Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):871-877
This study aimed to evaluate the diagnostic profile of breast cancer cases during the coronavirus disease 2019 (COVID-19) pandemic compared with the previous year.
It is a retrospective study of cases diagnosed by a reference service in the public health system of Campinas, SP, Brazil. Two periods were analyzed: March to October 2019 (preCOVID period) and March to October 2020 (COVID-period). All women diagnosed during the periods were included. The Chi-Squared or Fisher exact and Mann-Whitney tests were used.
In the preCOVID and COVID periods, breast cancers were diagnosed, respectively, in 115 vs 59 women, and the mean ages at diagnosis were 55 and 57 years (p = 0.339). In the COVID period, the family history of breast cancer was more observed (9.6% vs 29.8%, p < 0.001), cases were more frequently symptomatic (50.4% vs 79.7%, p < 0.001) and had more frequently palpable masses (56.5% vs 79.7%, p = 0.003). In symptomatic women, the mean number of days from symptom to mammography were 233.6 (458.3) in 2019 and 152.1 (151.5) in 2020 (p = 0.871). Among invasive tumors, the proportion of breast cancers in stages I and II was slightly higher in the COVID period, although not significantly (76.7% vs 82.4%, p = 0.428). Also in the COVID period, the frequency of luminal A-like tumors was lower (29.2% vs 11.8%, p = 0.018), of triple-negative tumors was twice as high (10.1% vs 21.6%, p = 0.062), and of estrogen receptor-positive tumors was lower (82.2% vs 66.0%, p = 0.030).
During the COVID-19 pandemic, breast cancer diagnoses were reduced. Cases detected were suggestive of a worse prognosis: symptomatic women with palpable masses and more aggressive subtypes. Indolent tumors were those more sensitive to the interruption in screening.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(7):640-645
The present study seeks to identify the associated factors that increased primary cesarean delivery rates.
This was a cross-sectional study that evaluated the number of primary cesarean sections performed in the years 2006 and 2018 at the Hospital de Clínicas de Porto Alegre (HCPA, in the Portuguese acronym), through the collection of data from the medical records of the patients.
Advanced maternal age, twin pregnancy, and higher body mass index (BMI) became more frequent in 2018 in comparison with 2006. To mitigate the impact of confounding in comparisons among groups, we made an adjustment by propensity scores and detected significant differences when comparing both age groups on twin pregnancy rates, gestational diabetes mellitus, and thyroid disease.
Data from the present study can be used to prevent and improve the management of morbidities, impacting on better outcomes in obstetrical practice.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(7):660-666
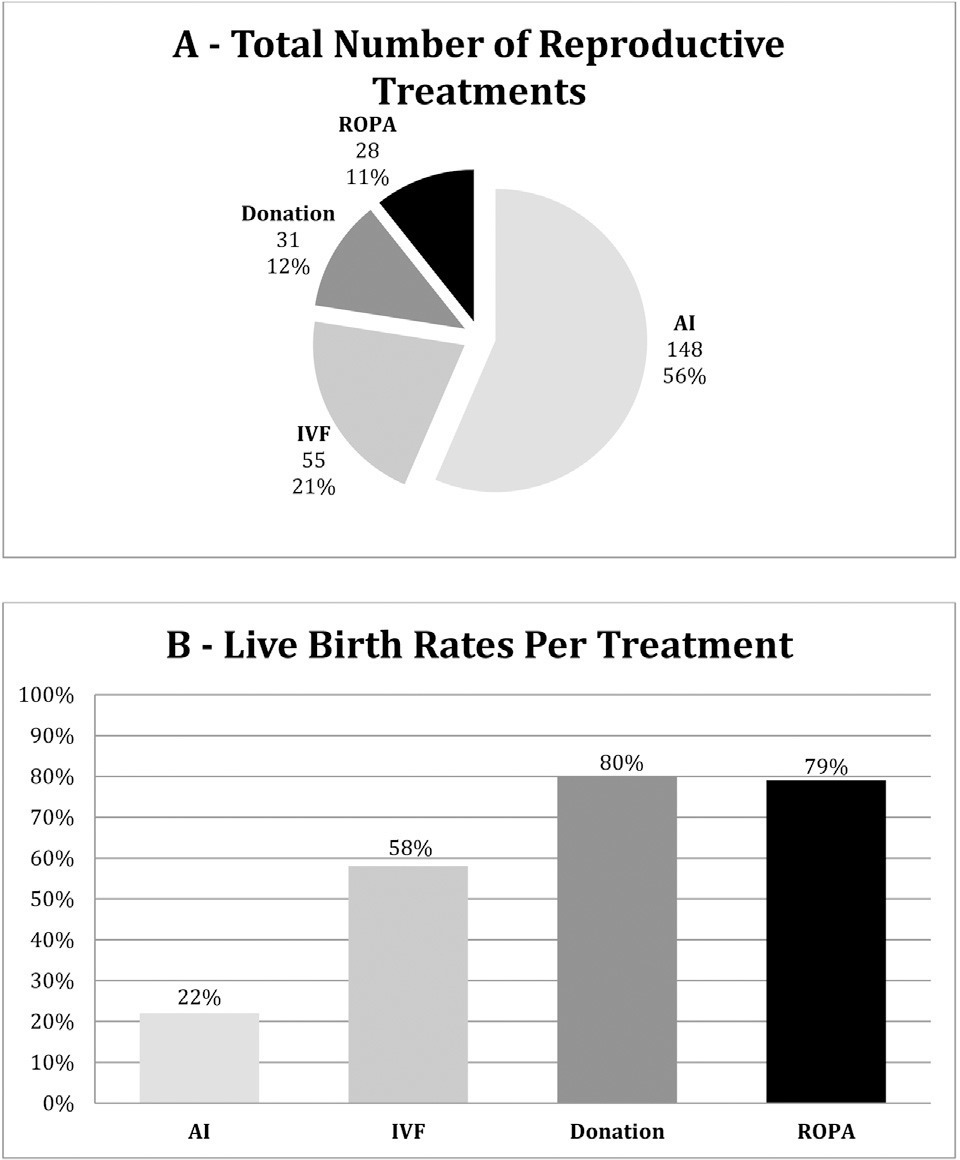
The present study aims to describe the main characteristics of female couples resorting to a fertility clinic, to understand whether these patients have clear previous plans concerning procreation and how they end up completing their family planning, and to briefly describe the main outcomes of the recepción de ovocitos de pareja (ROPA, in the Spanish acronym: in English, reception of partner's oocytes) method.
This is a descriptive retrospective study of the pathway and outcomes of female couples in a fertility clinic during a 2-year period.
A total of 129 couples were treated. Only one third of the couples had no condition potentially affecting fertility or advanced age. Most couples were decided to undergo artificial insemination or in vitro fertilization and the majority kept their plans, as opposed to 38% of the couples who decided to the ROPA method (lesbian shared in vitro fertilization) who changed plans. Live birth rates per treatment (including frozen embryo transfers) for artificial insemination, 58% for in vitro fertilization, 80% for treatments with donated oocytes or embryos, and 79% for ROPA. Four in five couples achieved live births.
The present study highlights the importance of a thorough medical workup in same-sex couples resorting to assisted reproduction. Despite the higher-than-expected rates of fertility disorders, the outcomes were good. Most couples end up in a single parented method. Furthermore, the results of the ROPA method are reassuring.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):567-572
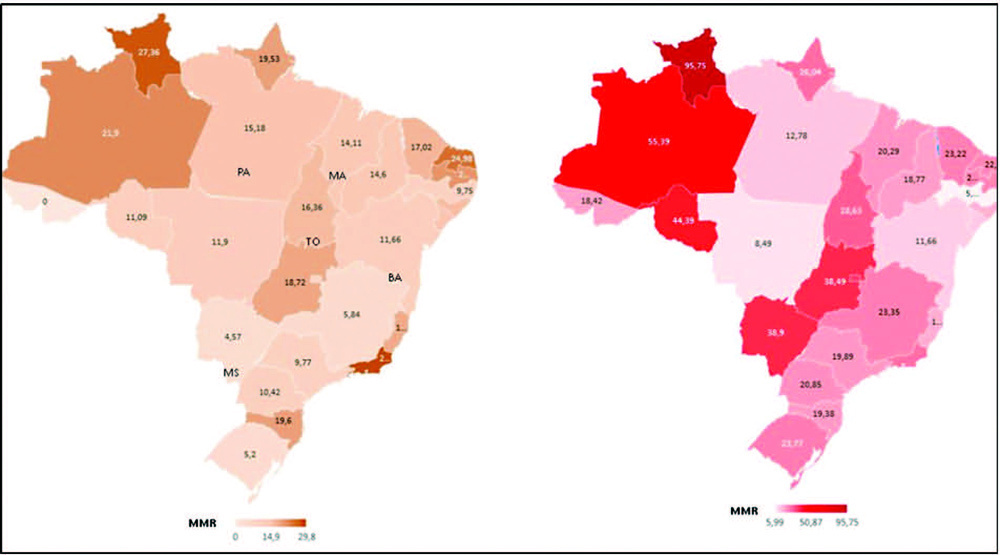
To compare death rates by COVID-19 between pregnant or postpartum and nonpregnant women during the first and second waves of the Brazilian pandemic.
In the present population-based evaluation data from the Sistema de Informação da Vigilância Epidemiológica da Gripe (SIVEP-Gripe, in the Portuguese acronym), we included women with c (ARDS) by COVID-19: 47,768 in 2020 (4,853 obstetric versus 42,915 nonobstetric) and 66,689 in 2021 (5,208 obstetric versus 61,481 nonobstetric) and estimated the frequency of in-hospital death.
We identified 377 maternal deaths in 2020 (first wave) and 804 in 2021 (second wave). The death rate increased 2.0-fold for the obstetric (7.7 to 15.4%) and 1.6-fold for the nonobstetric groups (13.9 to 22.9%) from 2020 to 2021 (odds ratio [OR]: 0.52; 95% confidence interval [CI]: 0.47–0.58 in 2020 and OR: 0.61; 95%CI: 0.56– 0.66 in 2021; p < 0.05). In women with comorbidities, the death rate increased 1.7-fold (13.3 to 23.3%) and 1.4-fold (22.8 to 31.4%) in the obstetric and nonobstetric groups, respectively (OR: 0.52; 95%CI: 0.44–0.61 in 2020 to OR: 0.66; 95%CI: 0.59–0.73 in 2021; p <0.05). In women without comorbidities, the mortality rate was higher for nonobstetric (2.4 times; 6.6 to 15.7%) than for obstetric women (1.8 times; 5.5 to 10.1%; OR: 0.81; 95%CI: 0.69–0.95 in 2020 and OR: 0.60; 95%CI: 0.58–0.68 in 2021; p <0.05).
There was an increase in maternal deaths from COVID-19 in 2021 compared with 2020, especially in patients with comorbidities. Death rates were even higher in nonpregnant women, with or without comorbidities.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(7):646-653
This study aims to describe the behavior of chromosomopathy screenings in euploid fetuses.
This is a prospective descriptive study with 566 patients at 11 to 14 weeks of gestation. The associations between ultrasound scans and serological variables were studied. For the quantitative variables we used the Spearman test; for the qualitative with quantitative variables the of Mann-Whitney U-test; and for qualitative variables, the X2 test was applied. Significance was set at p ≤ 0.05.
We have found that gestational age has correlation with ductus venosus, nuchal translucency, free fraction of β subunit of human chorionic gonadotropin, pregnancy-associated plasma protein-A and placental growth factor; there is also a correlation between history of miscarriages and nasal bone. Furthermore, we correlated body mass index with nuchal translucency, free fraction of β subunit of human chorionic gonadotropin, and pregnancy-associated plasma protein-A. Maternal age was associated with free fraction of β subunit of human chorionic gonadotropin and pregnancy-associated plasma protein-A.
Our study demonstrates for the first time the behavior of the biochemical and ultrasonographic markers of chromosomopathy screenings during the first trimester in euploid fetuses in Colombia. Our information is consistent with international reference values. Moreover, we have shown the correlation of different variables with maternal characteristics to determine the variables that could help with development of a screening process during the first trimester with high detection rates.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):573-577
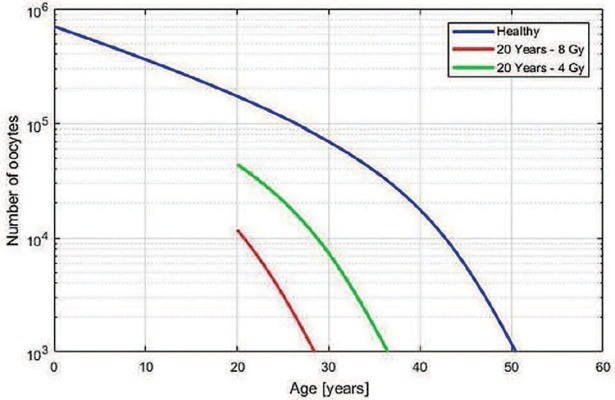
The present study aimed to develop a useful mathematical model that predicts the age at which premature ovarian insufficiency might occur after teletherapy radiation. A diagnosis of premature or early menopause has physical and psychological consequences, so women may need support and long-term medical follow-up.
To correlate ovarian radiation dose with ovarian function, we used the formula described by Wallace et al.: √g(z) = 10(2-0,15z), where “g(z)” and “z” represent oocyte survival rate and the radiation dose (in Gray), respectively. By simulating different ages and doses, we observed a pattern that could be used to simplify the relationship between radiation dose and remaining time of ovarian function.
We obtained a linear function between ovarian radiation dose and loss of ovarian function (LOF) that is the percentage of decrease in the time to the ovarian failure compared with the time expected for a woman at the same age without irradiation exposition. For patients <40 years old and with ovarian radiation doses < 5 Gy, the equation LOF = 2.70 + (11.08 × Dose) can be applied to estimate the decrease in time to premature ovarian insufficiency.
The present study reports a practicable theoretical method to estimate the loss of ovarian function. These findings can potentially improve the management and counseling of young women patients submitted to radiotherapy during their reproductive years.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):578-585
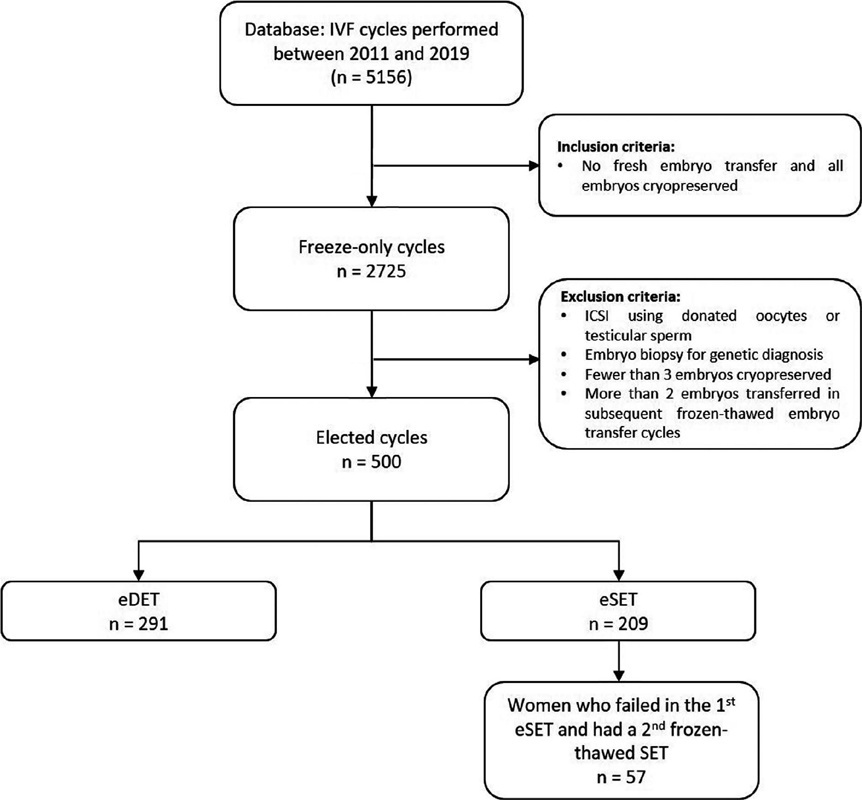
It is known that the single embryo transfer (SET) is the best choice to reduce multiples and associated risks. The practice of cryopreserving all embryos for posterior transfer has been increasingly performed for in vitro fertilization (IVF) patients at the risk of ovarian hyperstimulation syndrome or preimplantation genetic testing for aneuploidy. However, its widespread practice is still controverse. The aim of this study was to evaluate how effective is the transfer of two sequential SET procedures compared with a double embryo transfer (DET) in freeze-only cycles.
This retrospective study reviewed 5,156 IVF cycles performed between 2011 and 2019, and 506 cycles using own oocytes and freeze-only policy with subsequent elective frozen-thawed embryo transfers (eFET) were selected for this study. Cycles having elective SET (eSET, n = 209) comprised our study group and as control group we included cycles performed with elective DET (eDET, n = 291). In the eSET group, 57 couples who had failed in the 1st eSET had a 2nd eFET, and the estimated cumulative ongoing pregnancy rate was calculated and compared with eDET.
After the 1st eFET, the ongoing pregnancy rates were similar between groups (eSET: 35.4% versus eDET: 38.5%; p =0.497), but the estimated cumulative ongoing pregnancy rate after a 2nd eFET in the eSET group (eSET + SET) was significantly higher (48.8%) than in the eDET group (p < 0.001). Additionally, the eSET +SET group had a 2.7% rate of multiple gestations, which is significantly lower than the eDET group, with a 30.4% rate (p < 0.001).
Our study showed the association of freeze-only strategy with until up to two consecutive frozen-thawed eSETs resulted in higher success rates than a frozenthawed DET, while drastically reducing the rate of multiple pregnancies.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):467-474
Placenta accreta spectrum (PAS) is a serious diseases, and the recommendation is that the treatment is conducted in centers of excellence. Such hospitals are not easy to find in low- and middle-income countries. We seek to describe the process of prenatal diagnosis, surgical management, and postnatal histological analysis in a low-income country referral hospital with limited resources.
A descriptive, retrospective study was carried out including patients with a pre- or intraoperative diagnosis of PAS. The clinical results of the patients were studied as well as the results of the prenatal ultrasound and the correlation with the postnatal pathological diagnosis.
In total, 129 patients were included. Forty-eight of them had a prenatal PAS ultrasound diagnosis (37.2%). In the remaining 81 (62.8%), the diagnosis was intraoperative. Although hysterectomy was performed in all cases, one-third of the patients (31%) did not have a histological study of the uterus. In 40% of the patients who had a histological study, PAS was not reported by the pathologist.
The frequency of prenatal diagnosis and the availability of postnatal histological studies were very low in the studied population. Surgical skill, favored by a high flow of patients, is an important factor to avoid complications in settings with limited resources.