth or miscarriage, while in Europe it varied among countries. It makes the data available from Latin America more uniform, although lesser representative when compared with European ones, given that reporting is compulsory formost countries. The cumulative live birth rate was better in Latin America. Female age, use of intracytoplasmic sperm injection (ICSI), cycles with transfer of ≥ 3 embryos, as well as multiple pregnancy rates were greater in the Latin American Register of Assisted Reproduction (RLA, in the Portuguese acronym). Assisted reproductive technology complications, such as ovarian hyperstimulation syndrome, hemorrhage, and infections were also higher in LatinAmerica, although they are extremely uncommon in both regions.
Both regions have points to improve in the quality of their reports. Latin America has produced a more uniform reporting, their clinical results are generally
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(8):500-507
The present study was conducted with the objective of investigating the effectiveness of solution-focused group counseling (SFGC) on promoting the mental health of midwifery students.
The present study is an intervention-based study with a pretest, a post-test, and a control group. The statistical population included all of the midwifery students studying in the midwifery department of the Bam University of Medical Sciences, Kerman, Iran, who filled out the General Health Questionnaire (GHQ) in the screening phase. In the second phase, 40 individuals, having a low level of mental health based on the cutoff score of 23, were selected and randomly divided into 2 groups (intervention and control), each group with 20 participants. The intervention group participated in 5 sessions of 75 minutes for SFGC. Then, the post-test was held in both groups and the data analysis was conducted using the Mann-Whitney and the Kruskal-Wallis test with IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp, Armonk, NY, USA). The significance level was considered as p < 0.05.
The findings showed that the mean of the post-test mental health scores of the intervention group (14.5 ± 50.35) and of the control group (23.6 ± 35.83) showed a statistically significant difference (p < 0.0001). Moreover, the comparison between the mean scores of the mental health subscales (physical symptoms, stress, social performance, and depression) showed a statistically significant difference in these groups, and SFGC improved physical symptoms, stress, social performance, and depression in the members of the intervention group.
Solution-focused group counseling may improve all levels of mental health. This type of counseling is recommended to be used to solve the psychological problemsand to improve the mental health of students, as well as of the staff of the health system.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):213-219
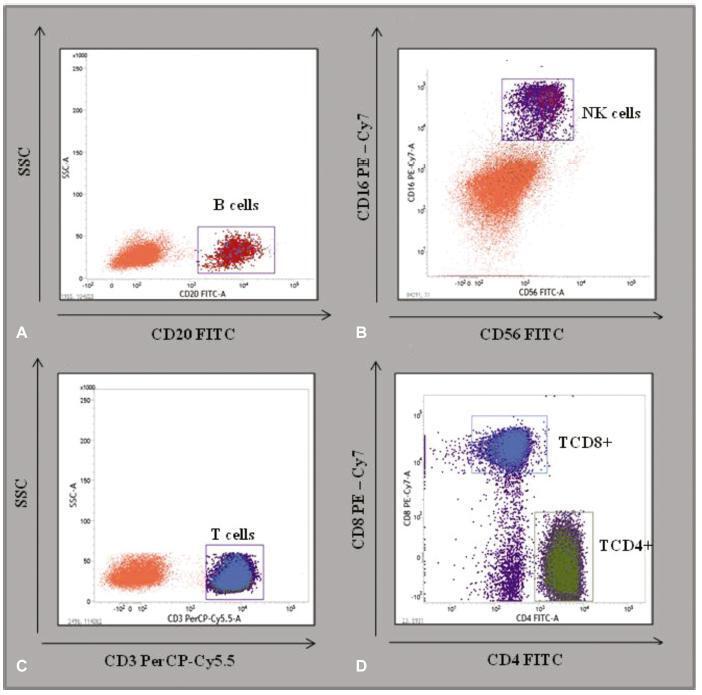
To describe the immunological and hematological reference intervals of low-risk pregnant women.
A cross-sectional retrospective database analysis of a basic and translational study analyzing the hematological evaluation blood counts and immunophenotyping of TCD3 + , TCD4 + , TCD8 + , B, and natural killer (NK) cells of the peripheral blood in 79 low-risk pregnant women and of 30 control women from the state of Pernambuco, Brazil, was performed.
No significant differences were detected between the hematological profiles of the 2nd and 3rd trimesters. Nevertheless, the median level of B cells decreased significantly in the 2nd (174 x 103 μL; p < 0.002) and 3rd trimesters (160 x 103 μL; p < 0.001), compared with the control group (296 x 103 μL). Similarly, the median level of NK cells was lower in the 2nd (134 x 103 μL; p < 0.0004) and 3rd trimesters (100 x 103 μL, p < 0.0004), compared with the control group (183 x 103 μL). In contrast, relative TCD4+ and TCD8+ levels increased in the 2nd and 3rd trimesters compared with the controls (TCD4 + : 2nd trimester = 59%; p < 0.001; 3rd trimester = 57%; p < 0.01; control = 50%; and TCD8 + : 2nd trimester = 31%; p < 0.001; 3rd trimester = 36%; p < 0.01; control = 24%).
Low-risk pregnant women have ~ 40% less B and NK cells in the peripheral blood, compared with non-pregnant women. These parameters may improve health assistance for mothers and contribute to define reference values for normal pregnancies.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):220-229
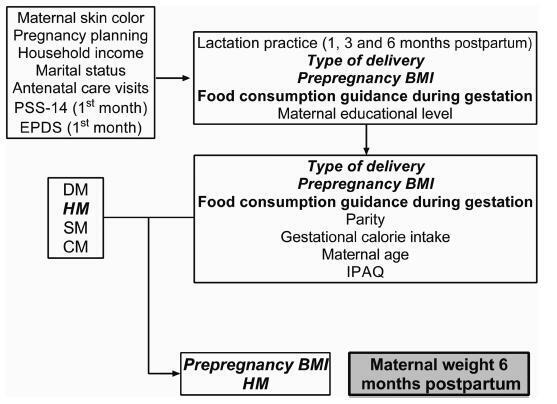
Different intrauterine environments may influence the maternal prepregnancy body weight (BW) variation up to 6 months postpartum. The objective of the present study was to verify the association of sociodemographic, obstetric, nutritional, and behavioral factors with weight variation in women divided into four groups: hypertensive (HM), diabetic (DM), smokers (SM), and control mothers (CM).
It was a convenience sample of 124 postpartum women recruited from 3 public hospitals in the city of Porto Alegre, state of Rio Grande do Sul, Brazil, between 2011 and 2016.Multiple linear regressions and generalized estimating equations (GEE) were conducted to identify the factors associated with maternal weight variation. For all GEE, the maternal weight measurements were adjusted for maternal height, parity, educational level, and the type of delivery, and 3 weight measurements (prepregnancy, preceding delivery, and 15 days postpartum) were fixed.
A hierarchical model closely associated the maternal diagnosis of hypertension and a prepregnancy body mass index (BMI) classified as overweight with maternal weight gain measured up to the 6th month postpartum (the difference between the maternal weight at 6months postpartum and the prepregnancy weight). These results showed that the BW of the HM group and of overweight women increased ~ 5.2 kg 6 months postpartum, compared with the other groups. Additionally, women classified as overweight had a greater BW variation of 3.150 kg.
This evidence supports the need for specific nutritional guidelines for gestational hypertensive disorders, as well as great public attention for overweight women in the fertile age.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):230-235
To assess the perinatal and maternal outcomes of pregnant women with cystic fibrosis (CF) and severe lung impairment.
This was a series of cases aiming to review the maternal and fetal outcomes in cases of singleton pregnant women with a diagnosis of CF. We have included all of the cases of singleton pregnancy in patients with CF who were followed-up at the obstetrics department of the Medical School of the Universidade de São Paulo, between 2003 and 2016. The exclusion criteria were the unattainability of the medical records of the patient, and delivery at other institutions. A forced expiratory volume in 1 second < 50% was considered as severe lung impairment. We have also analyzed data regarding maternal hospitalization and respiratory exacerbations (REs).
Pregnant women with CF and severe lung impairment did not present an association with spontaneous prematurity, fetal growth restriction or fetal demise. All of the cases involved multiple RE episodes requiring antibiotic therapy. The median (range) of events per patient was of 4 (2-4) events.
Cystic fibrosis patients with severe lung impairment may achieve successful term pregnancies. However, pregnancies of women with CF are frequently complicated by REs, and this population may require hospital admission during the course of the pregnancy. Cystic fibrosis patients should be followed by a specialized team with experience in treating respiratory diseases.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):236-241
To compare sexual function and quality of life (QOL) among intrauterine contraceptive (copper-intrauterine device [Cu-IUD] or the 52-mg 20 μg/day levonorgestrel- releasing intrauterine system [LNG-IUS]) users.
This was part of a cross-sectional study. Women aged between 18 and 49 years old, in a heterosexual relationship, reporting sexual intercourse in the previous 4 weeks, using Cu-IUD (Group 1) or LNG-IUS (Group 2) responded to a questionnaire with sociodemographic information, to the Female Sexual Function Index (FSFI), to the World Health Organization QOL Questionnaire Abbreviated Version (WHOQOL-BREF), and to a questionnaire about the contraceptive method used. The Student t-test, the Pearson χ2 test or the Fisher exact test, and the Mann-Whitney test were used for the analysis. For the adjusted comparison, we have used the analysis of covariance (ANCOVA). A multiple regression analyzing factors related to FSFI 26.55 was done. Significance was established at p < 0.05.
A total of 347 women in Group 1 (mean age of 32.3 ± 7.5 years old) and of 298 in Group 2 (mean age of 32.7 ± 6.4 years old) completed the questionnaires.Most women had ≥ 8 years of schooling, were in amonogamous relationship, and had had ≤ 2 pregnancies. A total of 122 Cu-IUD and of 87 LNG-IUS users scored ≤ 26.55 on the FSFI. Significant lower scores in physical, environmental, and overall QOL domains in the WHOQOL-BREF questionnaire were found in Group 1. More women using the Cu- IUD were not satisfied with the method.
We did not find significant differences in sexual function; there was a lower score in some domains of QOL among women who used the Cu-IUD. It was not possible to ensure that those differences were related to the contraceptive method.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):242-248
To analyze the factors associated with health-related quality of life (HRQoL) in women with cervical cancer (CC) in a single center in Rio de Janeiro, state of Rio de Janeiro, Brazil.
A cross-sectional study in women with a diagnosis of CC followed-up in the gynecology outpatient clinic of the Hospital do Câncer II (HCII, in the Portuguese acronym) of the Instituto Nacional de Câncer (INCA, in the Portuguese acronym). The data were collected from March to August 2015. Women with palliative care, communication/cognition difficulty, undergoing simultaneous treatment for other types of cancer, or undergoing chemotherapy and/or radiation therapy were excluded. For the evaluation of the HRQoL, a specific questionnaire for women with CC was used (Functional Assessment of Cancer Therapy - Cervix Cancer [FACT-Cx]). The total score of the questionnaire ranges from 0 to 168, with higher scores indicating a better HRQoL.
A total of 115 women were included in the present study, with a mean age of 52.64 years old (standard deviation [SD] = 12.13). The domains of emotional (16.61; SD = 4.55) and functional well-being (17.63; SD = 6.15) were those which presented the worst scores. The factors that had an association with better HRQoL in women with CC were having a current occupation, a longer time since the treatment and diagnosis, and women who had undergone hysterectomy.
Considering the domains of HRQoL of the women treated for cervical cancer, a better score was observed in the domains of physical and social/family wellbeing. For most domains, better scores were found between those with a current occupation, with a longer time after the diagnosis and treatment, and among those who had undergone a hysterectomy.