Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(4):192-200
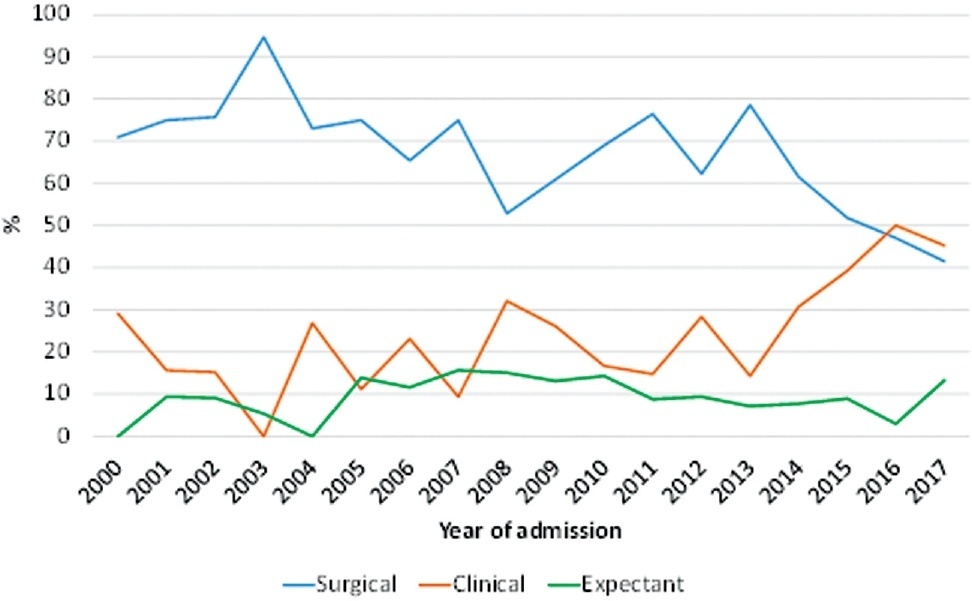
To evaluate the use of different treatment options for ectopic pregnancy and the frequency of severe complications in a university hospital.
Observational study with women with ectopic pregnancy admitted at UNICAMP Womeńs Hospital, Brazil, between 01/01/2000 and 12/31/2017. The outcome variables were the type of treatment (first choice) and the presence of severe complications. Independent variables were clinical and sociodemographic data. Statistical analysis was carried out by the Cochran–Armitage test, chi-square test, Mann–Whitney test and multiple Cox regression.
In total 673 women were included in the study. The mean age was 29.0 years (± 6.1) and the mean gestational age was 7.7 (± 2.5). The frequency of surgical treatment decreased significantly over time (z = -4.69; p < 0.001). Conversely, there was a significant increase in the frequency of methotrexate treatment (z = 4.73; p < 0.001). Seventy-one women (10.5%) developed some type of severe complication. In the final statistical model, the prevalence of severe complications was higher in women who were diagnosed with a ruptured ectopic pregnancy at admission (PR = 2.97; 95%CI: 1.61–5.46), did not present with vaginal bleeding (PR = 2.45; 95%CI: 1.41–4.25), had never undergone laparotomy/laparoscopy (PR = 6.69; 95%CI: 1.62–27.53), had a non-tubal ectopic pregnancy (PR = 4.61; 95%CI: 1.98–10.74), and do not smoke (PR = 2.41; 95%CI: 1.08–5.36).
there was a change in the first treatment option for cases of ectopic pregnancy in the hospital during the period of analysis. Factors inherent to a disease that is more difficult to treat are related to a higher frequency of severe complications.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(4):186-191
Psychiatric symptoms are common mental issues in pregnancy and the postpartum period. There is limited information regarding the psychiatric symptoms of women with high-risk pregnancy in the postpartum period. This study aimed to compare the severity of psychiatric symptoms and psychological distress in women with high-risk and low-risk pregnancies in the postpartum period.
This case-control study examined 250 women in the postpartum period in two groups with low-risk (n = 112) and high-risk (n = 138) pregnancies. Women completed the Brief Symptom Inventory-53 (BSI-53) and the Risk Postnatal Psychosocial Depression Risk Questionnaire (PPDRQ).
The mean severity of psychiatric symptoms in women with high-risk pregnancies was significantly higher than that in women with low-risk pregnancies (39.34 ± 17.51 vs. 30.26 ± 17.08). Additionally, the frequency of psychological distress in women with high-risk pregnancies was approximately twice higher than that in women with low-risk pregnancies (30.3% vs. 15.2%). Furthermore, the risk factors for depression in women with high-risk pregnancies were almost 1.5 times (59.8% vs. 39.8%) higher than the factors in women with low-risk pregnancies. The results of the logistic analysis indicated that high-risk pregnancies could be twice the odds ratio of developing postpartum psychological distress (ß = 2.14, 95% CI 1.4-6.3, p= 0.036).
Psychiatric symptoms and the psychological distress index are higher in postpartum women with high-risk pregnancies than in postpartum women with low-risk pregnancies. The study suggests that obstetricians and pregnant women's health care providers should strongly consider screening of psychiatric symptoms in women with high-risk pregnancies both during pregnancy and after delivery as the women's routine care priorities.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(4):179-185
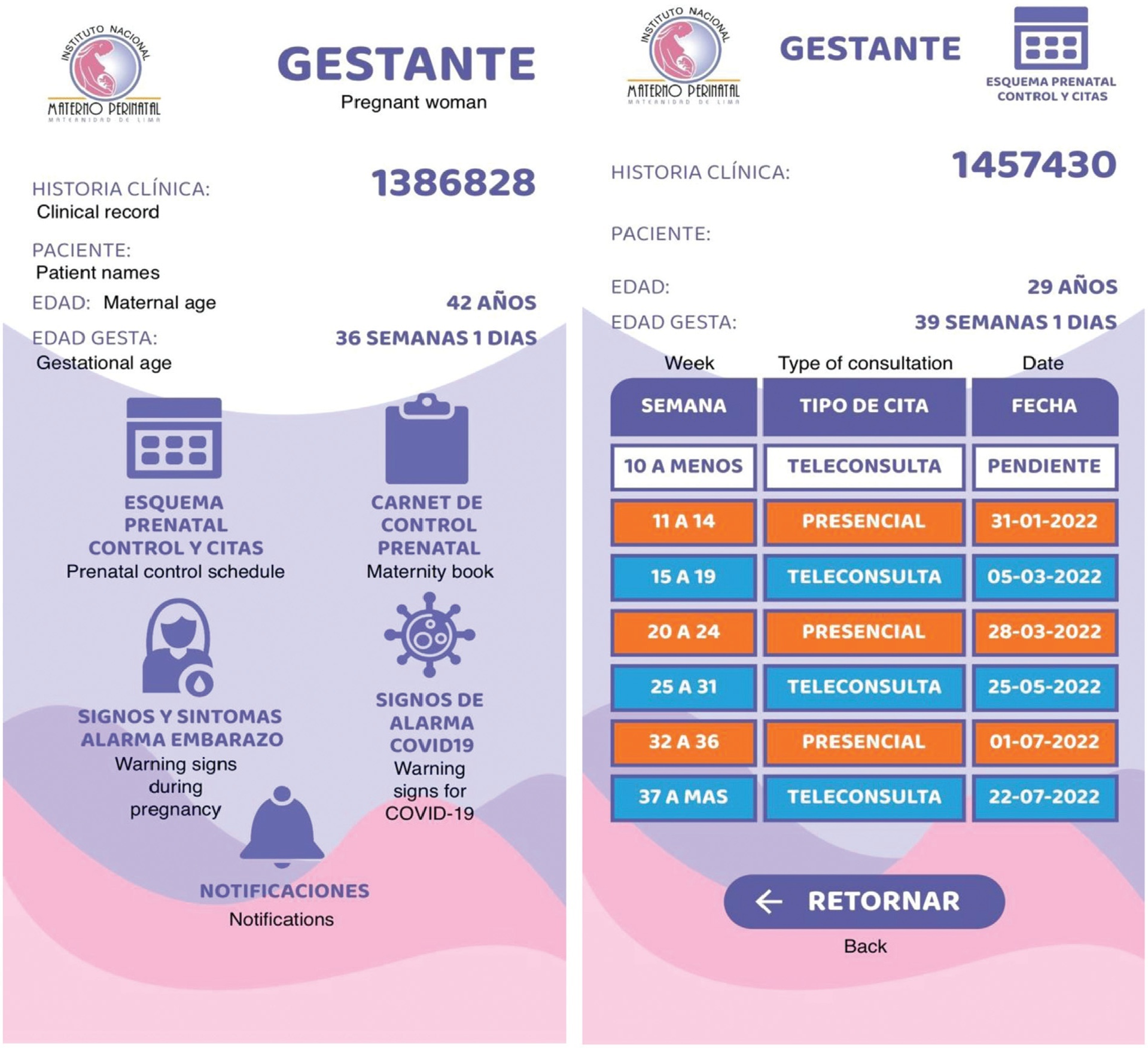
We describe the development and structure of a novel mobile application in a mixed model of prenatal care, in the context of the COVID-19 pandemic. Furthermore, we assess the acceptability of this mobile app in a cohort of patients.
First, we introduced a mixed model of prenatal care; second, we developed a comprehensive, computer-based clinical record to support our system. Lastly, we built a novel mobile app as a tool for prenatal care. We used Flutter Software version 2.2 to build the app for Android and iOS smartphones. A cross-sectional study was carried out to assess the acceptability of the app.
A mobile app was also built with the main attribute of being connected in real-time with the computer-based clinical records. The app screens detail information about activities programmed and developed in the prenatal care according to gestational age. A downloadable maternity book is available and some screens show warning signs and symptoms of pregnancy. The acceptability assessment was mostly rated positively regarding the characteristics of the mobile app, by 50 patients.
This novel mobile app was developed as a tool among pregnant patients to increase the information available about their pregnancies in the provision of a mixed model of prenatal care in the context of the COVID-19 pandemic. It was fully customized to the needs of our users following the local protocols. The introduction of this novel mobile app was highly accepted by the patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(4):171-178
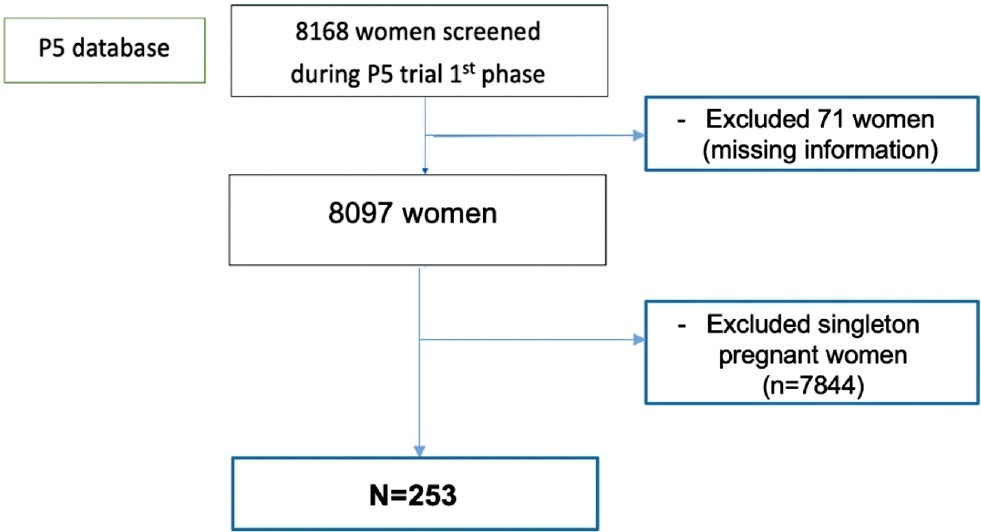
To describe a reference curve for cervical length (CL) in mid-trimester twin gestations using transvaginal ultrasound (TVU) and to investigate whether short CL increases spontaneous preterm birth (sPTB) in asymptomatic twin pregnancies.
This was a prospective cohort study performed at 17 outpatient antenatal facilities of Brazil with women at 18 0/7 to 22 6/7 weeks of gestation who participated in a randomized clinical trial screening phase (P5 trial) between July 2015 and March 2019. TVU was performed to provide CL measurement in all screened women. Almost all women with CL ≤ 30 mm received vaginal progesterone 200mg/day and they were also randomized to receive cervical pessary or not. We considered data from the CL distribution among asymptomatic twin pregnancies and analyzed CL and its association with PTB generating receiver operating characteristics (ROC) curves and Kaplan-Meier curves.
A total of 253 pregnant women with twins were included in the distribution curve. The mean CL was 33.7 mm and median was 35.5mm. The 10th percentile was 17.8mm. We identified a PTB rate of 73.9% (187/253) with 33.6% of sPTB < 37 (85/253) and 15% (38/253) of sPTB < 34 weeks. The best cutoff point to predict sPTB < 37 was 24.15 mm. However, the ROC curve showed a poor performance (0.64). The Kaplan-Meier survival curves identified that only CL values ≤ 20mm were associated to sPTB < 34 weeks.
A cutoff point of CL ≤ 20 mm can be interesting point to identify short cervix in Brazilian twin pregnancies. However, in Brazilian asymptomatic twin pregnancies, CL does not show a good performance to predict PTB.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):11-20
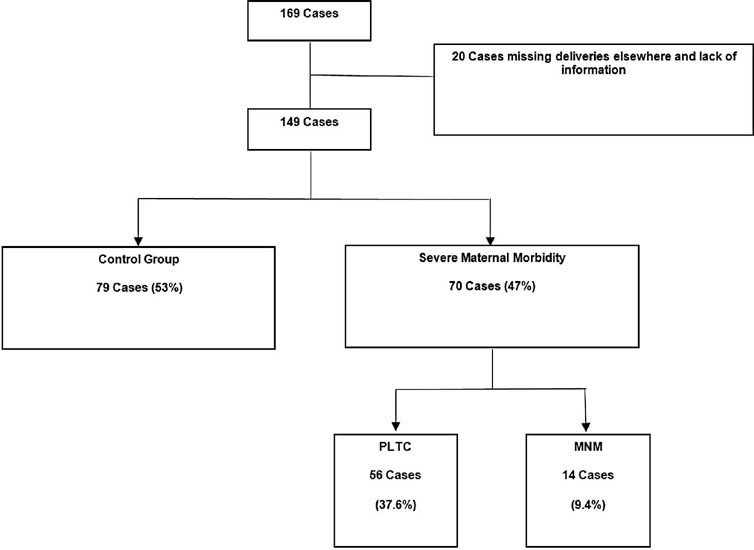
Systemic lupus erythematosus (SLE) may cause irreversible organ damage. Pregnancy with SLE may have severe life-threatening risks. The present study aimed to determine the prevalence of severe maternal morbidity (SMM) in patients with SLE and analyze the parameters that contributed to cases of greater severity.
This is a cross-sectional retrospective study from analysis of data retrieved from medical records of pregnant women with SLE treated at a University Hospital in Brazil. The pregnant women were divided in a control group without complications, a group with potentially life-threatening conditions (PLTC), and a group with maternal near miss (MNM).
The maternal near miss rate was 112.9 per 1,000 live births. The majority of PLTC (83.9%) and MNM (92.9%) cases had preterm deliveries with statistically significant increased risk compared with the control group (p = 0.0042; odds ratio [OR]: 12.05; 95% confidence interval [CI]: 1.5–96.6 for the MNM group and p = 0.0001; OR: 4.84; 95%CI: 2.2–10.8 for the PLTC group). Severe maternal morbidity increases the risk of longer hospitalization (p < 0.0001; OR: 18.8; 95%CI: 7.0–50.6 and p < 0.0001; OR: 158.17; 95%CI: 17.6–1424,2 for the PLTC and MNM groups, respectively), newborns with low birthweight (p = 0.0006; OR: 3.67; 95%CI: 1.7–7.9 and p = 0.0009; OR: 17.68; 95%CI: 2–153.6) for the PLTC and MNM groups, respectively] as well as renal diseases (PLTC [8.9%; 33/56; p = 0.0069] and MNM [78.6%; 11/14; p = 0.0026]). Maternal near miss cases presented increased risk for neonatal death (p = 0.0128; OR: 38.4; 95%CI: 3.3–440.3]), and stillbirth and miscarriage (p = 0.0011; OR: 7.68; 95%CI: 2.2–26.3]).
Systemic lupus erythematosus was significantly associated with severe maternal morbidity, longer hospitalizations, and increased risk of poor obstetric and neonatal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):38-42
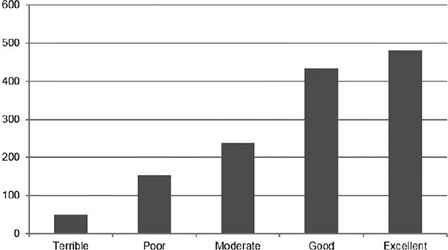
Pain is the primary limitation to performing hysteroscopy. We aimed to evaluate the predictive factors of low tolerance to office hysteroscopic procedures. Methods Retrospective cohort study of the patients who underwent office hysteroscopy from January 2018 to December 2020 at a tertiary care center. Pain tolerance to office-based hysteroscopy was subjectively assessed by the operator as terrible, poor, moderate, good, or excellent. Categorical variables were compared with the use of the Chi-squared test; an independent-samples t-test was conducted to compare continuous variables. Logistic regression was performed to determine the main factors associated with low procedure tolerance.
A total of 1,418 office hysteroscopies were performed. The mean age of the patients was 53 ± 13.8 years; 50.8% of women were menopausal, 17.8% were nulliparous, and 68.7% had a previous vaginal delivery. A total of 42.6% of women were submitted to an operative hysteroscopy. Tolerance was categorized as terrible or poor in 14.9% of hysteroscopies and moderate, good, or excellent in 85.1%. A terrible or poor tolerance was more frequently reported in menopausal women (18.1% vs. 11.7% in premenopausal women, p = 0.001) and women with no previous vaginal delivery (18.8% vs. 12.9% in women with at least one vaginal birth, p = 0.007). Low tolerance led more often to scheduling a second hysteroscopic procedure under anesthesia (56.4% vs. 17.5% in reasonable-to-excellent tolerance, p < 0.0005).
Office hysteroscopy was a well-tolerated procedure in our experience, but menopause and lack of previous vaginal delivery were associated with low tolerance. These patients are more likely to benefit from pain relief measures during office hysteroscopy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):31-37
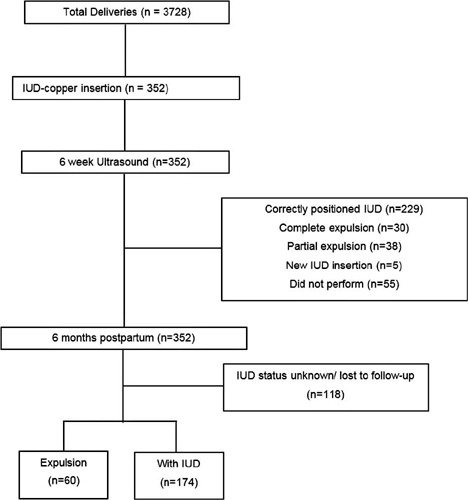
To evaluate the expulsion and continuation rates of the copper intrauterine device (IUD) inserted in the immediate postpartum period in a Brazilian public university hospital.
In the present cohort study, we included women who received immediate postpartum IUD at vaginal delivery or cesarean s March 2018 to December 2019. Clinical data and the findings of transvaginal ultrasound (US) scans performed 6-weeks postpartum were collected. The expulsion and continuation rates were assessed 6-months postpartum using data from the electronic medical records or by telephone contact. The primary outcome was the proportion of IUDs expelled at 6 months. For the statistical analysis, we used the Student t-test, the Poisson distribution, and the Chi-squared test.
There were 3,728 births in the period, and 352 IUD insertions were performed, totaling a rate of 9.4%. At 6 weeks postpartum, the IUD was properly positioned in 65.1% of the cases, in 10.8% there was partial expulsion, and in 8.5% it had been completely expelled. At 6 months postpartum, information was obtained from 234 women, 74.4% of whom used IUD, with an overall expulsion rate of 25.6%. The expulsion rate was higher after vaginal delivery when compared with cesarean section (68.4% versus 31.6% respectively; p = 0.031). There were no differences in terms of age, parity, gestational age, final body mass index, and newborn weight.
Despite the low insertion rate of copper IUDs in the postpartum period and a higher expulsion rate, the rate of long-term continuation of intrauterine contraception was high, indicating that it is a useful intervention to prevent unwanted pregnancies and to reduce short-interval birth.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):21-30
To evaluate the rates of precancerous lesions, colposcopy referral, and positive predictive value (PPV) by age groups of a population-based screening with DNA-HPV testing.
The present demonstration study compared 16,384 HPV tests performed in the first 30 months of the program with 19,992 women tested in the cytology screening. The colposcopy referral rate and PPV for CIN2+ and CIN3+ by age group and screening program were compared. The statistical analysis used the chi-squared test and odds ratio (OR) with 95% confidence interval (95%CI).
The HPV tests were 3.26% positive for HPV16-HPV18 and 9.92% positive for 12 other HPVs with a 3.7 times higher colposcopy referral rate than the cytology program, which had 1.68% abnormalities. Human Papillomavirus testing detected 103 CIN2, 89 CIN3, and one AIS, compared with 24 CIN2 and 54 CIN3 detected by cytology (p < 0.0001). The age group between 25 and 29 years old screened by HPV testing had 2.4 to 3.0 times more positivity, 13.0% colposcopy referral, twice more than women aged 30 to 39 years old (7.7%; p < 0.0001), and detected 20 CIN3 and 3 early-stage cancer versus 9 CIN3 and no cancer by cytology screening (CIN3 OR= 2.10; 95%CI: 0.91 -5.25; p = 0.043). The PPV of colposcopy for CIN2+ ranged from 29.5 to 41.0% in the HPV testing program.
There was a significant increase in detections of cervix precancerous lesions in a short period of screening with HPV testing. In women < 30 years old, the HPV testing exhibited more positivity, high colposcopy referral rate, similar colposcopy PPV to older women, and more detection of HSIL and early-stage cervical cancer.