Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(4):214-219
DOI 10.1590/S0100-72032006000400002
PURPOSE: to evaluate the characteristics of mammography use and the social demographic profile of women accessing public and private health care services. METHODS: a cross-sectional study was carried out in the city of Taubaté, southeast Brazil. Six hundred and forty-three women who underwent mammographic examinations in the available health care services were interviewed, 472 of them in public and 171 in private health services. The social demographic and reproductive profiles of the women interviewed and the characteristics of the mammography use, such as the proportion of the women interviewed who had been previously screened, the age when the screening began, the interval between the screenings and their frequency, were evaluated by means of the Fisher exact, Wilcoxon and chi2 tests. RESULTS: the mean age of the interviewed women was similar in both studied groups. The proportion of women previously screened 54.2 and 79.5% in public and private services, respectively as well as the age when the screening began 46.8 years (SD 10.2%) in public services and 40.2 years (SD 7.7) in private services differed significantly (p<0.01). Twenty-five percent of women older than 50 years did not follow the adequate standards of periodic screening. CONCLUSIONS: the way of accessing health services has influenced the proportion of women previously screened and the age at which this screening began, being more adequate in the private health system. Although there was a later start in the public health services, the age when the mammographic screening began was earlier than the current official recommendations. There has been a failure of compliance with mammographic screening in women older than 50 years, in both researched groups.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(4):220-226
DOI 10.1590/S0100-72032006000400003
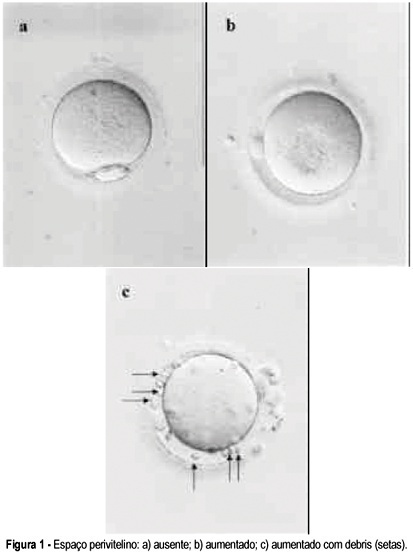
PURPOSE: to verify the possibility of identifying oocytes that would result in a higher fertilization rate. METHODS: retrospective analysis of the fertilization rate after ICSI of 957 oocytes in metaphase II according to three morphology parameters: cytoplasm inclusions, thickness of the perivitelline space, and fragmentation of the first polar body. Oocytes were obtained from 115 cycles performed among 107 women attended at the "Centro de Reprodução Humana de Campinas", from April to December of 2004. For the statistical analysis of differences in the fertilization rate between 'normal' oocytes and those presenting each alteration, the chi2 test was used with confidence levels of 5 and 10%. RESULTS: no significant difference in fertilization rate was observed regarding characteristics of the polar body or thickness of the perivitelline space. Fertilization rate among oocytes with perivitelline space with debris was 14 percentage points lower than among oocytes with absent space (p=0.055) and the rate among oocytes with granular cytoplasm was seven percentage points lower than among oocytes with normal cytoplasm (p<0.10>0.05). CONCLUSIONS: the morphological parameters of oocytes currently being evaluated do not allow us to clearly distinguish those that would lead to a higher fertilization rate and could be used in clinical practice.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(4):227-231
DOI 10.1590/S0100-72032006000400004
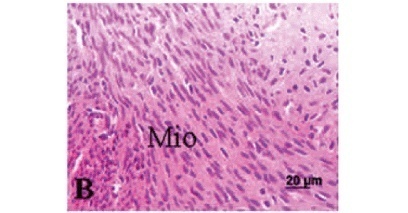
PURPOSE: to evaluate histomorphometric changes in the rat myometrium upon treatment with isoflavones, as compared with estrogens, using histological and morphometric techniques. METHODS: twenty-eight oophorectomized adult rats were randomly divided into four treatment groups: GPropi = propylene glycol (control); GExtr10 - 10 mg/kg soybean extract; GExtr300 - 300 mg/kg soy bean extract; GCee - 200 µg/kg conjugated equine estrogens (Cee). Drugs or drug vehicle were administered by gavage once a day for 21 days. Upon sacrifice, the uteri were removed and weighed. Fragments of uterine horns were collected and fixed in 10% formaldehyde and processed for paraffin inclusion. The histological sections were stained by hematoxylin and eosin and evaluated microscopically by means of an image analyzer to quantify the myometrial thickness and the number of blood vessels and eosinophils. The data were studied by analysis of variance (ANOVA) followed by the Tukey-Kramer multiple comparison test. RESULTS: isoflavones in the concentration of 300 mg/kg induced a significant increase in the myometrium thickness (GExtr300=25.6±5.0 mm) compared to control (GPropi=5.5±0.5 mm). The effect of this high dose is similar to the estrogen effect (GCee=27.5±7.9 mm). In low doses (10 mg/kg), the effect was similar to control. Isoflavones (GExtr300) induced also an increase in the number of blood vessels (GPropi=3.5±1.6; GExtr300=10.2±3.6 vessels/mm²) and of eosinophils (CPropi=0.15±0.01; GExtr300=4.3±0.9 eosinophils/mm²). These effects were comparable to those produced by Cee treatment in GCee (9.2±1.1 eosinophils/mm²). CONCLUSION: a high-dose treatment with isoflavones (300 mg/kg per day, 21 days) elicited an estrogen-like, highly significant proliferative action on the rat myometrium.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(4):232-237
DOI 10.1590/S0100-72032006000400005
PURPOSE: to identify maternal and perinatal factors related to neonates with birthweight >4,000 g. METHODS: cross-section cohort study with 411 consecutive cases of fetal macrosomia (FM) which occurred from March 1998 to March 2005. Data were compared to 7,349 cases of fetal birthweight >2,500 and <3,999 g which occurred in the same period. Maternal variables (maternal age, parity, diabetes, previous cesarean section, meconium-stained amniotic fluid, cephalopelvic disproportion, main cesarean section indications) and perinatal variables (birth injury, <7 1-min and 5-min Apgar score, fetal and early neonatal mortality range, need of neonatal intensive care unit) were analyzed. For statistical analysis the chi2 test with Yates correction and Student's t test were used with the level of significance set at 5%. RESULTS: FM was significantly associated with older mothers, more parous and <7 1-min Apgar score (p<0.05; OR=1.8; 95% CI: 1,4-2.5) and <7 5-min Apgar score (p<0,05; OR=2.3; 95% CI: 1.3-4,1), diabetes mellitus (p<0.05; OR=4.2; 95% CI: 2.7-6.4), meconium-stained amniotic fluid (p<0.02; OR=1.3; 95% CI: 1.0-1.7), need of neonatal intensive care unit (p<0,05; OR=2.0; 95% CI: 1.5-2.7), early neonatal mortality (p<0,05; OR = 2.7; 95% CI: 1.0-6.7), cesarean section (p < 0.05; OR = 2.03; 95% CI: 1,6-2,5) and cephalopelvic disproportion (p < 0.05;OR = 2.8; 95% CI: 1.6-4,8). There was no statistical difference between birth injury and fetal mortality range. In the FM group the main cesarean section indications were repeat cesarean sections (11.9%) and cephalopelvic disproportion (8.6%); in the normal birthweight group, repeat cesareans (8.3%) and fetal distress during labor (3.9%). CONCLUSIONS: in spite of the characteristic limitations of a retrospective evaluation, the analysis demonstrated which complications were associated with large fetal size, being useful in obstetric handling of patients with a diagnosis of extreme fetal growth. FM remains an obstetric problem of difficult solution, associated with important maternal and perinatal health problems, due to the significant observed rates of maternal and perinatal morbidity and mortality in developed and developing countries.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(4):238-243
DOI 10.1590/S0100-72032006000400006
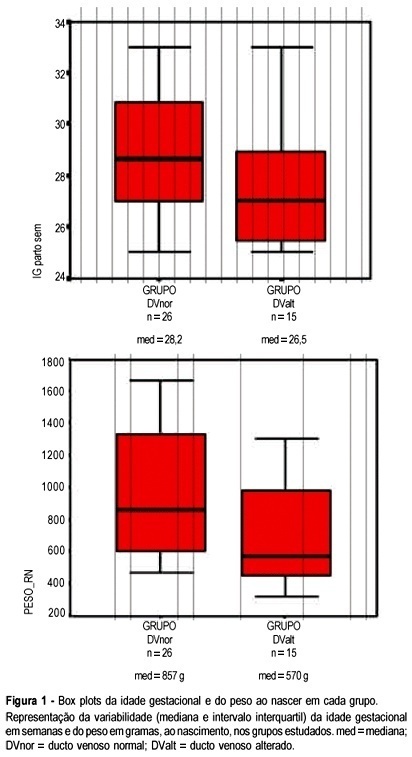
PURPOSE: to evaluate the relationship between S/A ratio in ductus venosus (DV) and perinatal outcomes in fetuses with brain sparing reflex. METHODS: the study was designed as an observational, sectional study with prospectively collected data. Forty-one fetuses with brain sparing reflex and gestational age between 25 and 33 weeks were studied between November 2002 and July 2005. The newborns were observed during the neonatal period in the intensive care unit of "Clínica Perinatal Laranjeiras" in order to find adverse outcomes. The study population was divided into two groups according to DV assessment. In the normal group all the fetuses with S/A ratio values of 3.6 or less were included, and in the abnormal group the fetuses with values of S/A ratio greater than 3.6. The statistical analysis was performed by the Mann-Whitney U-test, chi2 test and Fisher exact test. The results were considered significant when p<0.05. Gestational age, birth weight and Apgar score less than 7 at 5 min were evaluated. Perinatal outcome parameters were: intrauterine death, neonatal mortality, seizures, intraventricular hemorrhage, leukomalacia, need of surfactant, mechanical ventilation, myocardical failure, necrotizing enterocolitis, and length of stay in the intensive care unit. RESULTS: among the assessed 41 fetuses, 26 (63.4%) showed normal DV S/A ratio and the other 15 (36.6%) developed an abnormal DV S/A ratio (>3.6). There was no statistically signicant difference between the groups according to gestational age at delivery and Apgar <7. The only significant association was between abnormal DV S/A ratio and neonatal death (p=0.049; Fisher's exact test). No statistically significant association was observed for the other studied variables. CONCLUSIONS: our results suggest that abnormal DV blood flow detected by Doppler examination is not associated with adverse perinatal outcomes, except for neonatal mortality. This association may be considered statistically borderline (p=0.049). Excluding fetuses with birth weight less than 400 g, there was no other association between DV and neonatal mortality. The abnormal DV S/A ratio was not associated, in our study, with perinatal mortality in viable preterm fetuses.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(2):101-106
DOI 10.1590/S0100-72032006000200005
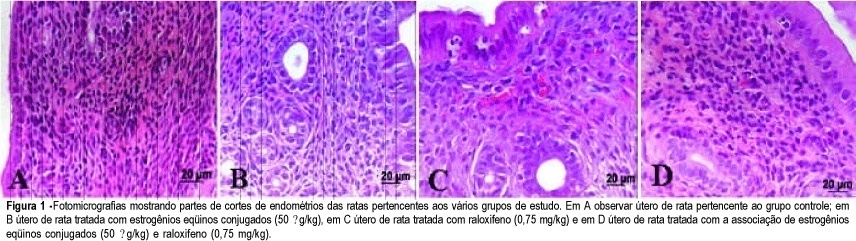
PURPOSE: to evaluate the effects of conjugated equine estrogens (CEE) and raloxifene (Ral), alone or combined, on the rat endometrium. METHODS: fifty-six adult rats were ovariectomized and randomly divided into seven groups: GCont (control); GCEE (CEE 50 µg/kg); GCEE/25 (CEE 25 µg/kg); GRal/0.75 (Ral 0.75 mg/kg); GRal/0.4 (Ral 0.4 mg/kg); GCEERal (50/0.75) - (CEE 50 µg/kg + Ral 0.75 mg/kg), and GCEE-Ral (25/0.4) - (CEE 25 µg/kg + Ral 0.4 mg/kg). The drugs were orally administered (gavage) for 21 consecutive days. At the end of the experiment, all animals were anesthetized and sacrificed. Fragments of uterus were removed, fixed in 10% formaldehyde and processed for paraffin inclusion. The histological sections were stained by HE and submitted to histomorphometric evaluation. The following parameters were analyzed: thickness of superficial epithelium and number of endometrial glands/mm² and of blood vessels/mm². The data were evaluated using ANOVA followed by the Turkey-Kramer test. RESULTS: in the GCont and only Ral treatment (GRal/0.75 and GRal/0.4) the endometrium showed signals of atrophy. In the groups treated with only CEE signs of endometrial proliferation were observed, mainly in group GCEE/50. Also, there was endometrial proliferation in the groups that received combined CEE and Ral (Ral GCEE (50/0.75) and GCEE-Ral (25/0.4)), but it was more intensive in the animals treated with isolated estrogen than in those that received combined estrogen and raloxifene. CONCLUSION: raloxifene may partially block the action of estrogen on the castrated adult rat endometrium.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(2):107-111
DOI 10.1590/S0100-72032006000200006
PURPOSE: we report a small series of pregnant women who underwent gastric bypass surgery for severe obesity, with a review of the literature on this topic. METHODS: five consecutive cases of pregnancy after gastroplasty between 2001 and 2004 were evaluated, and clinical, laboratory and therapeutic features were considered. Patients were 30 to 34 years old and all had been submitted to gastroplasty by the Capella technique. The outcomes for both the pregnant woman and the fetus were evaluated. A search of the English language literature was done through MEDLINE and Web of Science databases with the following terms: gastroplasty, gastric bypass surgery, bariatric surgery, and pregnancy. RESULTS: all 5 pregnancies were singleton. No major obstetric complications were observed and there were no premature or lowbirth weight infants. CONCLUSION: our data suggest that pregnancy following gastroplasty is safe for mother and fetus. However, since information about this topic is limited, further investigations are required to establish appropriate recommendations concerning the follow-up of these pregnancies.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(2):112-121
DOI 10.1590/S0100-72032006000200007
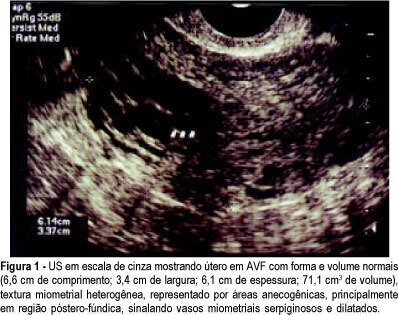
PURPOSE: to investigate the presence and outcome of uterinevascular malformations (UVAM) after gestational trophoblastic disease (GTD). METHODS: retrospective study of 2764 patients with GTD diagnosed from 1987 to 2004. All patients were followed up annually at the "Santa Casa da Misericórdia" Trophoblastic Disease Center (Rio de Janeiro, RJ, Brazil) with transvaginal ultrasonography (US) and color Doppler imaging. Seven patients had a final diagnosis of UVAM based on ultrasonographic analysis - pulsatility index (PI), resistance index (RI), peak systolic velocity (PSV) - and pelvic magnetic nuclear resonance (MNR) findings. Negative beta-hCG values were of utmost importance to establish differential diagnosis with persistent GTD. RESULTS: the incidence of UVAM after GTD was 0.2% (7/2764). US features of UVAM: PI mean 0.44±0,058 (extremes: 0.38-0.52); RI mean 0.36±0.072 (extremes: 0.29-0.50); PSV mean 64.6±23.99 cm/s (extremes: 37-96). MNR image showed a bulky uterus, myometrial inhomogeneity, serpiginous flow-related signal voids, and prominent parametrial vessels. The most common UVAM clinical presentation was vaginal hemorrhage, present in 52.7% (4/7). Pharmacological management with 150 mg medroxyprogesterone acetate was employed to control bleeding, after hemodynamic stabilization. These patients are still being followed and remain asymptomatic nowadays. Two patients with persistent UVAM became pregnant and had successful outcomes. CONCLUSION: patients with antecedent of GTD presenting transvaginal bleeding and negative beta-hCG may be considered to have UVAM and should be investigated through US with Doppler velocimetry. Conservative management is a valuable option in many of the acquired UVAM after GTD.