Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):325-332
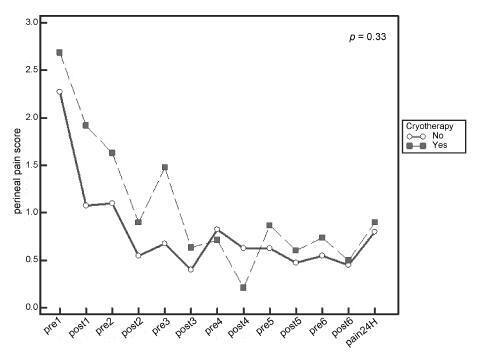
Systematic reviews that evaluate the perineal cryotherapy to reduce pain in the vaginal postpartum are inconclusive.
To evaluate clinical effectiveness of cryotherapy in the management of humanized postpartum perineal pain and vaginal edema.
A double-bind randomized controlled clinical trial (UTN number: U1111- 1131-8433) was conducted in a hospital in Northeastern, Brazil.Women were included following humanized childbirth. All had vaginal deliveries of a single, full-term pregnancy with cephalic presentation. Exclusion criteria included previous perineal lesion, episiotomy during the current delivery, instrumental delivery, uterine curettage and postpartum hemorrhage. In the experimental group, an ice pack was applied six times on the perineum for 20 minutes, reducing the temperature between 10 and 15° C, then 60 minutes without exposure to cold. In the non-cryotherapy, a water bag unable to reduce the temperature to this extent was used, compliance with the same application protocol of the first group. Perineal temperature wasmonitored at zero, 10 and 20 minutes for application in both groups. Evaluations were made immediately before and after the applications and 24 hours after delivery spontaneous, to determine the association between variables.
A total of 80 women were included in the study, 40 in each group. There was no significant difference in scores of perineal pain and edema between the groups with or without cryotherapy until 24 hours after childbirth. There was no difference between groups when accomplished repeated measures analysis over the 24 hours after delivery, considering the median perineal pain (p = 0.3) and edema (p = 0.9). Perineal cryotherapy did not influence the amount of analgesics used (p = 0.07) and no adverse effect was registered.
The use of cryotherapy following normal vaginal delivery within the concept of humanized minimally interventionist childbirth had no effect on perineal pain and edema, since it was already substantially lower, nor the need for pain medicaments.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):333-339
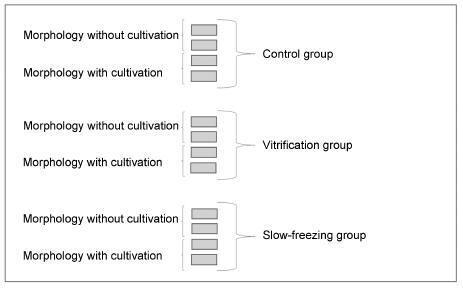
To assess the viability of bovine ovarian tissue after cryopreservation through either slow freezing or vitrification, and to compare it to that of control tissue by performing morphological analyses.
The study included 20 bovine ovarian cortex fragments that were divided into control, vitrification, and slow freezing groups. Each group consisted of four fragments of the same ovary, two fixed without cultivation, and two fixed with cultivation. Tissues were evaluated based on follicular morphology immediately after heating and after 7 days of culture, and compared with the control group.
A total of 240 fragments were analyzed, generating a sample of 1,344 follicles without cultivation and 552 with cultivation. When the non-cultivated samples were classified as non-atretic follicles, 572 were found in the control group, 289 in the vitrification group, and 373 in the slow freezing group, showing no significant differences. When classified as atretic, 46 follicles were found in the control group, 23 in the vitrification group, and 41 in the slow freezing group, also showing no statistical difference. In the post-culture sample, an evolution of the follicular stages could be observed. This finding was important to support that the follicles considered non-atretic in the non-cultivated group were actually viable in the morphological evaluation.
With no differences between the protocols, vitrification was shown to be an advanced and alternative method for patients who will undergo treatments that
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):340-347
Aerobic exercises may improve quality of life (QoL) in women with polycystic ovary syndrome (PCOS). However, there is no data on the effect of resistance exercise training (RET) programs on the QoL of women with PCOS. Thus, this study aimed to assess the effect of a 16-week RET program on QoL in PCOS women.
This 16-week case-control study enrolled 43 women with PCOS (PCOS group, PCOSG) and 51 healthy pre-menopausal controls aged 18 to 37 years (control group, CG). All women underwent a supervised RET program for 16 weeks, and were evaluated in two different occasions: week-0 (baseline), and week-16 (after RET). Quality of life was assessed using the 36-Item Short Form Health Survey (SF-36).
Testosterone reduced significantly in both groups after RET (p < 0.01). The PCOSG had improvements in functional capacity at week-16 relative to week-0 (p = 0.02). The CG had significant improvements in vitality, social aspects, and mental health at week-16 relative to week-0 (p ≤ 0.01). There was a weak correlation between social aspects of the SF-36 domain and testosterone levels in PCOS women.
A 16-week RET program modestly improved QoL in women with PCOS.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):348-355
To identify the epidemiological risk factors for congenital anomalies (CAs) and the impact of these fetal malformations on the perinatal outcomes.
This prospective cohort study comprised 275 women whose fetuses had CAs. Maternal variables to establish potential risk factors for each group of CA and perinatal outcomes were evaluated. The primary outcome was CA. Secondary outcomes included: fetal growth restriction (FGR); fetal distress (FD); premature rupture of membranes (PROM); oligohydramnios or polyhydramnios; preterm delivery (PTD); stillbirth; cesarean section; low birth weight; Apgar score < 7 at the 1st and 5th minutes; need for assisted ventilation at birth; neonatal infection; need for surgical treatment; early neonatal death; and hospitalization time. Chi-square (x2) test and multilevel regression analysis were applied to compare the groups and determine the effects of maternal characteristics on the incidence of CAs.
The general prevalence of CAs was of 2.4%. Several maternal characteristics were associated to CAs, such as: age; skin color; level of education; parity; folic acid supplementation; tobacco use; and history of previous miscarriage. There were no significant differences among the CA groups in relation to FGR, FD, PROM, 1-minute Apgar score > 7, and need for assisted ventilation at birth. On the other hand, the prevalence of the other considered outcomes varied significantly among groups. Preterm delivery was significantly more frequent in gastrointestinal tract/abdominal wall defects. The stillbirth rate was increased in all CAs, mainly in isolated fetal hydrops (odds ratio [OR]: 27.13; 95% confidence interval [95%CI]: 2.90-253.47). Hospitalization time was higher for the urinary tract and congenital heart disease groups (p < 0.01). Neonatal death was significantly less frequent in the central nervous system anomalies group.
It was possible to identify several risk factors for CAs. Adverse perinatal outcomes were presented in all CA groups, and may differ according to the type of CA considered.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(6):266-272
Some studies have investigated the influence of hormonal deficits and menopausal status in muscle disorders of women. However, it has not been investigated the relationship of both climacteric symptoms and the perception of quality of life with physical performance.
To evaluate the correlation of menopausal symptoms and quality of life with physical performance in middle-aged women.
This cross-sectional study was performed from April to November 2013 in the municipality of Parnamirim, in the Brazilian state, Rio Grande do Norte. The sample was composed of 497 women aged 40-65 years. The Menopause Rating Scale (MRS) and the Utian Quality of Life (UQOL) questionnaire were used to evaluate menopausal symptoms and quality of life respectively. Measures of physical performance included handgrip strength, knee extensor and flexor strengths (using an isometric dynamometer), gait speed, and chair stand test. The correlation between menopausal symptoms and quality of life with physical performance was assessed by Pearson's correlation coefficient with significance set at p< 0.05 and a confidence interval of 95 %.
There was a significant negative correlation between handgrip strength and somatic MRS score (p= 0.002) and total MRS score (p= 0.03). There was a significant correlation between knee flexor strength and sit-to-stand time and all menopausal symptom areas (p< 0.05), except psychological symptoms. There was a positive correlation between physical performance of the knee flexors and quality of life items including occupational (p= 0.001), emotional (p= 0.005), and total UQOL (p= 0.01) , but a negative correlation with sit-to-stand time and all quality of life domains (p< 0.05).
A greater intensity of menopausal symptoms and worse quality of life were related with worse physical performance. Thus, preventive measures should be implemented to avoid adverse effects on physical performance at more advanced ages.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(6):273-279
To verify sociodemographic factors associated with the occurrence of abortion in women of reproductive age, in areas covered by the Family Health Strategy (FHS), a program from the Brazilian Ministry of Health.
A cross-sectional study using household surveys of 350 women aged 15 to 49. The report of abortion was a variable indicator, and sociodemographic aspects were covariables. Prevalence ratio (PR) and respective 95% confidence intervals were used to estimate the magnitude of the associations.
There were associations among age, civil status, race/color, and religion; an increase in the prevalence of lower levels of education, age less than 20, and student status were protective factors.
The association between sociodemographic characteristics and the report of abortion is attributed to the fact that there is a lack at the FHS in the availability of fundamental healthcare services for young women; these findings call for action to guarantee the access to information about contraceptives and guidance to decrease the risk of unplanned pregnancies and abortions.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(6):280-286
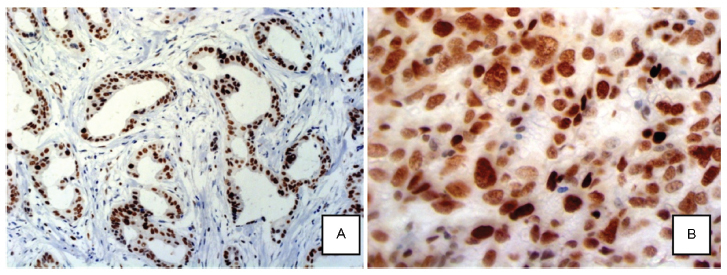
Neoadjuvant chemotherapy (NAC) is the standard treatment for locally advanced breast cancer. However, some tumors will not respond to this treatment due to histological and molecular features. The protein EZH2 (enhancer of zest homolog 2) is a histone methyltransferase that is correlated with poorly differentiated breast carcinomas and aggressive tumor behavior.
The present study evaluated the association between EZH2 expression and response to NAC, and its correlation with HER2 overexpression, estrogen and progesterone receptors (ER, PR) and Ki-67 proliferation index.
A total of 60 patients with locally advanced breast cancer treated with NAC were selected for this study. Twenty-three paraffin blocks had not enough material for tissue resection, and were not evaluated. A tissue microarray based in immunohistochemistry (IHC) analysis of EZH2 was performed for the remaining 37 specimens. Patients were divided into two groups based on response to NAC.
EZH2 expression was significantly associated with markers of poor prognosis such as ER negativity (p = 0.001), PR negativity (p = 0.042) and high Ki-67 proliferation index (p = 0.002). High EZH2 expression was not correlated with the response to NAC.
Our data suggested that EZH2 protein expression may not correlate with the clinical response to NAC. Other studies with more patients are needed to confirm this observation.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(6):287-292
betatrophin has been reported to boost β cell expansion in insulin resistant states. Pregnancy is a well-recognized physiological state of insulin resistance. Betatrophin levels in pregnant women and their relationships with metabolic variables remain to be elucidated.
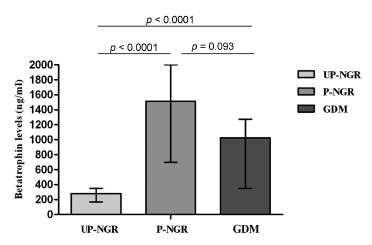
A total of 49 pregnant women and 31 age-matched unpregnant women with normal glucose regulation (UP-NGR) were included. Among these subjects, according to results from 75 g oral glucose tolerance test (OGTT), 22 women were diagnosed as having gestational diabetes mellitus ( GDM ).
Our study found that pregnant women, regardless of their glucose regulation status, had remarkably higher triglycerides (TG), total cholesterol (TC), fasting insulin (FINS), homeostasis model assessment of insulin resistance (HOMA-IR) and homeostasis model assessment of β-cell function (HOMA-β). However, GDM patients had much lower HOMA-β compared with those of pregnant women with normal glucose regulation (P-NGR). Participants of the P-NGR group had almost 4 times higher levels of betatrophin than those of the UP-NGR group. Although betatrophin levels were lower in the GDM group than those of the P-NGR group, the difference did not reach statistical significance. Spearman correlation analysis showed that betatrophin levels were positively and significantly associated with total cholesterol, triglycerides, highdensity lipoprotein cholesterol (HDL-c), FINS and HOMA-β. However, adjustments of TC, TG and HDL-c eliminated the association between HOMA-β and betatrophin.
Pregnant women have significantly higher betatrophin levels in comparison to unpregnant women. Betatrophin levels are positively and significantly associated with β cell function and lipid levels. Furthermore, lipids may contribute to