Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):475-482
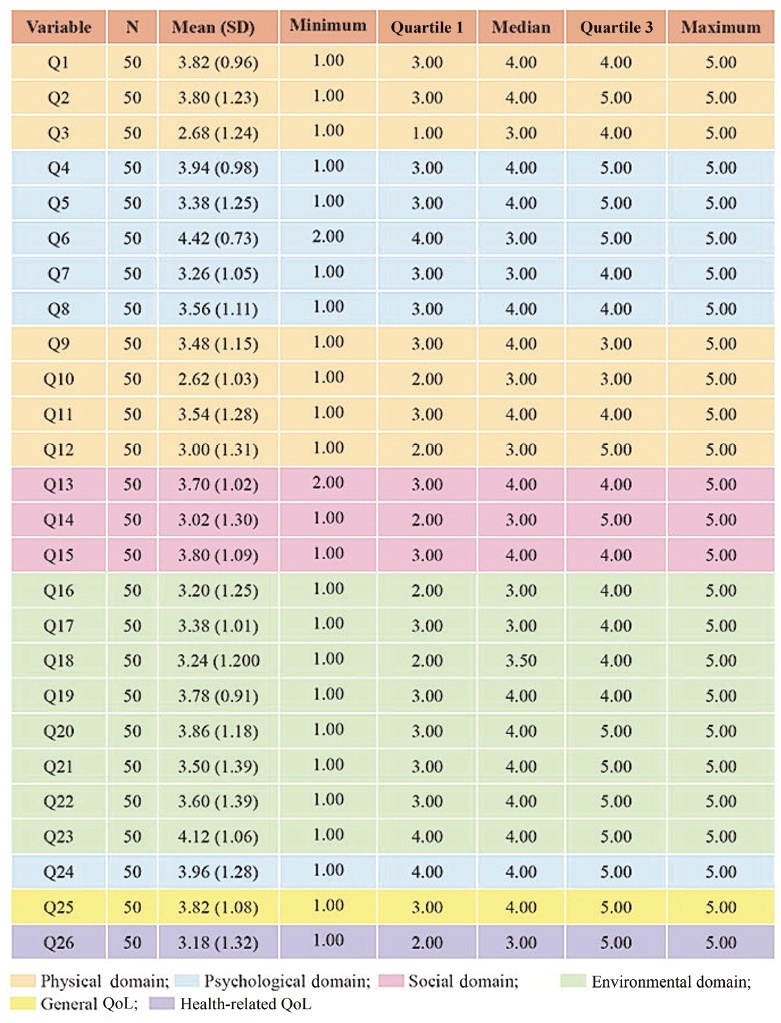
To assess the quality of life (QoL) of pregnant women with systemic lupus erythematosus (SLE) treated at a high-risk prenatal outpatient clinic during the third trimester of gestation.
An observational descriptive study was performed in a high-risk prenatal outpatient clinic. Women in the third trimester of pregnancy and undergoing antenatal care between July 2017 and July 2019 answered the abbreviated World Health Organization Quality of Life (WHOQOL-BREF) questionnaire, consisting of 26 questions divided into 4 domains (physical, psychological, social and environmental).
We interviewed 50 pregnant women with a mean gestational age of 30 weeks (standard deviation [SD]: 10 weeks) who were diagnosed with SLE. The average age of the participants was 30 years (SD: 14.85), and the average time since the diagnosis of SLE was of 9.06 years (SD: 6.8 years). Most participants had a partner, did not plan their pregnancy (76%), and did not use contraception prior to pregnancy (80%). The score of each domain ranges from 0 (the worst score) to 100 (the best score). The means ± SDs of the scores of the participants on each domain were: physical - 52.21 ± 18.44); psychological - 64.17 ± 18.56); social - 66.33 ± 27.09); and environmental - 64.56 (18.53). The means ± SDs of the general QoL, and health-related QoL items were of 70.50 ± 24.06 and 70.00 ± 30.72 respectively.
The physical domain presented the lowest scores compared with the other three domains. Pregnant women with SLE had high overall QoL scores, and their health-related QoL scores were also relatively high.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):398-408
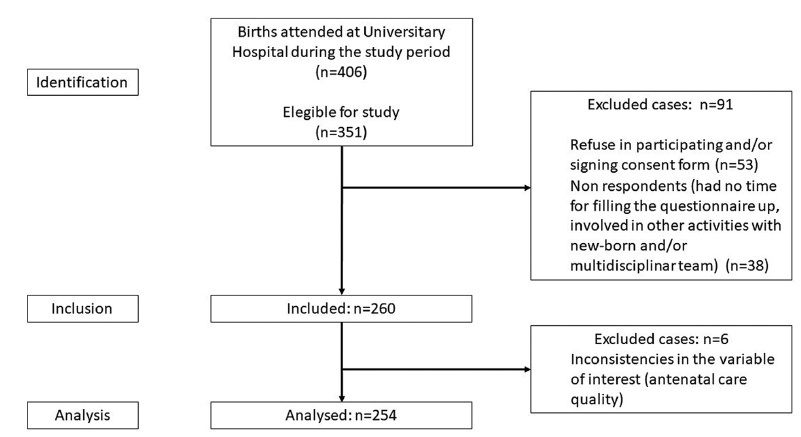
The present study aimed to evaluate the antenatal care adequacy for women who gave birth at the University Hospital of Santa Catarina in Florianopolis (Brazil) during the COVID-19 pandemic, and to evaluate the association of adequacy with sociodemographic, clinical, and access characteristics.
Data were collected between October and December 2020, including 254 patients who delivered in the University Hospital from Federal University of Santa Catarina and answered our questionnaires. Additional data were obtained from patients’ antenatal booklets. Antenatal care was classified as adequate, intermediate, or inadequate according to the number of appointments, gestational age at the beginning of follow-up, and tests results. We carried out a descriptive statistical analysis and a bivariate/with odds ratio analysis onmaternal sociodemographic, clinical and health access variables that were compared with antenatal adequacy.
Antenatal care was considered adequate in 35.8% of cases, intermediate in 46.8%, and inadequate in 17.4%. The followingmaternal variables were associated with inadequate prenatal care (intermediate or inadequate prenatal care): having black or brown skin colour, having two or more children, being of foreign nationality, not being fluent in Portuguese, and using illicit drugs during pregnancy; the clinical variables were more than 6 weeks between appointments, and not attending high-risk antenatal care; as for access, the variables were difficulties in attending or scheduling appointments, and attending virtual appointments only.
In a sample of pregnant women from a teaching hospital in Florianópolis during the COVID-19 pandemic, antenatal care was considered adequate in 35.8%, intermediate in 46.8%, and inadequate in 17.4% of cases.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):352-359
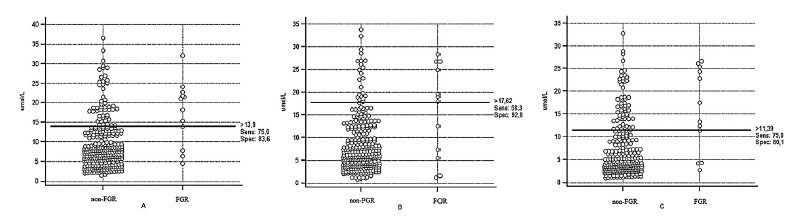
To assess homocysteine (Hcy) levels in the three trimesters of pregnancy in women with fetal growth restriction (FGR) and to evaluate the role of Hcy as a possible predictor of FGR.
A total of 315 singleton pregnant women were included in the present prospective cohort study and were monitored since the 1st trimester of pregnancy before delivery. Newborns were monitored for the first 7 days of life. Patients who had risk factors for FGR were excluded. Fetal growth restriction was defined according to uterine fundal height (< 10 percentile), ultrasound fetometry (< 5 percentile), and anthropometry of newborns (<5 percentile). The concentrations of Hcy were detected at between 10 and 14, between 20 and 24, and between 30 and 34 weeks of pregnancy by enzyme-linked immunosorbent assay (ELISA). Receiver operating characteristics (ROC) curve test and diagnostic odds ratio (DOR) were performed to evaluate the results of ELISA.
The concentration of Hcy in patients with FGR was 19.65 umol/L at between 10 and 14 weeks, compared with 9.28 umol/L in patients with normal fetal growth (p<0.0001). The optimal cut-off level for Hcy in the 1st trimester of pregnancy was>13.9 umol/L with AUC 0.788, sensitivity of 75%, specificity of 83.6%, and DOR of 15.2.
Assessment of serum Hcy concentration may be used as a predictor of FGR, with the highest diagnostic utility in the 1st trimester of pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):264-271
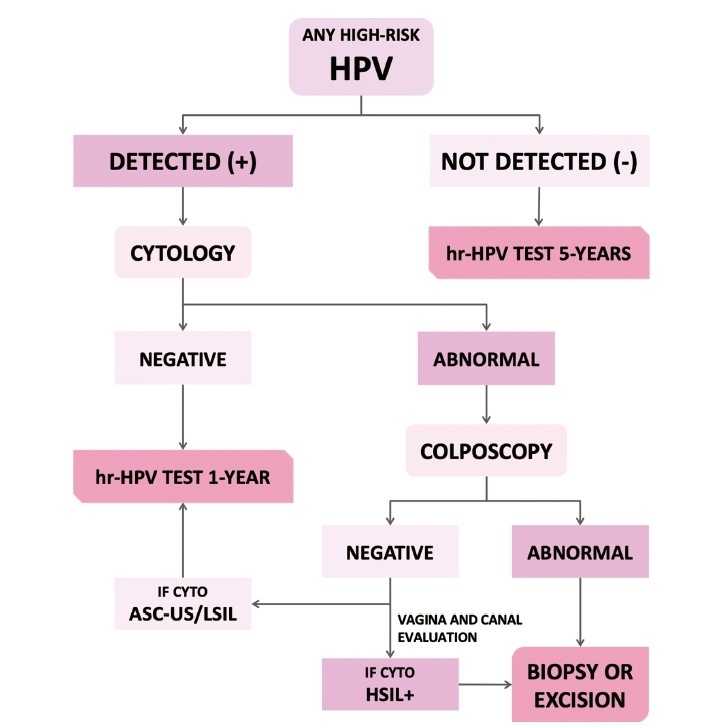
The present update is a reassessment of the 2018 ‘Guidelines for HPV-DNA Testing for Cervical Cancer Screening in Brazil’ (Zeferino et al.)9, according to the changes observed in new international guidelines and knowledge updates. The most relevant and recent guidelines were assessed. Questions regarding the clinical practice were formulated, and the answers considered the perspective of the public and private sectors of the Brazilian health system. The review addressed risk-based strategies regarding age to start and stop screening, the use of cytology and colposcopy to support management decisions, treatment, follow-up strategies, and screening in specific groups, including vaccinated women. The update aims to improve the prevention of cervical cancer and to reduce overtreatment and the misuse of HPV testing.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):483-488
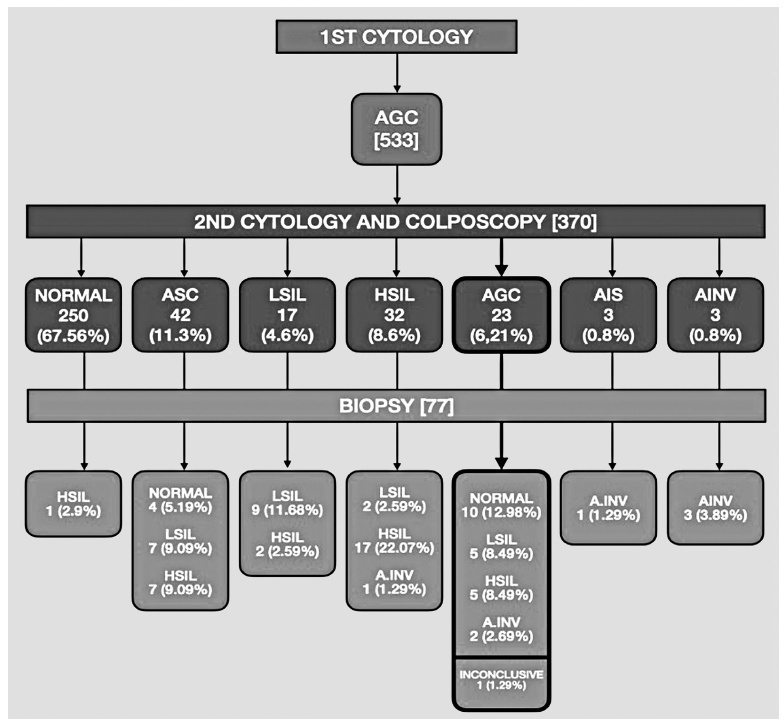
To determine the prevalence of the atypical glandular cells (AGCs) cytology and to analyze its clinical significance in different age ranges.
Retrospective observational study using computerized data from the Brazilian National Cancer Institute, including women screened between January 2002 and December 2008. The women included were those with an AGC result who were properly followed-up with colposcopy and a second cytology.
A total of 132,147 cytopathological exams were performed during the study period. Five-hundred and thirty-three (0.4%) women with AGC cytology were identified and, of these, 69.41% (370/533) were properly referred for colposcopy and a new cytology. Most of the women (79.2%) with a 1st or 2nd AGC cytology were between the ages of 25 and 54 years. The 2nd cytology demonstrated 67.6% (250/370) of normality, 24.5% (91/370) of squamous atypia, and 6.2% (23/370) of AGC, 0.8% (3/370) adenocarcinoma in situ and 0.8% (3/370) adenocarcinoma invasor. On biopsy of the women with a second AGC cytology, 43.4% (10/23) had normal histology, 43.4% (10/23) had squamous lesions, 8.7% (2/23) had invasive adenocarcinoma, and 1.2% (1/23) had an inconclusive report. All of the women with high-grade squamous intraepithelial lesion (HSIL) or invasive adenocarcinoma (respectively 5 and 2 patients), after a 2nd AGC cytology were 25 years old or older.
The prevalence of the AGC cytology was low in the studied population. Most of the AGC cytology cases occurred in adult women between the ages of 25 and 54. Although most of the patients had normal histology after follow-up, several of them presented with squamous intraepithelial lesions or invasive adenocarcinoma.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):280-286
The purpose of this study was to compare the frequency of the occurrence of high-risk human papillomavirus (HPV) and abnormal anal cytology in immunocompetent women with and without HPV-induced genital lesions.
This analytical cross-sectional, observational study was conducted between July 2017 and December 2018 in a specialized outpatient clinic of a tertiary hospital in Fortaleza, CE. Fifty-seven immunocompetent women with and without genital intraepithelial lesions were assessed; they were divided into two groups: group 1 was comprised of women with HPV-associated genital lesions (n=26), and group 2 was comprised of those without HPV-associated genital lesions (n=31). Samples for liquidbased cytology and high-risk DNA-HPV polymerase chain reaction real-time tests were collected from the cervix and anus. All cases were evaluated using high-resolution anoscopy; biopsies were performed when required. The Fisher exact and chi-squared tests were applied for consolidated data in the contingency table, and the Student ttest and Mann-Whitney U-test for independent variables.
Anal high-risk HPV infections were more frequent in group 1 (odds ratio [OR], 4.95; 95% confidence interval [CI], 1.34-18.3; p=0.012), along with concomitant highrisk HPV infections in the uterine cervix and the anus (OR 18.8; 95% CI, 2.20-160; p<0.001). The incidence of high-risk cervical HPV infection was associated with highrisk anal HPV infection (OR, 4.95; 95% CI, 1.34-18.3; p=0.012). There was no statistical difference concerning abnormal anal cytology or anoscopy between the groups, and no anal intraepithelial lesion was found in either group.
Immunocompetent women with HPV-associated genital lesions and high-risk cervical HPV were more likely to have high-risk anal HPV.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):258-263
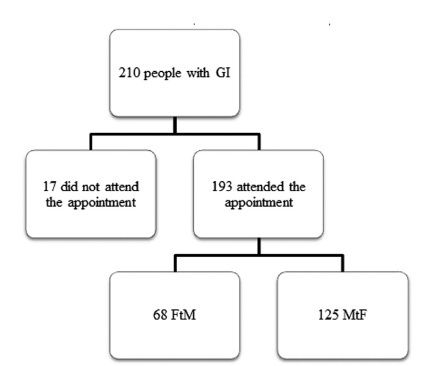
To identify the age when individuals first perceive gender incongruence (GI) and to compare sociodemographic data of female-to-male (FtM) and male-tofemale (MtF) transgender individuals assisted at an outpatient service.
The present cross-sectional study was conducted through a review of the medical records of individuals diagnosed with GI at a single specialized outpatient service in the city of Ribeirão Preto, state of São Paulo, Brazil.
A total of 193 medical records from 2010 to 2018 were evaluated, and 109 (56.5%) patients had GI since childhood. The FtM transgender individuals perceived GI in childhood more often than the MtF transgender individuals (odds ratio [OR]: 2.06, 95% confidence interval [95%CI]: 1.11-3.81) Unattended hormone use was highest among the MtF group (69.6% versus 32.3%; OR: 4.78, 95%CI: 2.53-9.03). All of the individuals who were engaged in prostitution or were diagnosed with a sexuallytransmitted infection, including HIV, were in the MtF group.
Despite the more prevalent perception of GI in childhood among the FtM group, social issues were more prevalent among the MtF group, which may be the result of social marginalization.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):251-257
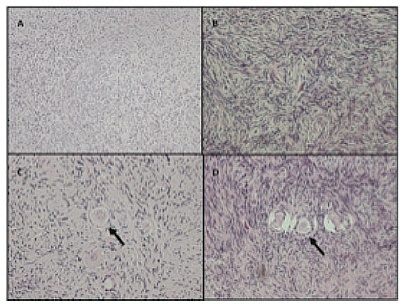
To evaluate the reproductive and histological characteristics of fresh cultured ovarian tissue from transgender male patients.
An in vitro pilot study in which samples were collected during sex reassignment surgery for transgender male patients. The ovarian cortex was cut into fragments of 2 mm, 3mm, and 4 mm, and placed in a 96-well plate suitable for cultivation at days 0, 2, 4, 6, and 8, when the histology was analyzed.
Stromal hyperplasia was observed in all samples, and it was not associated with the obtainment of primordial or primary follicles. Peripheral reduction in cell count was also a recurrent finding. Primordial and primary follicles were identified with a heterogeneous pattern in fragments from the same patient and from different patients, and follicles in more advanced stages of development (secondary and antral) were not found. There was an association between the diameter of the ovarian fragments and the identification of primary follicles (p=0.036). The number of days in culture was associated with histological signs of tissue damaging in the fragments (p=0.002). The total number of follicles identified in the samples with 2mm in diameter was significantly lower than in those that measured 4mm in diameter (p=0.031).
A diameter of 4mm is suitable for ovarian tissue culture with the benefit of ease of handling. Even after prolonged exposure to testosterone, the ovarian fragments presented primordial and primary follicles, maintaining viability throughout the days they were exposed to the culture. Freezing the ovarian cortex of transgender patients who will undergo surgery for gender reassignment would be an interesting option, in the future, for the preservation of fertility.