-
Review Article10-23-2020
Characterization of Placental Infection by Zika Virus in Humans: A Review of the Literature
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(9):577-585
Abstract
Review ArticleCharacterization of Placental Infection by Zika Virus in Humans: A Review of the Literature
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(9):577-585
Views214See moreAbstract
Objective
The aim of the current review is to present a systematic evaluation of reported human placental findings in cases of zika virus (ZIKV) infection.
Data
sources We reviewed the EMBASE, PUBMED, and SCIELO databases until June 2019, without language restrictions. Selection of studies The search terms placenta AND zika virus were used. The inclusion criteria of the studies were studies that reported placental findings in humans. Experimental studies, reviews, notes or editorials were excluded. A total of 436 studies were retrieved; after duplicate exclusion, 243 articles had their titles screened, and 128 had their abstract read; of those, 32 were included in the final analysis (18 case reports, 10 case series, and 4 cohorts)
Data collection
We collected data concerning the author, year of publication, study design, number of participants, number of placental samples, onset of symptoms, perinatal outcomes, and main findings on histological analysis.
Data synthesis
The placental pathologic findings were described as mild and nonspecific, similar to those of other placental infections, including chronic placentitis, chronic villitis, increased Hofbauer cells, irregular fibrin deposits, increased mononuclear cells in the villus stroma, villous immaturity, edema, hypervascularization, stromal fibrosis, calcification, and focal necrosis of syncytiotrophoblasts.
Conclusion
Zika infection presents unspecific placental findings, similar to other infections in the toxoplasmosis, other agents, rubella, cytomegalovirus, and herpes (TORCH)group. Characterizing and standardizing placental findings after zika virus infection is key to understanding the mechanisms of congenital diseases.
-
Systematic Review05-01-2017
Zika Virus Infection in Pregnant Women and Microcephaly
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):235-248
Abstract
Systematic ReviewZika Virus Infection in Pregnant Women and Microcephaly
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):235-248
Views389Abstract
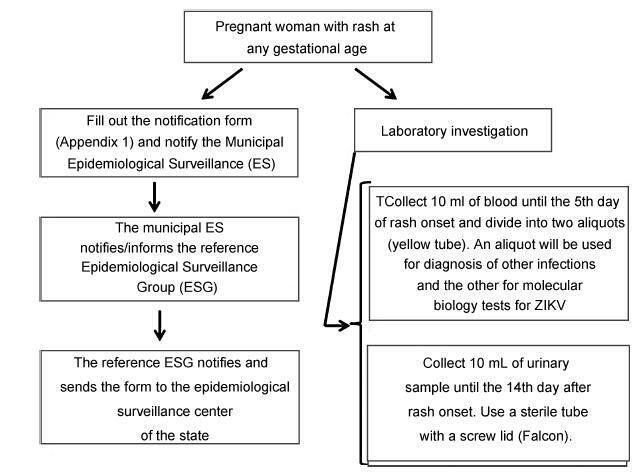
From the discovery of the Zika virus (ZIKV) in 1947 in Uganda (Africa), until its arrival in South America, it was not known that it would affect human reproductive life so severely. Today, damagetothe central nervous system is known to be multiple, and microcephaly is considered the tip of the iceberg. Microcephaly actually represents the epilogue of this infection’s devastating process on the central nervous system of embryos and fetuses. As a result of central nervous system aggression by the ZIKV, this infection brings the possibility of arthrogryposis, dysphagia, deafness and visual impairment. All of these changes of varying severity directly or indirectly compromise the future life of these children, and are already considered a congenital syndrome linked to the ZIKV. Diagnosis is one of the main difficulties in the approach of this infection. Considering the clinical part, it has manifestations common to infections by the dengue virus and the chikungunya fever, varying only in subjective intensities. The most frequent clinical variables are rash, febrile state, non-purulent conjunctivitis and arthralgia, among others. In terms of laboratory resources, there are also limitations to the subsidiary diagnosis. Molecular biology tests are based on polymerase chain reaction (PCR)with reverse transcriptase (RT) action, since the ZIKV is a ribonucleic acid (RNA) virus. The RT-PCR shows serum or plasma positivity for a short period of time, no more than five days after the onset of the signs and symptoms. The ZIKVurine test is positive for a longer period, up to 14 days. There are still no reliable techniques for the serological diagnosis of this infection. If there are no complications (meningoencephalitis or Guillain-Barré syndrome), further examination is unnecessary to assess systemic impairment. However, evidence is needed to rule out other infections that also cause rashes, such as dengue, chikungunya, syphilis, toxoplasmosis, cytomegalovirus, rubella, and herpes. There is no specific antiviral therapy against ZIKV, and the therapeutic approach to infected pregnant women is limited to the use of antipyretics and analgesics. Anti-inflammatory drugs should be avoided until the diagnosis of dengue is discarded. There is no need to modify the schedule of prenatal visits for pregnant women infected by ZIKV, but it is necessary to guarantee three ultrasound examinations during pregnancy for low-risk pregnancies, and monthly for pregnant women with confirmed ZIKV infection. Vaginal delivery and natural breastfeeding are advised.
Key-words arbovirus infectionsblindness/ etiologydeafness/ etiologymicrocephaly/ ultrasonographyPregnancy complicationsReal-time polymerase chain reactionZika virusSee more