Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(11):847-852
To compare the prevalence of urinary incontinence (UI) before and during the COVID-19 quarantine in CrossFit women and their relationship with training level.
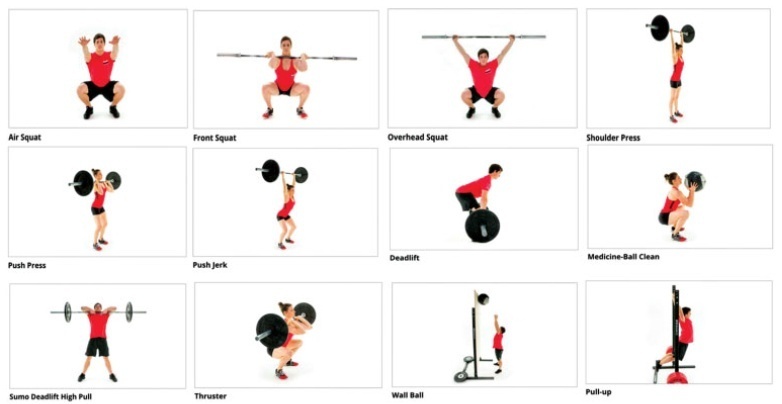
A cross-sectional study was performed among 197 women practicing CrossFit. The inclusion criteria were nulliparous women, between 18 and 45 years old, who had trained, before quarantine, in accredited gyms. The exclusion criteria were not following the COVID-19 prevention protocols and having UI on other occasions than just sport. An online questionnaire was emailed containing questions about frequency, duration, and intensity of training and data related to the COVID-19 pandemic. The participants were invited to answer whether they were infected with COVID-19 and what treatment/recommendation they have followed. Whether UI stopped among participants, they were asked about the possible reasons why this happened. The training intensity was categorized as “the same,” “decreased” or “increased.”
The mean age of the participants was 32 years old and most (98.5%) could practice CrossFit during the pandemic. There was a decrease in training intensity in 64% of the respondents. Exercises with their own body weight, such as air squat (98.2%), were the most performed. Urinary incontinence was reported by 32% of the participants before the COVID-19 pandemic, and by only 14% of them during the pandemic (odds ratio [OR]=0.32 [0.19-0.53]; p<0.01; univariate analysis). Practitioners reported that the reason possibly related to UI improvement was the reduction of training intensity and not performing doubleunder exercise.
The reduction in the intensity of CrossFit training during the COVID-19 quarantine decreased the prevalence of UI among female athletes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(11):840-846
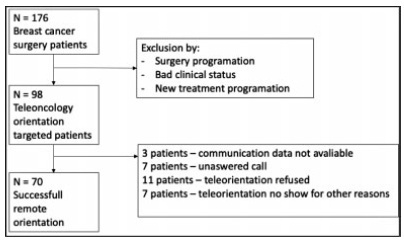
The present study aims to assess the feasibility and patient satisfaction of teleoncology orientation in a vulnerable population of breast cancer patients assessed in a government health system during the coronavirus pandemic in 2020.
Eligible patients received an invitation to receive remote care to minimize exposure to an environment in which the risk of respiratory infection was present. The means of communication was telephone through an application that allows free conversation with no charge. An anonymous-response questionnaire based on a Likert-type scale was sent through a cell phone application or e-mail directly to each patient or close relative of the patient immediately after teleconsultation. Responses to the questions, which addressed utility, facility, interface quality, interaction quality, reliability, satisfaction, and interest in future evaluation, were compiled and analyzed.
A total of 176 eligible patients scheduled for consultation were evaluated and 98 were included. Seventy (71.4%) successfully undertook the teleorientation. The questionnaire was submitted by 43 (61.4%) patients. The overall teleoncology orientation was classified as very positive by 41 (95.3%) patients. Specifically, regarding the questionnaire items, 43 (100%) patients scored 4 or 5 (agreed that the teleconsultation was beneficial) concerning the facility, followed by 42 (97.2%) for the interface quality, 41 (95.3%) for both utility and interaction quality, 40 (93%) for satisfaction and interest in future evaluation, and, finally, 39 (90.6%) for reliability.
Teleoncology orientation of low-income breast cancer patients is most feasible and leads to high patient satisfaction.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(11):834-839
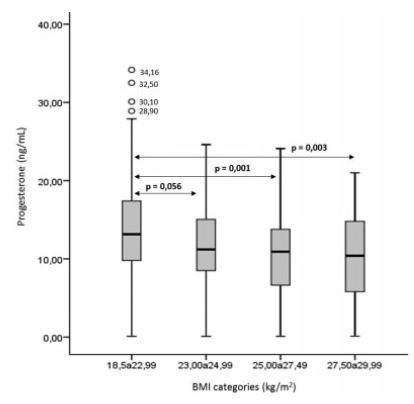
It has been suggested that excess body weight could represent a risk factor for infertility outcomes. The present study aimed to evaluate the association of overweight and anovulation among infertile women with regular menstrual cycles.
We conducted a retrospective case-control study with consistently anovulatory patients undergoing assisted reproduction treatment. The patients were stratified into normal weight (body mass index [BMI]: 18.5-24.9kg/m2) and overweight (BMI: 25.0- 29.9kg/m2).Those with polycystic ovary syndrome or obesity were excluded. The groups were matched for age, duration of infertility, prolactin, follicle stimulating hormone (FSH), thydroid stimulating hormone (TSH), luteinizing hormone (LH), and estradiol levels.
Overweight was significantly associated with anovulation, when using the World Health Organization (WHO) criteria for anovulation: progesterone levels>5.65 ng/ml and ultrasonography evidence of follicle collapse (odds ratio [OR]: 2.69; 95% confidence interval [CI95%]: 1.04-6.98).
Body mass index above the normal range jeopardizes ovulation among non-obese infertile women with regular menstrual cycles.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(11):820-825
To compare maternal and perinatal risk factors associated with complete uterine rupture and uterine dehiscence.
Cross-sectional study of patients with uterine rupture/dehiscence from January 1998 to December 2017 (30 years) admitted at the Labor and Delivery Unit of a tertiary teaching hospital in Canada.
There were 174 (0.1%) cases of uterine disruption (29 ruptures and 145 cases of dehiscence) out of 169,356 deliveries. There were associations between dehiscence and multiparity (odds ratio [OR]: 3.2; p=0.02), elevated maternal body mass index (BMI; OR: 3.4; p=0.02), attempt of vaginal birth after a cesarian section (OR: 2.9; p=0.05) and 5-minute low Apgar score (OR: 5.9; p<0.001). Uterine rupture was associated with preterm deliveries (36.5 ± 4.9 versus 38.2 ± 2.9; p=0.006), postpartum hemorrhage (OR: 13.9; p<0.001), hysterectomy (OR: 23.0; p=0.002), and stillbirth (OR: 8.2; p<0.001). There were no associations between uterine rupture and maternal age, gestational age, onset of labor, spontaneous or artificial rupture of membranes, use of oxytocin, type of uterine incision, and birthweight.
This large cohort demonstrated that there are different risk factors associated with either uterine rupture or dehiscence. Uterine rupture still represents a great threat to fetal-maternal health and, differently from the common belief, uterine dehiscence can also compromise perinatal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(11):811-819
To investigate the characteristics of women who had preterm birth (PTB) and related outcomes according to ethnicity.
A secondary analysis of a multicenter cross-sectional study conducted in Brazil. Women who had PTB were classified by self-report as white and non-white. Clinical, pregnancy, and maternal data were collected through postpartum interviews and reviews of medical charts. The sociodemographic, obstetric and clinical characteristics of the women, as well as the mode of delivery and the neonatal outcomes among different ethnic groups were compared through a bivariate analysis.
Of the 4,150 women who had PTB, 2,317 (55.8%) were non-white, who were more likely: to be younger than 19 years of age (prevalence ratio [PR]: 1.05; 95% confidence interval [95%CI]: 1.01-1.09); to be without a partner; to live on low income; to have lower levels of schooling; to have ≥ 2 children; to perform strenuous work; to be fromthe Northeastern region of Brazil rather than the from Southern region; to have a history of ≥ 3 deliveries; to have an interpregnancy interval<12 months; to have pregnancy complications such as abortion, PTB, preterm premature rupture of membranes (pPROM), and low birth weight; to initiate antenatal care (ANC) visits in the second or third trimesters; to have have an inadequate number of ANC visits; to be under continuous overexertion; to smoke in the first and second or third trimesters; and to have anemia and gestational hypertension. The maternal and neonatal outcomes did not differ between the groups, except for the higher rate of low birth weight (73.7% versus 69.0%) in infants born to non-white women, and the higher rate of seizures (4.05% versus 6.29%) in infants born to white women.
Unfavorable conditions weremore common in non-whites than inwhites. Proper policies are required to decrease inequalities, especially in the context of prematurity, when women and their neonates have specific needs.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(11):805-810
The aim of the present study was to examine the relation between the PON1 polymorphisms and recurrent pregnancy loss (RPL).
In a cross-sectional study, blood samples were collected from 100 females. DNA was extracted and PON1 genotypes were determined by polymerase chain reaction (PCR) amplification.
Regarding PON1 L55M, the mutated allele (M) frequency was found in 70.5% in RPL and in 53.5% in controls; theMallele was significantly associated with an increased risk of RPL (adjusted odds ratio [ORadj]=2.07; 95% confidence interval [CI]; p<0.001). However, regarding PON1 Q192R, the R mutated allele frequency was found in 28.5% in RPL and in 33% in controls. The R allele did not show any risk for RPL (ORadj 0.81; 95%CI; p=0.329).
The present study suggests that there is an effect of genetic polymorphism on RPL and provides additional evidence that combines with the growing information about the ways in which certain PON1 genotypes can affect the development of the fetus in the uterus.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(10):765-774
To investigate depression and sexual function among pregnant and nonpregnant women throughout the COVID-19 pandemic.
A total of 188 women, 96 pregnant and 92 non-pregnant were included. The Beck Depression Inventory (BDI) and the Arizona Sexual Experience Scale (ASEX) were applied to the participants after obtaining sociodemographic data.
The depression scores of pregnant and non-pregnant women were similar (p = 0.846). We found that the depression scores were significantly higher among the group of participants who have lower economic status (p = 0.046). Moreover, the depression score was significantly higher among women who lost their income during the pandemic (p = 0.027). The score on the ASEX was significantly higher, and sexual dysfunction was more prevalent among women who have lower levels of schooling and income (p < 0.05). Likewise, the ASEX scores were significantly higher (p = 0.019) among the group who experienced greater income loss throughout the pandemic. Upon comparing the pregnant and non-pregnant groups, we detected that sexual dysfunction had a significantly higher rate among pregnant women (p < 0.001).
In times of global crisis, such as the current pandemic, low-income families have an increased risk of experiencing depression and sexual dysfunction. When we compared pregnant women with non-pregnant women, depression scores were similar, but pregnant women were at a 6.2 times higher risk of developing sexual dysfunction.