Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(6):295-302
DOI 10.1590/S0100-72032011000600006
PURPOSE: To evaluate bone mineral density (BMD) and their risk factors associated with postmenopausal osteoporosis. METHODS: A cross-sectional clinical study was performed on 431 women (aged 40 - 75 years). Inclusion criteria: amenorrhea >12 months and age >45 years or, bilateral oophorectomy >40 years with BMD values (T-score of lumbar spine/femur neck) by DXA of the last 12 months. Risk factors evaluated: age, age and time of menopause, smoking, physical activity (30 min/5 times/week), rheumatoid arthritis (RA), use of corticotherapy and hormone therapy (HT), previous fracture, maternal hip fracture and body mass index (BMI=weight/height²). The χ2 test and the logistic regression method (Odds Ratio - OR) were used to determine osteoporosis risk. RESULTS: According to WHO criteria, 106 (24.6%) women showed osteoporosis (T-score <-2.5 DP), 188 (43.6%) osteopenia (-1.0/-2.4 DP), and 137 (31.8%) were normal (>-1.0 DP). Osteoporosis was detected in 12% of women aged 40 - 49 years, in 21.8% of women aged 50 - 59 years and in 45.7% of women aged >60 years (p<0.001). Osteoporosis occurred in 11.8% of women with a menopause period <5 years, in 29.4% with a menopause period from 6 to 10 years, and in 41% of women with a menopause period >10 years (p<0.001). Of the women with early menopause, 80% showed osteopenia/osteoporosis (p=0.03), and of those with BMI <20 kg/m², 50% were osteoporotic (p<0.001). The risk for osteoporosis detection increased with age (OR=1.1; CI95%=1.0-1.1), time of menopause (OR=1.1; CI95%=1.0-1.1), smoking (OR=1.9; CI95%=1.2-3.2), RA (OR=3.6; CI95%=1.3-9.6) and maternal fracture history (OR=2.1; CI95%=1.1-3.0) (p<0.05). In contrast, HT use (OR=0.3; 95%CI=0.2-0.6) and high BMI (OR=0.9; 95%CI=0.8-0.9) reduced the risk (p<0.05). CONCLUSION: In postmenopausal women, age, time of menopause, smoking and maternal history of fracture were clinical indicators of risk for osteoporosis, whereas HT use and high BMI proved to be protective factors.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(6):288-294
DOI 10.1590/S0100-72032011000600005
PURPOSE: to evaluate the performance of the combined first trimester screening for chromosomal abnormalities in a group of the Brazilian population. METHODS: a retrospective study including pregnant women with single fetuses referred to a fetal medicine center to perform the first trimester screening that combines maternal age, nuchal translucency measurement and two maternal serum biochemical markers: free B-hCG and PAPP-A. To evaluate the performance of the test, the detection rate, specificity, negative and positive predicted values and false-positive rates were calculated, considering as high risk the cut-off value above 1 in 300. RESULTS: we studied 456 patients submitted to the test. Advanced maternal age above 35 years was observed in 36.2% of cases. The incidence of chromosomal abnormalities in the study population was 2.2%. Twenty-one patients (4.6%) presented a high risk (above 1:300) by the combined test. Using this cut-off level, the detection rate of the test was 70% for all chromosomal abnormalities and 83.3% for trisomy 21, for a false-positive rate of 3.1%. CONCLUSIONS: the combined first trimester screening was effective to detect chromosomal abnormalities, mainly for trisomy 21, with low false-positive rates. The combined test contributed to decreasing the indication of an invasive test if we compare to maternal age alone as a risk factor.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(6):276-280
DOI 10.1590/S0100-72032011000600003
PURPOSE: To evaluate the effectiveness of misoprostol administered vaginally for uterine evacuation in interrupted early pregnancies and the time between the administration and emptying correlated with gestational age. METHODS: Clinical trial with 41 patients with pregnancies interrupted between the 7th and the 12th gestational weeks. The mean age was 27.3 (±6.1) years. Mean parity was 2.2 (±1.2) deliveries. The average number of previous abortions was 0.2 (± 0.5). Misoprostol was administered vaginally in a single 800 µg dose and transvaginal ultrasound was performed after 24 hours. Abortion was considered complete when the anteroposterior diameter of the endometrial cavity measured <15 mm. Patients whose diameter remained was larger than 15 mm underwent uterine curettage. Two groups (<8 and >8 weeks of gestational age) were compared using the binomial test and Student's t test regarding outcome: frequency of complete abortion and the interval between administration of misoprostol and abortion (in minutes). The level of significance was 5%. RESULTS: The mean gestational age at diagnosis was 8.5 weeks (SD=1.5). The intervals between administration of misoprostol and uterine contractions and between the administration and abortion were 322.5±97.0 minutes and 772.5±201.0 minutes, respectively. There was complete abortion in 80.3%. The success rate was 96.2% for the first group and 53.3% for the second (p<0.01). We observed a statistically significant difference in time between administration and uterine evacuation (676.2±178.9 vs. 939.5±105.7 minutes, p<0.01). The side effects observed were hyperthermia (12.1%), nausea (7.3%), diarrhea or breast pain (2.4%). No case of genital infection was observed. CONCLUSIONS: The use of vaginal misoprostol is a safe and effective alternative to curettage for interrupted early pregnancies, being better in pregnancies up to the 8th week. The time interval until emptying was lower in pregnancies that were interrupted earlier.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(5):246-251
DOI 10.1590/S0100-72032011000500007
PURPOSE: to evaluate the prevalence of cytogenetic alterations and chromosomic polymorphism in couples with a subfertility phenotype in a Brazilian population. METHODS: karyotype analysis through G and C banding of 1,236 individuals who presented the subfertility phenotype, from two different centers (public and private) were included in the study. These patients were classified in two sub-groups: one with two or more gestational consecutive losses or not and the o with, at least, one gestacional loss or absence of conception. Karyotype results were evaluated in different groups and frequencies were calculated. Statistical analyses were carried out through Fisher's exact test and Odds Ratio analysis. RESULTS: approximately 25% of the cases presented abnormal karyotype results, including numerical and structural alterations and also polymorphic variants. In both centers, the prevalence of polymorphic variants was 8.9 and 3.8%, respectively. CONCLUSIONS: there was no significant difference between the prevalence of polymorphic variants and other abnormalities in individuals with or without previous history of reproductive loss. The results of the present study reinforce the need of adequate disclosure of complete cytogenetic information in the karyotype results, with specific attention in relation to the polymorphic variants.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(5):238-245
DOI 10.1590/S0100-72032011000500006
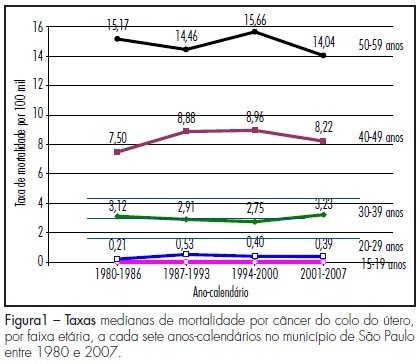
PURPOSE: to compare the coverage of conventional Papanicolaou cytology in women aged 15 to 59 years between two home surveys, related to some personal attributes and to the tendency to die from cervical cancer. METHODS: we analyzed data collected in two home surveys, with complex sampling, in the city of São Paulo, Brazil, over the years from 1987 to 2001 and 2002. The self-reported answers of 968 women in the first inquiry and of 1,125 women in the second inquiry were compared regarding the reply to the question about the execution of the Papanicolaou test "sometimes in a lifetime" in relation to age distribution, black skin, marital status, years of education and tendency to die because cervical cancer during the period from 1980 to 2007. The Fisher exact test was used to compare the sample regarding each item, with the level of significance set at p value >5%. RESULTS: from the first to the second inquiry there was a 24% increase in the execution of conventional Papanicolaou cytology (from 68.8% to 85%). The greatest variations in the increased coverage related to the personal attributes of the women were detected in black skin color, among single women and among women of lower schooling. Regarding the tendency to mortality rates due to cervical cancer, no clear ascending or declining tendency was observed along the 28 years studied (1980 to 2007). CONCLUSION: there was an increase in access to the cytological Papanicolaou test among the most vulnerable women. Since 2001 and 2002, the 85% coverage already reached WHO recommendation, although without a clear trend of decline in mortality due to cervical cancer in the following years, indicating that screening is only part of an effective and organized program for the control of cervical cancer, whose model must guarantee full women's health care.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(5):219-224
DOI 10.1590/S0100-72032011000500003
To compare the sexual function of healthy adult pregnant women with that of gestational diabetes patients (GDM) in the third trimester. METHODS: This cross-sectional study enrolled two groups of women managed antenatal care clinics. Inclusion criteria were: maternal age .20 years, gestational age at least 28 weeks, being in a heterosexual relationship with the same partner for at least 6 months, and being able to read. We excluded women with a medical recommendation for sexual abstinence due to clinical or obstetric disorders; hypertension controlled through medications; pregnancy resulting from rape; absent or sexually unavailable partner in the last month; hospital admission in the last month; use of vaginal creams in the last 30 days; multiple pregnancy, regular use of alcohol or illicit drugs or use of medications that can interfere with sexual function. Eighty-seven patients fulfilled the selection criteria and were included in the study. The Sexual Quotient . Feminine Version (QS-F) questionnaire was used to assess sexual function. Student's t and X² tests were used to compare differences between groups and p<0.05 was considered significant. RESULTS: The mean gestational age of the participants was 34 weeks. There were no significant differences in the mean QS-F scores between groups (62.5 healthy vs 62.8 GDM women, p=0.9). Approximately half the participants (47 and 47.5% of the healthy and GDM women, respectively, p=0.9) had total scores up to 60, indicative of dysfunction in one of the assessed domains (desire, sexual satisfaction, arousal, orgasm, dyspareunia and vaginismus). CONCLUSIONS: The prevalence of sexual dysfunction was high among women in the third trimester of pregnancy and did not differ significantly between healthy women and women with GDM.