-
Case Report
Vulvar Hemangioma: Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(6):369-371
06-01-2018
Summary
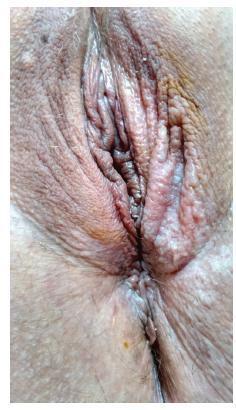
Case ReportVulvar Hemangioma: Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(6):369-371
06-01-2018Views134See moreAbstract
Hemangioma is a benign neoplasm that may affect the vulva, and it can cause functional or emotional disability. This article reports the case of a 52-year-old female patient with a history of a genital ulcer for the past 3 years and who had undergone various treatments with creams and ointments. The patient was biopsied and diagnosed with vulvar hemangioma and was subsequently submitted to surgical excision of the lesion. We emphasize the importance of following the steps of the differential diagnosis and proceeding with a surgical approach only if necessary.

-
Case Report
Extramammary Paget Disease of the Vulva – Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):524-528
10-01-2016
Summary
Case ReportExtramammary Paget Disease of the Vulva – Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):524-528
10-01-2016Views85See moreAbstract
Extramammary Paget disease (EPD) is a rare malign neoplasm that may affect the vulva and has manifestations common to benign diseases such as itching, pain and eczema. This leads to delay in diagnosis and consequent worse prognosis. The definitive diagnosis is obtained by biopsy of the vulva, which shows Paget cells. The treatment of choice is wide excision with margins, which leads to sequelae, functional and aesthetic. Recurrence is common. This article reports the case of a 48-year-old female patient with history of vulvar itching for the past 2 years, who had been submitted to various treatments for benign pathologies. The patient was biopsied and was diagnosed with extensive EPD, being submitted to vulvectomy. This article aims to draw attention to the need for biopsy of pruritic vulvar lesions that do not respond to usual treatment.
-
Article
Aggressive angiomyxoma of the vagina: a case report
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(12):575-582
02-03-2013
Summary
ArticleAggressive angiomyxoma of the vagina: a case report
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(12):575-582
02-03-2013DOI 10.1590/S0100-72032013001200008
Views112See moreAggressive angiomyxoma is a rare, slow-growing soft tissue tumor that usually arises in the pelvis and perineal regions of women in reproductive age, with a marked tendency to local recurrence. Because of its rarity, it is often initially misdiagnosed. Surgical resection is the main treatment modality of aggressive angiomyxoma. We describe a case of a vaginal aggressive angiomyxoma in a 47-year-old woman in which the diagnosis was only made after histological examination. The etiology, presentation, diagnosis and management of this rare tumor are outlined. Angiomyxoma of vulva and vagina refers to a rare disease. Pre-operative diagnosis is difficult due to rarity and absence of diagnostic features, but it should be considered in every mass in genital, perianal and pelvic region in a woman in the reproductive age. Thus, these cases should have complete radiological workup before excision, as pre-diagnosis can change the treatment modality and patient prognosis'.
-
Artigo de Revisão
Vulvar intraepithelial neoplasia: a current problem
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(8):420-426
10-16-2008
Summary
Artigo de RevisãoVulvar intraepithelial neoplasia: a current problem
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(8):420-426
10-16-2008DOI 10.1590/S0100-72032008000800008
Views42See moreVulvar intraepithelial neoplasia (VIN) is a pathological denomination coined by the International Society for Study of Vulvo-vaginal Diseases (ISSVD) and adopted by the International Society of Gynaecological Pathology (ISGYP) and by the World Health Organization. VIN is a heterogeneous pathological entity with a usual type (warty, basaloid and mixed) and a differentiated type. The incidence of the disease is increasing, especially in young women. The high-risk human papilomavirus (HR-HPV) infection, human immunodeficiency virus (HIV) infection, smoking, cervical, vaginal and rectal intraepithelial neoplasia are considered to be high risk factors for development of VIN. There are no specific symptoms or vulvar macroscopic aspects of VIN. However, a clinical lesion is always present. Liberal vulvar biopsies under colposcopy guidance should be done. Patients with diagnosis of VIN harbor an increased risk for vulvar invasive cancer. Surgical excision and laser CO2 vaporization are the most popular therapeutic modalities for VIN treatment, both with high rates of recurrence. A close follow-up of the patients is advised. Topical imiquimod seems to be a promising treatment option. Probably, prophylactic vaccination against HR-HPV will be an important tool for VIN prevention.
-
Artigos Originais
Vulval intraepithelial lesions in HIV-infected patients
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):407-414
11-22-2005
Summary
Artigos OriginaisVulval intraepithelial lesions in HIV-infected patients
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):407-414
11-22-2005DOI 10.1590/S0100-72032005000700007
Views109See morePURPOSE: to evaluate the prevalence of vulval squamous intraepithelial lesions and associated factors in HIV-infected patients attended at the public health services of Rio de Janeiro city. METHOD: a total of 374 HIV-infected patients were attended at public services in Rio de Janeiro city and submitted to gynecological examination, Pap smear and colposcopic examination of the cervix and vulva. The association of vulval intraepithelial lesion was analyzed according to the results of clinical (age and cervical lesions), laboratorial (CD4 count) and behavioral (number of partners and smoking habit) variables. The study (independent) variables were the epidemiological data, the immunologic status and the results of gynecological propaedeutic. Thus, age, the smoking habit, number of sexual partners, count of T CD4 lymphocites, and cervical intraepithelial lesion were selected. In the beginning, a bivariate analysis was performed, aiming at assessing the association between the presence of vulval intraepithelial lesion (ultimate variable) and the independent variables (age, smoking habits, number of sexual partners, cytology, colposcopy and CD4 count). Thereafter, the results with statistical significance (p<0.05) were submitted to a multiple logistic regression, and the probability ratio with the respective 95% confidence interval was established. RESULTS: the prevalence of vulval intraepithelial lesions was 40%. In the multivariate analysis CD4 count below 500 cells/mm³ OR=2.69 [IC 95%: 1.61-4.52], abnormal colposcopy OR=1.64 [IC 95%: 1.01-2.67] and age under 26 OR=1.98 [IC 95%: 1.18-3.30] were significant. In the vulval and cervical simultaneous lesion subgroup, age under 26 OR=3.30 [IC 95%: 1.65-6.59] and CD4 count below 500 cells/mm³ OR=4.15 [IC 95%: 1.92-8.96], were significant on analysis. CONCLUSIONS: the prevalence of vulval squamous intraepithelial lesions in HIV-infected patients is high. Immunodeficiency, presence of cervical intraepithelial lesions and age under 26 were associated with the presence of vulval intraepithelial lesions.



