Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):580-587
DOI 10.1590/S0100-72032005001000003
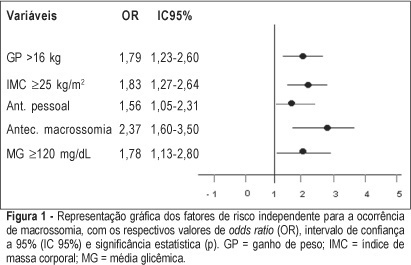
PURPOSE: to identify risk factors for fetal macrosomia in pregnant women with diabetes or daily hyperglycemia. METHODS: retrospective study, control-case, including 803 pairs of mothers and newborns belonging to this specific population, divided into two groups - macrosomic (cases, n=242) and non-macrosomic (controls, n=561). Variables regarding age, parity, weight and body mass index (BMI), weight gain (WG), diabetes history, high blood pressure and tabagism, diabetes type and classification, and glycemic control indicators in the third trimester were compared. The means were evaluated by the F test and the categorized variables were submitted to univariate analysis using the chi² test. The significative results were included in the multiple regression model for the identification of macrosomia independent risk considering OR, 95% CI and p value. The statistical significance limit of 5% was established for all analyses. RESULTS: there was a significative association between macrosomia and WG >16 kg, BMI >25 kg/m², personal, obstetric and macrosomic history, classification in the Rudge groups (IB and IIA + IIB), glycemic mean (GM) >120 mg/dL and postprandial glycemic mean >130 mg/dL in the third trimester. In the multiple regression analysis, WG >16 kg (OR=1,79; 95% CI: 1,23-1.60), BMI >25 kg/m² (OR=1.83; 95% CI: 1.27-2.64), personal history of diabetes (OR=1.56; 95% CI: 1.05-2.31) and of macrosomia (OR=2.37; 95% CI: 1.60-3.50) and GM >120 mg/dL in the third trimester (OR=1.78; 95% CI: 1.13-2.80) confirmed to be independent risk factors for macrosomia in these pregnancies. CONCLUSION: WG >16 kg, BMI >25 kg/m², GM >120 mg/dL in the third trimester and personal history of macrosomia and diabetes were identified as risk factors for fetal macrosomia in pregnant women with diabetes or daily hyperglycemia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):575-579
DOI 10.1590/S0100-72032005001000002
PURPOSE: to verify the occurrence of colonization by Streptococcus agalactiae in pregnant women attended at the prenatal outpatient clinic of the Teaching Maternity Hospital of Rio de Janeiro University (UFRJ) and to evaluate the susceptibility of the isolates to antimicrobial agents. METHODS: a total of 167 pregnant women between the 32nd and 41st week of gestation, regardless of risk factors, attended at the antenatal clinic between February 2003 and February 2004, were evaluated. The vaginal/anal material, collected by the same swab, was inoculated in Todd-Hewitt broth to which nalidixic acid (15 µg/mL) and gentamicin (8 µg/mL) were added, with following subcultures onto sheep blood-agar. Identification was carried out observing colony morphology and beta-hemolysis type on blood-agar, catalase, cAMP, and serological tests. The antimicrobial susceptibility testing used agar diffusion and agar dilution methods. Statistical analysis was performed by the chi2 test with the level of significance set at p<0,05. RESULTS: the frequency of colonization was 19.2%, with no significant differences when age, number of gestations, number of abortions and the presence or absence of diabetes mellitus were compared (p>0.05). All 32 isolated strains were susceptible to penicillin, cefotaxime, ofloxacin, chloramphenicol, vancomycin and meropenem. Resistance to erythromycin and clindamycin was detected in 9.4 and 6.2% of the isolates, respectively. CONCLUSIONS: the relatively high incidence (19.2%) of colonization by S. agalactiae among the evaluated pregnant women and the recovery of antimicrobial resistant strains, especially those recommended in cases of penicillin allergy, emphasize the importance, for a correct prevention of neonatal infections, of detecting colonization at the end of pregnancy and evaluating antimicrobial susceptibility.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(9):554-560
DOI 10.1590/S0100-72032005000900009
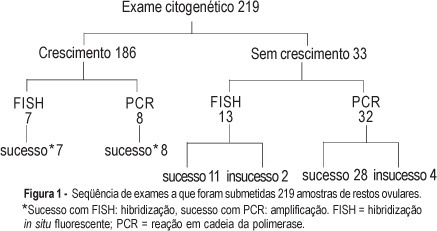
PURPOSE: to evaluate the performance of cytogenetic analysis, fluorescent in situ hybridization (FISH) and polymerase chain reaction (PCR) in the study of numerical chromosomal anomalies and in fetal sex determination of spontaneous abortion material. METHODS: cytogenetic analysis was performed on 219 spontaneous abortion specimens. Forty of these cases were also submitted to fetal sex determination using nested-PCR. Thirty-two of these cases were selected due to failed cytogenetic culture and the other eight were selected randomly. Twenty samples were submitted to the FISH technique, using probes for chromosomes 13, 18, 21, X and Y. Thirteen of these samples were selected due to failed cytogenetic culture and the other seven were randomly selected. The success rates of each technique were compared using the chi2 test and an established p<0.05 level of significance. The results of samples submitted to more than one test were evaluated for accuracy, using the cytogenetic result as the gold standard. RESULTS: cytogenetic analysis was successful in 84.9% of the samples and in 51.1% of them the results were abnormal: 65.2% trisomy, 17.9% triploidy, 9.4% tetraploidy, 4.2% chromosome X monosomy, and 1.1% each for double trisomy, tetrasomy and structural abnormality. The most frequent trisomy was that of chromosome 16 (39%). The success rate of FISH and PCR techniques (90%) did nod differ significantly from the cytogenetic analysis. In all cases submitted to more than one test, the results were identical to those obtained through cytogenetic analysis. Samples that failed to grow on cytogenetic test and that were submitted to other techniques of molecular biology had a success rate of 87.5 and 84.6% for PCR and FISH, respectively. CONCLUSION: cytogenetic analysis of spontaneous abortions had a high success rate and chromosomal anomalies were identified in over half of the cases. Molecular biology techniques (PCR and FISH) complemented the cytogenetic study and proved to be reliable in the detection of numerical chromosomal anomalies and in fetal sex determination.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(9):548-553
DOI 10.1590/S0100-72032005000900008
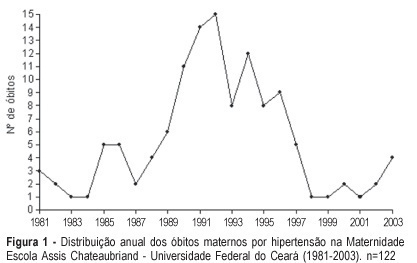
PURPOSE: to study maternal mortality caused by hypertension during pregnancy, determining the mortality rate and the profile of those patients. METHODS: a retrospective study of maternal mortality caused by hypertension at the Maternidade Escola Assis Chateaubriand of the Universidade Federal do Ceará, from 1981 to 2003. General maternal mortality rate (MMR) and specific maternal mortality rate due to hypertension were evaluated, as well as these patients' epidemiological and clinical data. RESULTS: two hundred and ninety six cases of maternal death and 184,672 of live births were recorded, with a MMR of 160.28/100.000 live births. The most frequent cause of death was hypertension (41.2%); with 122 cases and an annual average of 5.3 deaths, and hypertension MMR of 60.10/100,000 live births. The women's age range varied from 13 to 42 years with an average of 26 years. Most of the patients came from the interior of the state. Deaths occurred predominantly in the first 24 hours after admission to the hospital (50.9%). Deaths were predominant in the first pregnancy (40.3%) and in women with 31 to 38 weeks gestational age (48.2%). Eclampsia occurred in 73 patients (64.1%) and was predominant along the gestational period (53.4%). There were 101 deaths in the puerperium. Cesarean section (62.3%) and general anesthesia (45.1%) prevailed. A high percentage of patients (61.4%) had no prenatal care. CONCLUSIONS: General MMR and hypertension MMR were high, the latter being the main cause of death in our maternity hospital.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(9):534-540
DOI 10.1590/S0100-72032005000900006
PURPOSE: to evaluate the role of morphological (12) and Doppler velocimetry (17) ultrasonographic features, in the detection of lymph node metastases in breast cancer patients. METHODS: 179 women (181 axillary cavities) were included in the study from January to December 2004. The ultrasonographic examinations were performed with a real-time linear probe (Toshiba-Power Vision-6000 (model SSA-370A)). The morphological parameters were studied with a frequency of 7.5-12 MHz. A frequency of 5 MHz was used for the Doppler velocimetry parameters. Subsequently, the women were submitted to level I, II and III axillary dissection (158), or to the sentinel lymph node technique (23). Sensitivity, specificity, and positive and negative predictive values were calculated for each parameter. The decision tree test was used for parameter association. The cutoff points were established by the ROC curve. RESULTS: at least one lymph node was detected in 173 (96%) of the women by the ultrasonographic examinations. Histological examination detected lymph node metastases in 87 women (48%). The best sensitivity among the morphological paramenters was found with the volume (62%), the antero-posterior diameter (62%) and the fatty hilum placement (56%). Though the specificity of the extracapsular invasion (100%), border regularity (92%) and cortex echogenicity (99%) were high, the sensitivity of these features was too low. None of the Doppler velocimetry parameters reached 50% sensitivity. The decision tree test selected the ultrasonographic parametners: fatty hilum placement, border regularity and cortex echogenicity, as the best parameter association. CONCLUSION: the detection of axillary cavity lymph node stage by a noninvasive method still remains an unfulfilled goal in the treatment of patients with breast cancer.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(9):541-547
DOI 10.1590/S0100-72032005000900007
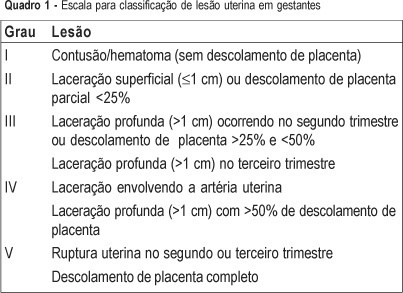
PURPOSE: to evaluate the predictors (clinical findings and physiological and anatomical scores) of the maternal and fetal outcomes among pregnant women victims of abdominal trauma who were submitted to laparotomy and to discuss particularities of assessment in this situation. METHODS: retrospective analysis of the medical records of 245 women with abdominal trauma and surgical treatment, from 1990 to 2002. Thirteen pregnant women with abdominal injury were identified. All cases were registered in the Epi-Info 6.04 protocol and data were analyzed statistically by the Fisher exact test, with confidence interval of 95%. RESULTS: ages ranged from 13 to 34 years (mean of 22.5). Six women (46.2%) were in the third trimester of pregnancy. Penetrating trauma accounted for 53.8% of injuries and in six of these patients the mechanism of trauma was gunshot wounds. Three patients had uterine injuries associated with fetal death. There were no maternal deaths and fetal mortality was 30.7%. The use of trauma scores was not associated with maternal and fetal mortality. Uterine injury was the only predictive risk factor for fetal loss (p=0.014). CONCLUSIONS: this is a retrospective study analyzing a small number of pregnant women victims of severe trauma. However, the results show that there are no predictive accuracy scores to evaluate maternal and fetal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(9):524-528
DOI 10.1590/S0100-72032005000900004
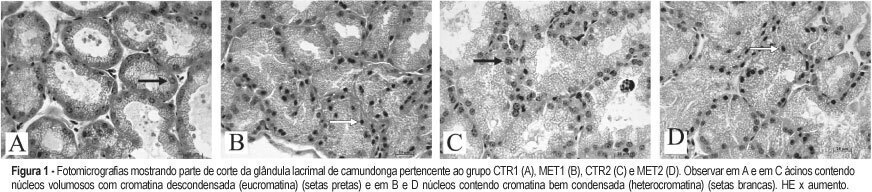
PURPOSE: to evaluate the morphological changes in murine lacrimal glands by metoclopramide-induced hyperprolactinemia during the proestrus phase or pregnancy. METHODS: forty adult mice were divided into two groups: CTR1 (control) and MET1 (treated with metoclopramide). After fifty days, half of the mice were sacrificed. The remaining animals were mated, and then labeled as pregnant controls (CTR2). Part of these animals were treated with metoclopramide and constituted the metoclopramide-treated pregnant (MET2) group. The CTR2 and MET2 groups were sacrificed on the 6th day of pregnancy. The blood was collected for determination of the hormonal levels of estradiol and progesterone by a chemoluminescent method. The lacrimal glands were then removed, fixed in 10% formaldehyde and stained with HE. The morphometric analysis was performed using the Axion Vision program (Carl Zeiss) to measure acinar nuclear and cellular volumes. RESULTS: the nuclear and cellular volumes of the lacrimal glands in the MET1-(152.2±8.7; 6.3±1.6 µm³) and MET2-(278.3±7.9; 27.5±0.9 µm³) treated groups were lower than those in CTR1 (204.2±7.4; 21.9±1.3 µm³) and CTR2 (329.4±2.2; 35.5±2.0 µm³), respectively. There was a significant hormonal level reduction in the animals that received metoclopramide compared to controls (CTR1: estradiol = 156.6±42.2 pg/ml; progesterone = 39.4±5.1 ng/ml; MET1: estradiol = 108.0±33.1 pg/ml; progesterone = 28.0±6.4 ng/ml; CTR2: estradiol = 354.0±56.0 pg/ml; progesterone = 251.0±56.0 ng/ml; MET2: estradiol = 293.0±43.0 pg/ml, progesterone = 184.0±33.0 ng/ml). CONCLUSION: metoclopramide-induced hyperprolactinemia produced morphological signs of reduction of cellular activity in lacrimal glands during the proestrus phase and pregnancy. It is hypothesized that this effect might be related to the hyperprolactinemia-induced decrease in the hormonal production of estrogen and progesterone.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(9):529-533
DOI 10.1590/S0100-72032005000900005
PURPOSE: to study the histological modifications that occur in the endometrium of women before and six months after tubal ligation (TL) and to correlate these findings with progesterone (P4) levels. METHODS: the study was conducted on 16 women with normal menstrual cycles who were evaluated before and in the sixth cycle after TL. P4 levels were determined from the 8th day at 2-day intervals until ovulation and on the 8th, 10th and 12th day after ovulation or on the 24th day of the cycle. An endometrial biopsy was obtained between the 10th and 12th day after ovulation or on the 24th day of the cycle and a correlation with P4 was determined. Data were analyzed statistically by the nonparametric McNemar test for the evaluation of hormonal determination and by the exact Fisher test for the histological evaluation of the endometrium, with the level of significance set at p<0.05. RESULTS: mean age was 34.1±1.3 years. The intermenstrual interval was 27.1±2.6 days and the duration of bleeding was 3 to 5 days, with no difference between the studied periods. Before TL, 8/16 (50.0%) of the cases had a secretory endometrium according to the cycle, 3/16 (18.8%) had a secretory endometrium not according to the cycle and 3/16 (18.8%) had a dysfunctional endometrium, suggesting a defect in the luteal phase in 6/16 (37.5%). After TL, 7/16 (43.8%) had a secretory endometrium according to the cycle, 3/16 (18.8%) a secretory endometrium not according to the cycle and 4/16 (25.0%) had a dysfunctional endometrium, suggesting a defect in the luteal phase in 7/16 (43.8%). In 2/16 (12.5%) of the cases before TL and in 2/16 (12.5%) other cases after TL it was not possible to perform histological evaluation due to insufficient material or unspecfiic endometritis. In the luteal phase after TL, mean P4 levels were significantly lower on days +8, +10 and +12 than before TL, being 15.1, 18.0 and 20.7 ng/ml, respectively, before TL and 10.6, 8.0 and 5.4 ng/ml after TL (p<0.05). Before TL, 5/8 (62.5%) of the cases with a secretory endometrium according to the cycle had P4 >10 ng/ml and 3/8 (37.5%) had P4 <10 ng/ml. After TL, when the endometrium was secretory according to the cycle, P4 was >10 ng/ml in 4/7 (57.1%) and <10 ng/ml in 3/7 (42.9%). These differences were nonsignificant (p>0.05). CONCLUSION: six months after TL, the intermenstrual interval and the duration of bleeding were unchanged. P4 levels decreased during the luteal phase although this did not interfere in the endometrial response.