Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(3):155-161
DOI 10.1590/S0100-72032003000300003
PURPOSE: the morbidity in HIV-positive patients due to puerperal fever was studied and correlated to the method and duration of labor, the duration of premature rupture of the membranes, CD4+ cell count and the viral load (VL) at peridelivery. METHODS: a total of 207 HIV-positive women with prenatal examinations and deliveries between May 1997 and December 2001 were enrolled. Of these, 32 had natural childbirth and 175 had a cesarean section. Of the total of enrolled patients, 62.8% were submitted to elective cesarean section. The average age of the group was 27.4 years, and 25.6% were nulliparous and 26% were primiparous. At the moment of the delivery the average gestational age was 37.8 weeks. At the end of pregnancy the average of the CD4+ cell count was approximately 481 cells/mm³ and the viral load 49,100 copies/mL. RESULTS: puerperal morbidity occurred in 34 patients, with 33 after cesarean section and one after natural childbirth. The most usual intercurrent post-cesarean infection was that of the surgical wound (13% of the infection cases). Analyzed factors, such as delivery duration, duration of rupture of the membranes, number of CD4+ cells or the viral load at peridelivery, did not interfere in puerperal morbidity. CONCLUSIONS: puerperal morbidity was 16.8% and occurred more frequently after cesarean sections (18.9%) than after vaginal deliveries (3.1%). The other factors did not present a significant effect on puerperal morbidity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(5):317-321
DOI 10.1590/S0100-72032003000500003
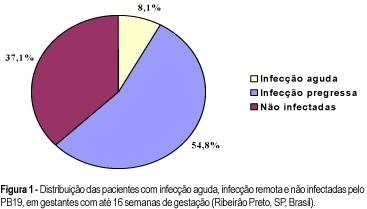
PURPOSE: to evaluate the rate of seropositivity for parvovirus B19 (PB19) among pregnant women and the rate of seroconversion against this infection during pregnancy. METHODS: prospective study carried out in the Hospital of the Medical School of Ribeirão Preto, University of São Paulo. In the first stage of the present study, we evaluated 245 pregnant women with gestational age less than 16 weeks to determine the seroprevalence of PB19 infection by ELISA. According to the serological results we determined if the PB19 infection was an acute infection (IgM positive and IgG negative or positive), or a former infection (IgM negative and IgG positive). In the second stage of this study, 73 previously seronegative pregnant women were tested again when they came to the hospital for delivery (IgM and IgG), to detect the seroconversion rate during pregnancy. RESULTS: the seroprevalence of the PB19 infection until 16 weeks of gestation was 62.9% (95% IC: 56.8-68.9), divided into acute infection (8.1%), or former infection (54.8%). Of the 73 patients, seronegative in the first stage of this investigation, seven (9.6%) showed seroconversion during pregnancy (95% IC: 2.8-16.3), two (2.7%) showed acute serological infection and five (6.9%) presented markers of past infection. The final seroprevalence of PB19 infection during pregnancy was 72.5%. CONCLUSIONS: considering that only the acute PB19 infection is associated with risk for vertical transmission, the high seroprevalence of this infection observed in this study would be protecting these fetuses against this form of infection. Despite the relatively high rate of seroconversion against PB19 infection during the pregnancy period, we did not observe any symptomatic neonate in this group.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(5):323-328
DOI 10.1590/S0100-72032003000500004
PURPOSE: to determine whether an elective cesarean section at the 38th week of gestation for HIV positive patients, in spite of decreasing vertical transmission, increases the risk of maternal death. METHODS: fifty-eight HIV-infected patients were studied and submitted to the complete ACTG 076 protocol (oral administration of zidovudine in the prenatal period associated with the intravenous form at delivery) followed by an elective cesarean section at the 38th week of gestation. The control group consisted of 226 noninfected women (the first four patients submitted to an elective cesarian section after each cesarian section in infected patient). The analyzed variables were: uterine atonia, puerperal fever, abdominal wall infection, urinary infection, endometritis, average blood loss, surgery time, and hospitalization time. Data were analyzed by the c² test (the Fisher test was used when there were less than 5 cases). The relative risk was calculated with the Epi-Info 6.0 program. RESULTS: results show that the elective cesarean section performed on HIV-positive patients, when compared to the control group, did not present a higher incidence of uterine atonia, puerperal fever, abdominal wall infection, urinary infection or endometritis. However, a greater average blood loss (2.26 relative risk) was recorded as well as an extended surgery time (3.32 relative risk). The HIV-infected patients remained less time in hospital than the noninfected control group (0.33 relative risk). CONCLUSION: we conclude that there was no increase in maternal morbidity after cesarean section as a means of interrupting gestation in the HIV-infected patients.