Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):190-199
To compare hand-held breast ultrasound (HHBUS) and automated breast ultrasound (ABUS) as screening tool for cancer.
A cross-sectional study in patients with mammographically dense breasts was conducted, and both HHBUS and ABUS were performed. Hand-held breast ultrasound was acquired by radiologists and ABUS by mammography technicians and analyzed by breast radiologists. We evaluated the Breast Imaging Reporting and
(BI-RADS) classification of the exam and of the lesion, as well as the amount of time required to perform and read each exam. The statistical analysis employed was measures of central tendency and dispersion, frequencies, Student t test, and a univariate logistic regression, through the odds ratio and its respective 95% confidence interval, and with p<0.05 considered of statistical significance.
Atotal of 440 patientswere evaluated. Regarding lesions,HHBUS detected 15 (7.7%) BI-RADS 2, 175 (89.3%) BI-RADS 3, and 6 (3%) BI-RADS 4, with 3 being confirmed by biopsy as invasive ductal carcinomas (IDCs), and 3 false-positives. Automated breast ultrasound identified 12 (12.9%) BI-RADS 2, 75 (80.7%) BI-RADS 3, and 6 (6.4%) BI-RADS 4, including 3 lesions detected by HHBUS and confirmed as IDCs, in addition to 1 invasive lobular carcinoma and 2 high-risk lesions not detected by HHBUS. The amount of time required for the radiologist to read the ABUS was statistically inferior compared with the time required to read the HHBUS (p<0.001). The overall concordance was 80.9%. A total of 219 lesions were detected, from those 70 lesions by both methods, 126 only by HHBUS (84.9% not suspicious by ABUS) and 23 only by ABUS.
Compared with HHBUS, ABUS allowed adequate sonographic study in supplemental screening for breast cancer in heterogeneously dense and extremely dense breasts.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):178-184
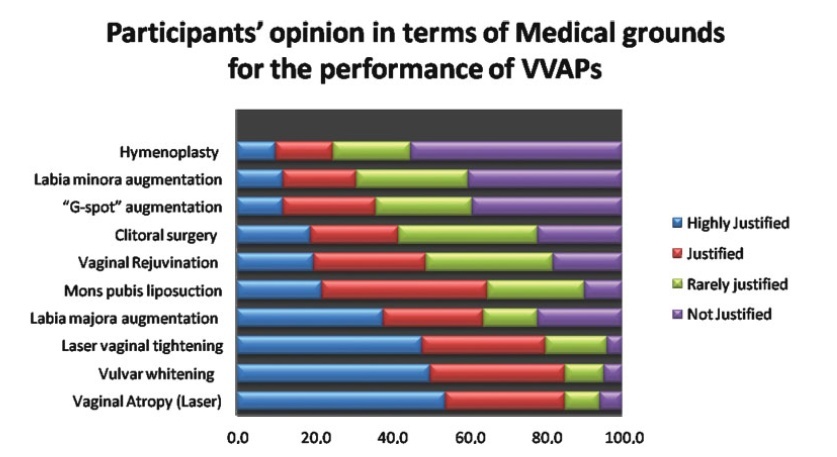
The present study aimed to explore the opinion and ethical consideration of vulvovaginal aesthetics procedures (VVAPs) among health professionals and medical students in Saudi Arabia.
This is a cross-sectional study performed between January 2020 and April 2020. Data was collected through electronic media, WhatsApp, and emails. The results were analyzed by applying the Students t-test, and correlations were considered significant if they presented a p-value<0.05.
There is significant demand to educate doctors, health professionals, medical students, and gynecologists for the VVAPs to have a solid foundation, justified indications, and knowledge about various aesthetic options. Although female doctors, medical students, young doctors, and gynecologists have more knowledge about VVAPs, all health professionals ought to be aware of recent trends in vulvovaginal aesthetics (VVA). The present analysis determined that VVA should be under the domain of gynecologists, rather than under that of plastic surgeons, general surgeons, and cosmetologists. Themajority of the participants considered that vaginal rejuvenation, “G-spot” augmentation, clitoral surgery, and hymenoplasty are not justifiable on medical grounds.
The decision to opt for different techniques for vaginal tightening and revitalization should be taken very carefully, utilizing the shared decision-making approach. Ethical aspects and moral considerations are important key factors before embarking in the VVAPs purely for cosmetic reasons. Further research is required to determine the sexual, psychological, and body image outcomes for women who underwent elective VVAPs. Moreover, medical educators must consider VVAPs as part of the undergraduate and postgraduate medical curriculum.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):172-177
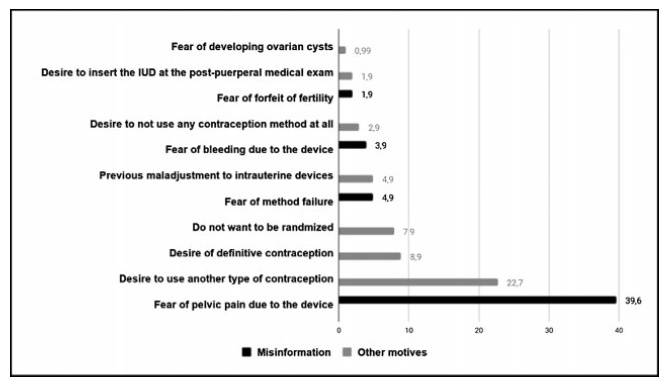
To evaluate the acceptability of postplacental placement of intrauterine devices (PPIUD), reasons for refusal and suggested policies to increase its use.
Cross-sectional study conducted at the Women Hospital of the Universidade de Campinas, Campinas, SP, Brazil. Postplacental placement of intrauterine devices was offered to women admitted in labor who did not present infections, uterinemalformation, twin pregnancy, preterm birth, and were at least 18 years old. In case of refusal, the parturient was asked to give their reasons and the answers were classified as misinformation about contraception or other reasons. The following were considered misinformation: fear of pain, bleeding, contraception failure and future infertility. Bivariate analysis was performed.
Amongst 241 invited women, the refusal rate was of 41.9%. Misinformation corresponded to 50.5% of all refusals, and the reasons were: fear of pain (39.9%); fear of contraception failure (4.9%); fear of bleeding (3.9%); fear of future infertility (1.9%); other reasons for refusal were 49.5%. Parturients aged between 18 and 27 years old refused the PPIUD more frequently due to misinformation (67.4%), and older parturients (between 28 and 43 years old) refused frequently due to other reasons (63.6%) (p=0.002). Themean age of those who declined the PPIUD due to misinformation was 27.3 ± 6.4 years old, while those who declined for other reasons had a mean age of 29.9 ± 5.9 years old (p=0.017).
The refusal of the PPIUD was high, especially amongst young women and due to misinformation. It is necessary to develop educative measures during antenatal care to counsel women about contraception, reproductive health and consequences of unintended pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):165-171
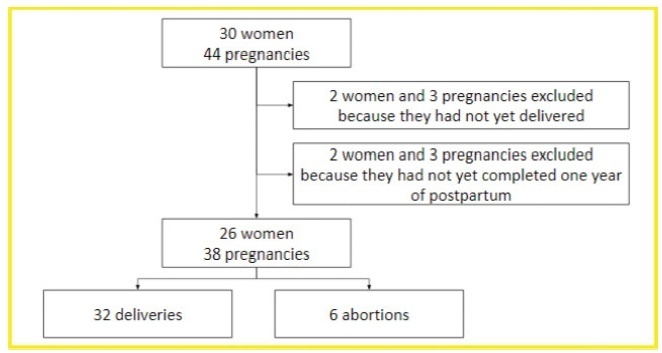
To describe the obstetric outcomes of patients withmultiple sclerosis (MS) and the impact of pregnancy and the postpartum period on the progression of the disease.
A case series study performed between December 2019 and February 2020, reporting pregnancies occurred between 1996 and 2019. The subjects included were women with MS undergoing follow-up at an MS referral center in Northeastern Brazil, and who had at least one pregnancy after the onset of MS symptoms, or who had their first relapse in the first year after delivery.
In total, 26 women and 38 pregnancies were analyzed - 32 of them resulted in delivery, and the remaining 6, in miscarriages. There was a significant increase in the prevalence of relapse during the postpartum period when compared with the gestational period. In 16 (42.1%) of the pregnancies, there was exposure to diseasemodifying therapies (DMTs) - 14 (36.8%), to interferon β, and 2 (5.3%), to fingolimod. Higher rates of abortion, prematurity and low birth weight were reported in the group was exposed to DMT when compared with the one who was not.
In the sample of the present study, there was a significant increase in the rate of MS relapse during the postpartum period when compared with the gestational period. Additionally, it seems that exposure to DMTs during pregnancy may affect the obstetric outcomes of the patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):297-303
To evaluate the number of patients with early-stage breast cancer who could benefit from the omission of axillary surgery following the application of the Alliance for Clinical Trials in Oncology (ACOSOG) Z0011 trial criteria.
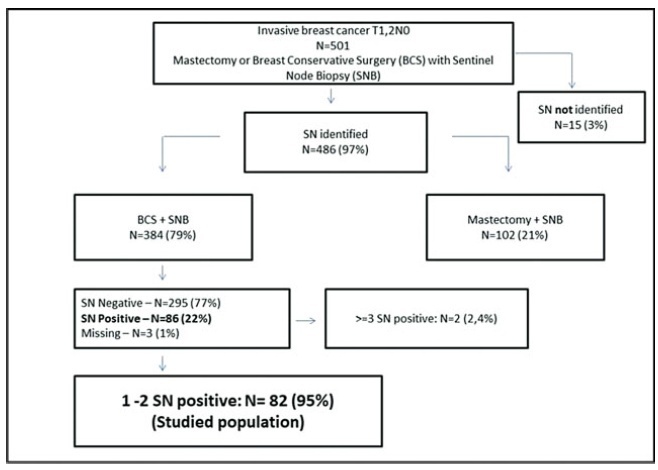
A retrospective cohort study conducted in the Hospital da Mulher da Universidade Estadual de Campinas. The study population included 384 women diagnosed with early-stage invasive breast cancer, clinically negative axilla, treated with breast-conserving surgery and sentinel lymph node biopsy, radiation therapy, chemotherapy and/or endocrine therapy, from January 2005 to December 2010. The ACOSOG Z0011 trial criteria were applied to this population and a statistical analysis was performed to make a comparison between populations.
A total of 384 patients underwent breast-conserving surgery and sentinel lymph node biopsy. Of the total number of patients, 86 women underwent axillary lymph node dissection for metastatic sentinel lymph nodes (SNLs). One patient underwent axillary node dissection due to a suspicious SLN intraoperatively, thus, she was excluded fromthe study. Among these patients, 82/86 (95.3%) had one to two involved sentinel lymph nodes andmet the criteria for the ACOSOG Z0011 trial with the omission of axillary lymph node dissection. Among the 82 eligible women, there were only 13 cases (15.9%) of lymphovascular invasion and 62 cases (75.6%) of tumors measuring up to 2 cm in diameter (T1).
The ACOSOG Z0011 trial criteria can be applied to a select group of SLNpositive patients, reducing the costs and morbidities of breast cancer surgery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):250-255
To investigate the effect of closure types of the anterior abdominal wall layers in cesarean section (CS) surgery on early postoperative findings.
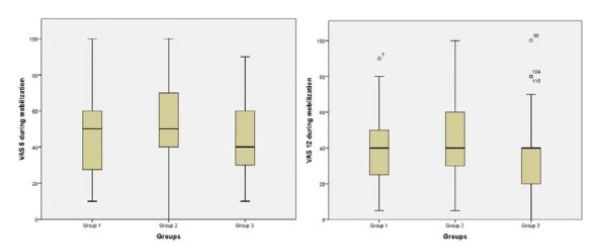
The present study was designed as a prospective cross-sectional study and was conducted at a university hospital between October 2018 and February 2019. A total of 180 patients who underwent CS for various reasons were enrolled in the study. Each patient was randomly assigned to one of three groups: Both parietal peritoneum and rectus abdominis muscle left open (group 1), parietal peritoneum closure only (group 2), and closure of the parietal peritoneum and reapproximation of rectus muscle (group 3). All patients were compared in terms of postoperative pain scores (while lying down and duringmobilization), analgesia requirement, and return of bowel motility.
The postoperative pain scores were similar at the 2nd, 6th, 12th, and 18th hours while lying down. During mobilization, the postoperative pain scores at 6 and 12 hours were significantly higher in group 2 than in group 3. Diclofenac use was significantly higher in patients in group 1 than in those in group 2. Meperidine requirements were similar among the groups. There was no difference between the groups’ first flatus and stool passage times.
In the group with only parietal peritoneum closure, the pain scores at the 6th and 12th hours were higher. Rectus abdominismuscle reapproximations were found not to increase the pain score. The closure of the anterior abdominal wall had no effect on the return of bowel motility.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):35-40
To evaluate the presence of residual disease in the uterine specimen after hysteroscopic polypectomy or polyp biopsy in patients with endometrioid endometrial cancer (EC).
We analyzed a series of 104 patients (92 cases from the Hospital AC Camargo and 12 from the Hospital do Servidor Público Estadual de São Paulo) with polyps that were diagnosed by hysteroscopy, showing endometrioid EC associated with the polyp or in the final pathological specimen. Patients underwent a surgical approach for endometrial cancer from January 2002 to January 2017. Their clinical and pathological data were retrospectively retrieved from the medical records.
In78cases (75%), thepolyphad EC, and in 40(38.5%), itwas restricted tothe polyp, without endometrial involvement. The pathologic stage was IA in 96 cases (92.3%) and 90 (86.5%) had histologic grade 1 or 2. In 18 cases (17.3%), there was no residual disease in the final uterine specimen, but only in 9 of them the hysteroscopy suggested that the tumor was restricted to the polyp. In 5 cases (4.8%) from the group without outside of the polyp during hysteroscopy, myometrial invasion was noted in the final uterine specimen. This finding suggests the possibility of disease extrapolation through the base of the polyp.
Patients with endometrioid EC associated with polyps may have the tumor completely removed during hysteroscopy, but the variables shown in the present study could not safely predict which patient would have no residual disease.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):3-8
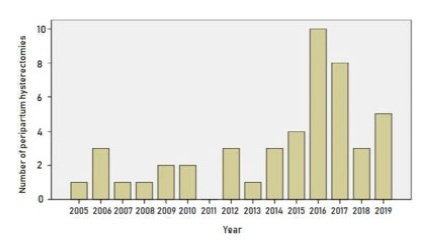
To determine the indications and outcomes of peripartum hysterectomies performed at Hospital de Clínicas de Porto Alegre (a university hospital in Southern Brazil) during the past 15 years, and to analyze the clinical characteristics of the women submitted to this procedure.
A cross-sectional study of 47 peripartum hysterectomies from 2005 to 2019.
The peripartum hysterectomies performed in our hospital were indicated mainly due to placenta accreta or suspicion thereof (44.7% of the cases), puerperal hemorrhage without placenta accreta (27.7%), and infection (25.5%). Total hysterectomies accounted for 63.8% of the cases, andwefound no differencebetween total versus subtotal hysterectomies in the studied outcomes. Most hysterectomies were performed within 24 hours after delivery, and they were associated with placenta accreta, placenta previa, and older maternal age.
Most (66.0%) patients were admitted to the intensive care unit (ICU). Those who did not need it were significantly older, and had more placenta accreta, placenta previa, or previous Cesarean delivery.