Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(6):286-292
DOI 10.1590/S0100-72032010000600006
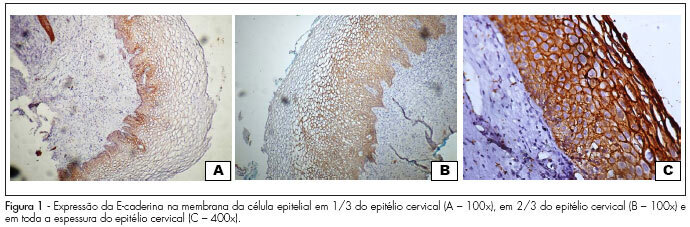
PURPOSE: to evaluate the expression of E-cadherin in cervical lesions of patients suffering from HIV infection. METHODS: we conducted a study with 77 patients with cervical HPV infection, 40 of them were HIV seropositive and 37 HIV seronegative who underwent colposcopy and a biopsy of the cervix. The material obtained by biopsy of the cervix was sent for histopathologic and immunohistochemical study. Sections were obtained and mounted on silanized slides and examined by an observer who was blind to patient serology. E-cadherin antibody, clone NHC-38 diluted 1:400 (DAKO) and the Novolink polymer system (Novocastra) were used. The expression of E-cadherin was determined on the epithelial cell membrane based on the extent of the stained area. The χ2 test with Yates correction or the Fisher's Exact test was used for comparison of the proportion in univariate analysis. All the variables with p<0.25 were included in the logistic regression model, called initial model. The analyses were carried out using the SPSS software, with the level of significance set at 5%. RESULTS: the expression of E-cadherin was observed in up to the internal 1/3 of the epithelium in 59.3% of cases and in up to 2/3 of the epithelium in 11.1% of cases, but in 29.6% of cases the expression was identified throughout the thickness of the epithelium in HIV-seronegative patients. In contrast, in HIV-seropositive patients, 45.9% showed expression up to 1/3 of the epithelium, 13.5% showed expression in up to 2/3 of the epithelium, and 40.5% showed expression throughout the thickness of the epithelium. E-cadherin expression did not differ between groups (p=0.5). However, the multivariate analysis identified a significant association between high-grade cervical injury and E-cadherin expression in 2/3 and 3/3 of the epithelium (p=0.001; χ2=36.9). CONCLUSIONS: the expression of E-cadherin in the epithelial cell membrane is not associated with infection by the human immunodeficiency virus, but with the degree of intraepithelial cervical injury.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(9):536-544
DOI 10.1590/S0100-72032006000900006
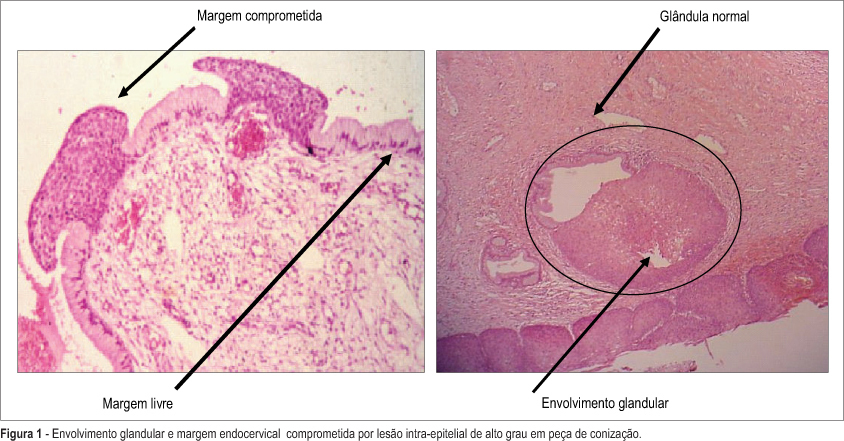
PURPOSE: to evaluate risk factors associated with cervical intraepithelial lesion recurrence after LEEP conization. METHODS: nested case-control study in a cohort of 201 patients with cervical intraepithelial lesion, that were submitted to LEEP conization. Average follow-up of these patients was 2 years. Ninety-four HIV-infected women and 107 non-infected were enrolled. Cervical conization was achieved by the Loop Electrosurgical Excision Procedure (LEEP). Evaluated surgical biopsy histopathological characteristics were lesion grade, lesion borders and glandular involvement. After surgery all patients were submitted to a colposcopy and cytological evaluation every six months. Recurrent lesions were defined it confirmed by biopsy after surgery. Cases were patients with and controls patients without recurrence. chi2 test and multivariable analysis by logistic regression were used for group comparisons. Kaplan Meier's method was performed for the survival analyses (log-rank test). RESULTS: 40 patients had lesion recurrence. Initially, significant variables were: partner number, HIV-infection, lesion borders and glandular involvement. The most frequent recurrence occurred when there were simultaneous association between positive margins and glandular involvement as indicator for recurrence risk. After logistic regression analysis the main factors associated with lesion recurrence were: glandular involvement (OR-9.1; 95% CI:13.0- 27.5); HIV-infection (OR-4.6; 95% IC:1.1-6.3); compromised margins (OR-2.6; 95% IC:1.9-11.2). CONCLUSIONS: risk factors associated with cervical intraepitelial lesion recurrence were HIV-infection, glandular involvement and compromised margins.