Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):465-470
To describe and evaluate the use of a simple, low-cost, and reproducible simulator for teaching the repair of obstetric anal sphincter injuries (OASIS).
Twenty resident doctors in obstetrics and gynecology and four obstetricians participated in the simulation. A fourth-degree tear model was created using lowcost materials (condom simulating the rectal mucosa, cotton tissue simulating the internal anal sphincter, and bovine meat simulating the external anal sphincter). The simulator was initially assembled with the aid of anatomical photos to study the anatomy and meaning of each component of the model. The laceration was created and repaired, using end-to-end or overlapping application techniques.
The model cost less than R$ 10.00 and was assembled without difficulty, which improved the knowledge of the participants of anatomy and physiology. The sutures of the layers (rectal mucosa, internal sphincter, and external sphincter) were performed in keeping with the surgical technique. All participants were satisfied with the simulation and felt it improved their knowledge and skills. Between 3 and 6 months after the training, 7 participants witnessed severe lacerations in their practice and reported that the simulation was useful for surgical correction.
The use of a simulator for repair training in OASIS is affordable (low-cost and easy to perform). The simulation seems to improve the knowledge and surgical skills necessary to repair severe lacerations. Further systematized studies should be performed for evaluation.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):458-464
Intraoperative frozen section (IFS) is a valuable resource, and its use in gynecological pathology has not been sufficiently emphasized. The main goal of the present study is to evaluate the reliability and agreement rates between IFS and the final paraffin section (PS) and determine how reliable IFS is.
A retrospective study of all IFSs performed on uterine tumors and suspicious adnexal masses between January 2012 and December 2016 (excluding metastases) at the department of obstetrics and gynecology of the Centro Hospitalar Tondela Viseu. Frozen versus permanent section diagnosis were compared regarding the histologic type of the tumor, and the depth of myometrial invasion.
A total of 286 cases were eligible for the present study, including 102 (35.7%) IFSs of uterine tumors, and 184 (64.3%) IFSs of ovarian tumors. The overall rate of deferred cases was 5.2% (15/286). The accuracy of the diagnosis in cases of endometrial carcinoma was 96.25% (77/80). Among the ovarian tumors, misdiagnoses occurred in 2 cases (1.1%), corresponding to a borderline tumor (serous type) and a clear cell intracystic adenocarcinoma.
The IFS analysis plays an important role in selected situations and is associated to a high sensitivity and specificity in cases of ovarian and endometrial tumors. Its high accuracy is almost universally associated with the possibility of obtaining an optimal surgical treatment at the time of the first surgical approach.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):450-457
The present study aims to investigate the association between caspase-8 (CASP8) (rs13416436 and rs2037815) and Fas cell surface death receptor (FAS) (rs3740286 and rs4064) polymorphisms with endometriosis in Brazilian women.
In the present case-control study, 45 women with a diagnosis of endometriosis and 78 normal healthy women as a control group were included. The genotyping was determined by real-time polymerase chain reaction (PCR) with Taqman hydrolysis probes (Thermo Fisher Scientific, Darmstadt, Germany). Genotypic and allelic frequencies were analyzed using Chi-squared (χ2) test. In order to determine the inheritance models and haplotypes ,SNPStats (Institut Català d’Oncologia, Barcelona, Spain) was used. Levels of 5% (p = 0.05) were considered statistically significant.
No significant difference was observed in genotypic or allelic frequencies between control and endometriosis groups for rs13416436 and rs2037815 (CASP8 gene). On the other hand, a significant difference between rs3740286 and rs4064 (FAS gene) was found. Regarding polymorphisms in the FAS gene, a statistically significant differencewas found in co-dominant and dominantmodels. Only the haplotype containing the rs3740286A and rs4064G alleles in the FAS gene were statistically significant.
The polymorphisms in the CASP8 gene were not associated with endometriosis. The results indicate an association between FAS gene polymorphisms and the risk of developing endometriosis.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):444-449
To identify maternal factors associated with the presence of low birth weight in term neonates.
Matched hospital-based case-controlled study performed in a high complexity institution located in the city of Neiva, Colombia. The study included women with term gestation and singleton live fetuses. Patients with prior diseases, coming from other regions, with pregnancy resulting from assisted reproduction, or with a diagnosis of fetal abnormality or aneuploidy were excluded. Low birth weight was the dependent variable, and the independent variables that were analyzed were maternal sociodemographic and clinical characteristics. Adjusted and non-adjusted odds ratios (aOR and OR) together with the 95% confidence intervals (95% CI) were reported.
The study included 270 participants (90 cases and 180 controls). Controlling for maternal age, educational level, socioeconomic and civil status, social security and the presence of maternal disease during gestation, it was found that weight gain (aOR 0.77, 95% CI 0.70-0.85) and the absence of prenatal care (aOR 8.20, 95% CI 3.22-20.87) were among the factors associated with low birth weight.
The absence of weight gain and of prenatal care are factors associated with the presence of low birth weight in term neonates and should be considered in clinical practice.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):437-443
To evaluate the social, obstetric and psychological risk factors related to repeat pregnancy in teenagers.
A case control study conducted at Centro de Atenção à Saúde Integral da Mulher (Caism, in the Portuguese acronym), in Campinas, Brazil, from 2015 to 2017. Three groups were selected: a case-group of adolescents who had repeat pregnancy and two control-groups, one consisting of adolescents who had delivered at first time and another one of adult women with more than one deliveries. Participants were asked about habits, socio-demographics characteristics, reproductive and obstetric history and assessed psychological issues.
Ninety women were enrolled, 30 in each study group. Adolescents with repeat pregnancy have lower self-esteem scores and more ineffective contraceptive use. When compared with teens at first delivery, they had less schooling level (odds ratio [OR] 4.03 [1.37-11.8]), more school abandon (OR 8.16 [2.36-28.2]) and drugs use (OR 4.97[1.39-17.8]). Non-white skin color (OR 6.2 [1.15-41.0]), drugs use (OR 17.5 [2.62-116.6]) and first sexual intercourse under 15y (OR 18.0[2.82-115.0]) were found as higher risk factors for repeat pregnancy when comparing adolescents and adults.Moreover, adolescents withmore than one gestation had lower self-esteem and greater susceptibility to unplanned pregnancy.
There was an association between repeat pregnancy among adolescents and lower education, early onset of sexual activity, non-white skin color, low use of contraception and increased use of drugs.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):410-416
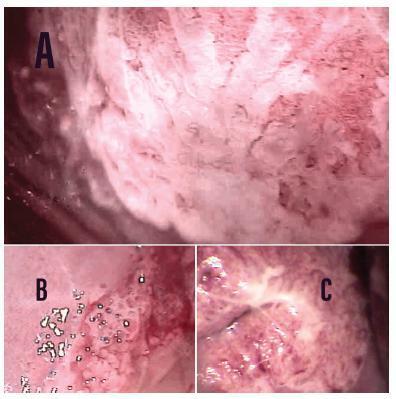
To estimate the cytological and colposcopic performances for the diagnosis of cervical neoplasias.
Cross-sectional retrospective study with data from patients’ charts. The participants underwent colposcopy, guided biopsies, and excision when needed. The cytological and colposcopic categorization followed the Bethesda System and the international colposcopic terminologies. The cytology and colposcopy performances were evaluated by sensitivity (SE), specificity (SP), positive predictive value (PPV), and negative predictive value (NPV) analyses with 95% confidence interval (95% CI).
From 1,571 participants, a total of 1,154 (73.4%) were diagnosed with cervical squamous intraepithelial neoplasia grade 2 or worse (CIN 2+), 114 (7.2%) with adenocarcinoma in situ or worse (AIS+), 615 (39.2%) presented atypical squamous cells, cannot exclude high-grade squamous intraepithelial lesion or worse (ASC-H+) cytology, and 934 (59.4%) presented major or suspicious for invasion colposcopic abnormalities. The SE, SP, PPV, and NPV of ASC-H+ for diagnoses of CIN 2+ and AIS+ were, respectively: 44% (95% CI: 41-47) and 72% (95% CI: 67-76), 79% (95% CI: 77-81) and 79% (95% CI: 75-83), 88% (95% CI: 87-90) and 55% (95% CI: 50-60), and 28% (95% CI: 26-31) and 88% (95% CI: 85-91). The SE, SP, PPV, and NPV of major or suspicious for invasion colposcopic abnormalities for diagnoses of CIN 2+ and AIS+were, respectively: 62% (95% CI: 60-65) and 86% (95% CI: 83-89), 59% (95% CI: 57-62) and 59% (95% CI: 55-64), 85% (95% CI: 83-87) and 44% (95% CI: 40-49), and 29% (95% CI: 27-32) and 92% (95% CI: 89-94).
The SE analyses results of ASC-H+ and major or suspicious for invasion colposcopic abnormalities were higher for diagnoses of glandular neoplasias. These results confirm the role of cytology in identifying women at risk who will have their final diagnoses settled by colposcopy and histology.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):397-402
To analyze the perioperative results and safety of performing gynecological surgeries using robot-assisted laparoscopy during implementation of the technique in a community hospital over a 6-year period.
This was a retrospective observational study in which the medical records of 274 patients who underwent robotic surgery from September 2008 to December 2014 were analyzed. We evaluated age, body mass index (BMI), diagnosis, procedures performed, American Society of Anesthesiologists (ASA) classification, the presence of a proctor (experienced surgeon with at least 20 robotic cases), operative time, transfusion rate, perioperative complications, conversion rate, length of stay, referral to the intensive care unit (ICU), and mortality. We compared transfusion rate, perioperative complications and conversion rate between procedures performed by experienced and beginner robotic surgeons assisted by an experienced proctor.
During the observed period, 3 experienced robotic surgeons performed 187 surgeries,while 87 surgeries were performedby 20 less experienced teams, always with the assistance of a proctor. The median patient age was 38 years, and the median BMI was 23.3 kg/m2. The most frequent diagnosis was endometriosis (57%) and the great majority of the patients were classified as ASA I or ASA II (99.6%). The median operative time was 225 minutes, and the median length of stay was 2 days. We observed a 5.8% transfusion rate, 0.8% rate of perioperative complications, 1.1% conversion rate to laparoscopy or laparotomy, no patients referred to ICU, and no deaths. There were no differences in transfusion, complications and conversion rates between experienced robotic surgeons and beginner robotic surgeons assisted by an experienced proctor.
In our casuistic, robot-assisted laparoscopy demonstrated to be a safe technique for gynecological surgeries, and the presence of an experienced proctor was considered a highlight in the safety model adopted for the introduction of the robotic gynecological surgery in a high-volume hospital and, mainly, for its extension among several surgical teams, assuring patient safety.