Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(1):24-31
DOI 10.1590/S0100-72032005000100006
PURPOSE: to compare the effectiveness and safety of sublingual misoprostol (25 µg) versus vaginal misoprostol (25 µg) (Prostokos®) for labor induction with gestational age > 37 weeks and unripe cervices. METHODS: a randomized controlled clinical trial was performed at the Maternidade Monteiro de Morais (CISAM-UPE), in Recife - PE, Brazil, from October 2003 to February 2004. One hundred and twenty-three women with gestational age > 37 weeks, Bishop score <8, not in labor and with medical indication for interruption of pregnancy were included in this study. The women received randomly 25 µg sublingual misoprostol or 25 µg vaginal misoprostol every 6 h, not exceeding eight doses. In order to evaluate the differences between the groups, means, standard deviations, Student's t-test, c² trend and Mann-Whitney test were used. The statistical significance was considered to be 5%. RESULTS: there were no significant differences between the number of women with vaginal delivery in the sublingual group as compared with the vaginal group (65.5 vs 75.8%, p<0.22), or in the interval of time between the induction onset and delivery (24 h and 42 min vs 20 h and 37 min respectively, p=0.11). The two groups, sublingual and vaginal, also did not differ as to the hyperstimulation syndrome (1.7 vs 3.2%, p=0.95), meconium incidence (5.2 vs 4.8%, p=0.74), Apgar score <7 at 5 min (3.4 vs 4.8%, p=0.98) and other adverse effects. CONCLUSION: twenty-five micrograms of sublingual misoprostol every six h presented the same effectiveness and safety as an equal vaginally administered dose of this substance. Sublingual misoprostol seems to be acceptable and is another option to be considered for labor induction.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(1):32-36
DOI 10.1590/S0100-72032005000100007
PURPOSE: to evaluate the prevalence of HIV infection in parturient women from maternity hospitals linked to the Public Health Service in Sergipe state (Brazil) using the rapid test, and to evaluate this strategy to introduce the protocol for adequate management of HIV patients. METHODS: cross-sectional study which included the training of all health personnel and enrollment of every parturient woman admitted to maternity hospitals linked to the Public Health Service of Sergipe in the Northeast of Brazil. They received instructions about HIV perinatal transmission, were asked to undertake the rapid test, independently of their knowledge about their HIV serologic status, and signed the term of free consent. Additional information about antenatal care and obstetric history was obtained. The test used was the DetermineTM - Abbott Laboratories, and we used the Health Ministry protocol for HIV infeccion prophylaxis. A database was created at Epi-Info 2002, and the prevalence was calculated in relation to all tests performed from January 2003 to March 2004. RESULTS: after 9215 performed tests, 39 HIV-seropositive patients (0.42%) were detected. Twenty-three of them (59%) had no previous knowledge about their seropositivity. Two patients that already knew their positive sorology status did not refer this condition to the health persomel. The Health Ministry protocol was used for all positive cases. Antenatal care attendance was high (89%) but only 32.5% of the patients had already been submitted to an HIV serologic test during pregnancy. CONCLUSIONS: HIV prevalence in pregnant women (0.42%) in Sergipe was similar to the average rate in Brazil. A large number of seropositive pregnant women did not know their serologic status at the moment of delivery. This indicates bad antenatal care performance and the necessity to keep using HIV rapid test at the moment of labor and delivery in order to reduce vertical transmission.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(1):37-43
DOI 10.1590/S0100-72032005000100008
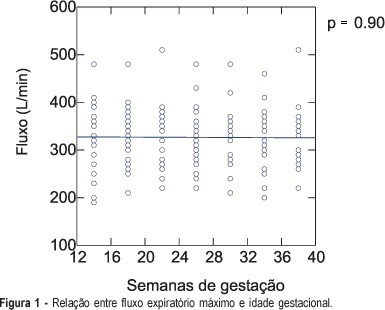
PURPOSE: to investigate the normal peak expiratory flow values in healthy pregnant women employing a portable expiratory apparatus (Mini-Wright Peak Flow Meter), and to relate the obtained measurements to each patient's height, body mass index (BMI) and age, along gestation. METHODS: a longitudinal prospective study including 26 pregnant women followed up from the first trimester to the 36th week of gestation and examined every four weeks. On the occasion of seven visits, the pregnant women performed forced exhaling into a portable expiratory apparatus three times, with the highest value being considered the peak expiratory flow. All measurements were made under the same investigator's supervision in order to reduce the margin of error. Pearson coefficient was used to calculate the correlation between flow and BMI, between flow and patient's height, and between flow and patient's age. RESULTS: the variation in flow values during pregnancy can be determined by flow = 328.32 -0.07 x week, with a Pearson coefficient equal to zero. To determine whether there was a difference in the correlation coefficients between BMI and flow, we compared the lowest coefficient (0.47 for week 30, flow = 123.49 + 7.64 x BMI) with the highest coefficient (0.59 for week 34, flow = 87.77 + 9.05 x BMI) of each studied time interval and obtained a value of 0.22, indicating a good correlation between the flow and BMI variables. There was a positive correlation between height and flow (Pearson = 0.61), with flow = -477.47 + 497.38 x height. The correlation coefficient between flow and age was 0.24, with the equation obtained in this case being non-linear. CONCLUSIONS: peak expiratory flow values did not change along gestation. Higher flows were observed in taller women. Pregnant women with a higher BMI before gestation presented higher flows. There was no correlation between flow and maternal age.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(1):7-11
DOI 10.1590/S0100-72032005000100004
PURPOSE: to identify factors associated with climacteric symptoms. METHODS: a cross-sectional study of 254 women aged between 45 and 60 years was carried out at the Climacterium Outpatient Clinic of Caxias do Sul University, RS, from June to October 2002. Women with previous hysterectomy or under hormonal therapy were excluded. The climacteric symptoms were evaluated by means of the Kuppermann index and the attitudes toward menopause by a specific questionnaire. Data were analyzed by Student's t test, analysis of variance (ANOVA) and multiple linear regression analysis. RESULTS: twenty eight percent of the women reported mild climacteric symtoms, whereas 42.3% reported moderate symptoms and 30.7%, intense symptoms. The most prevalent symptoms were: irritability (87.1%), arthralgias/myalgias (77.5%) and melancholy (73.2%), while the most severe were hot flushes in 60.2% of the women, irritability and insomnia. Attitudes toward menopause, skin color and physical activity were predictors of climacteric symptoms. Positive attitudes toward menopause (p=0.01), white color (p=0.02) and the habit of practicing physical activity (0.04) were associated with less intense climacteric symptoms. Negative attitudes toward menopause were associated with worse climacteric symptoms (p<0.01). CONCLUSIONS: in the current study, the climacteric symptoms were influenced by psychosocial factors and physical activity, as well as by climacteric hypoestrogenism.