Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(9):513-515
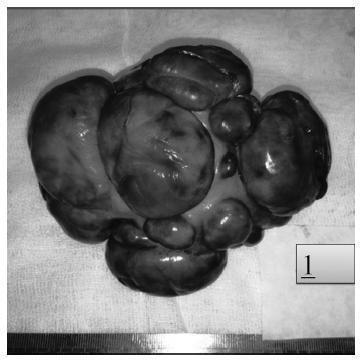
Acute abdomen secondary to epithelial ovarian cancer rupture during pregnancy is a rare event. Our aim is to present how the work of a coordinated multidisciplinary team in a case of ruptured epithelial ovarian cancer during pregnancy is feasible to obtain the best results possible. A 34-year-old woman during the 37th week of her first gestation presented with an acute abdomen. During laparotomy, a ruptured 16.5-cm left ovarian tumor was detected; the tumor was extirpated and sent to pathologic evaluation. In the meantime, a Kerr cesarean section was performed, and a healthy female neonate was born. The tumor was diagnosed as a cystadenocarcinoma; therefore, the family and the combined surgical team (obstetricians and a surgical oncologist) decided to complete a definitive radical ovarian cancer surgery: hysterectomy, right salpingooophorectomy, lymphadenectomy, omentectomy and appendectomy. The patient’s postoperative evolution was uneventful, and she was sent to adjuvant chemotherapy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(8):436-440
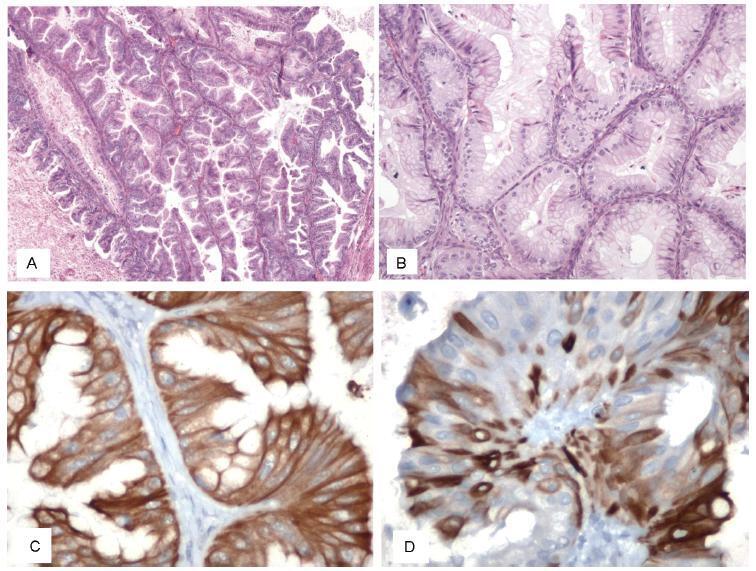
Cotyledonoid dissecting leiomyoma is a leiomyoma variant exhibiting unusual growth patterns. We aimed to demonstrate this, as well as to point out another feature that has not been previously reported.
A congested, multinodular myomectomy specimen was resected. Histologically, smoothmuscle fascicles with marked vascularity and extensive hydropic degeneration were detected. A total of 2 mitoses per 10 high power fields were counted, and the Ki-67 index was of 2-3%. We encountered atypical bizarre cells that have not been previously reported. Coagulative necrosis was not present. The patient was alive and well 36 months after surgery, with no evidence of recurrence.
Albeit the gross aggressive appearance, cotyledonoid dissecting leiomyomas are benign in nature. To this day, atypical cells have not been reported in this type of tumor. Despite the presence of symplastic features, cotyledonoid dissecting leiomyomas are clinically benign entities. Surgeons and pathologists should be acquainted with this variant.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(7):369-372
Amniotic fluid embolism (AFE) is a rare but potentially catastrophic clinical condition, characterized by a combination of signs and symptoms that reflect respiratory distress, cardiovascular collapse and disseminated intravascular coagulation (DIC). Its pathogenesis is still unclear. More recently, the traditional view of obstruction of pulmonary capillary vessels by amniotic fluid emboli as the main explanation for the etiology has been ruled out, and immunologic factors and the activation of the inflammatory cascade took on an important role. Amniotic fluid embolism has an unpredictable character, its diagnosis is exclusively clinical, and the treatment consists mainly of cardiovascular support and administration of blood products to correct the DIC. No diagnostic test is recommended until now, though multiple blood markers are currently being studied. The authors present a case report of a woman who had survived AFE in her previous pregnancy and had a subsequent pregnancy without recurrence, providing one more clinical testimony of the low risks for the pregnancy after AFE.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(6):309-314
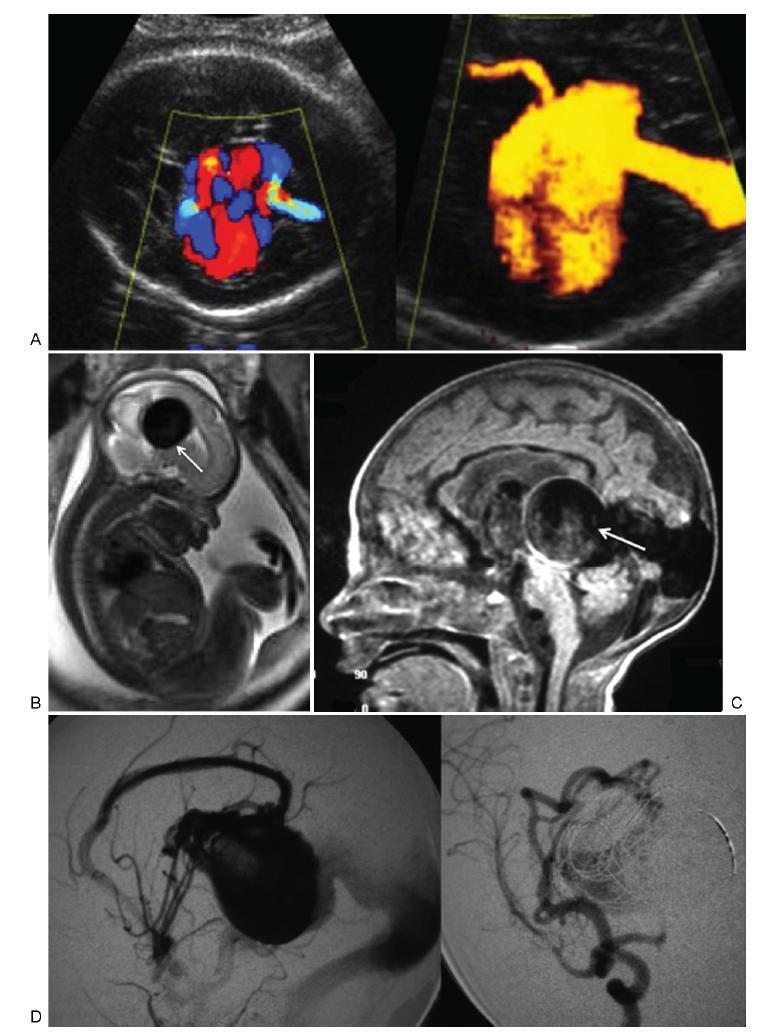
To describe the prenatal diagnosis of Galen vein aneurysm (GVA) based on ultrasonography and magnetic resonance imaging (MRI) in a series of cases, as well as its postnatal outcomes and follow-up until 4 years of age.
A retrospective longitudinal study was performed, analyzing a database comprising seven cases of prenatal diagnosis of GVA at two Brazilian institutions from February of 2000 to May of 2012. The following data were evaluated: gestational age at diagnosis, GVA dimensions on ultrasonography, associated fetal changes, findings on fetal echocardiography, gestational age at delivery, type of delivery, birth weight, Apgar score at the 1st and 5th minutes, neonatal outcomes, and survival with follow-up until 4 years of age.
The mean gestational age ± standard deviation on the prenatal diagnosis of GVA based on ultrasonography was 25±4.9 weeks. The mean length of GVA was 3.2±0.4 cm. The mean gestational age at birth was 37.5±0.7 weeks, and a cesarean section was performed in 85.7% of the cases (6/7). The mean birth weight was 3,070±240.4 g. The total survival rate was 42.8% (4/7), with three neonatal deaths. Of the four survivors, three presented with normal neuropsychomotor development until 4 years of age and only one showed serious neurological sequelae. Ultrasonography and MRI showed similar findings for all seven cases.
Galen Vein Aneurysm is associated with a high neonatal death rate. Therefore, its prenatal diagnosis is essential for parent counseling and follow-up at tertiary care institutions.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):249-254
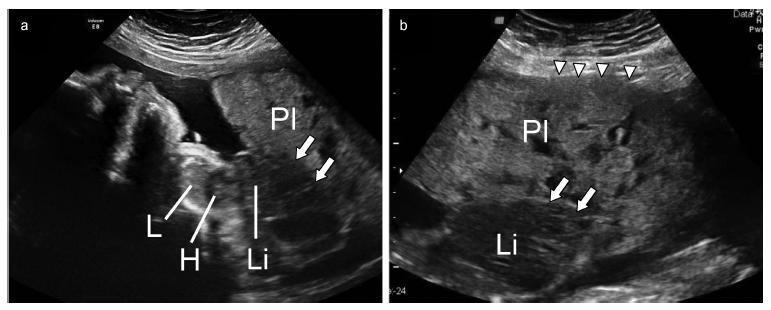
The occurrence of Manson’s schistosomiasis in organs of the female reproductive tract is an uncommon event, given that the etiological agent for this disease is a blood parasite that inhabits the mesenteric veins. In this case report, a 45-year-old female patient reported that her first symptoms had been strong pain in the left iliac region around two years earlier. An endovaginal pelvic ultrasonography showed that the left ovary was enlarged, and the report suggested that this finding might be correlated with clinical data and tumor markers. After being examined at several healthcare services, the patient was referred to an oncology service due to suspected neoplasia, where she underwent a left ovariectomy. The result from the histopathological examination showed the presence of granulomatous inflammatory processes surrounding both viable and calcified eggs of Schistosoma mansoni. There was no evidence of any neoplastic tissue. The patient was medicated and followed-up as an outpatient.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(4):195-198
A pregnancy complicated by typical hemolytic uremic syndrome (HUS) and hemolysis, elevated liver enzymes, low platelets (HELLP) syndrome is reported. At 20 weeks of gestation, a case of HUS was diagnosed, with Shiga toxin-producing Escherichia coli identified. Plasmapheresis allowed continuation of the pregnancy for 5 weeks. Superimposed preeclampsia and HELLP syndrome were diagnosed after the establishment of nephrotic range proteinuria, hypertension and recurrence of hemolysis. This is a singular case, as it demonstrates that HELLP syndrome can superimpose upon HUS, a fact that can impact future research on reproductive immunology. It also reminds clinicians that the overlapping of clinical and laboratory findings in HELLP syndrome makes the diagnosis of other thrombotic microangiopathies during pregnancy a clinical challenge.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(3):142-146
A case was reported of a fetus with the anomaly of limb body wall complex associated with placenta accreta. To date, only one account of this condition has been published in the world literature. Due to the low frequency of both complications, the hypothesis has been raised that this association may have happened not by mere coincidence, but rather by a possible common etiopathogenic mechanism. For the first time, a study proposes the existence of a possible etiopathogenic connection between the anomaly of limb body wall complex and hypoxic disorders caused by inadequate placentation in previous uterine scarring.