Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):427-435
We performed a systematic review to assess the effectiveness and safety of Tribulus terrestris to treat female sexual dysfunction (FSD).
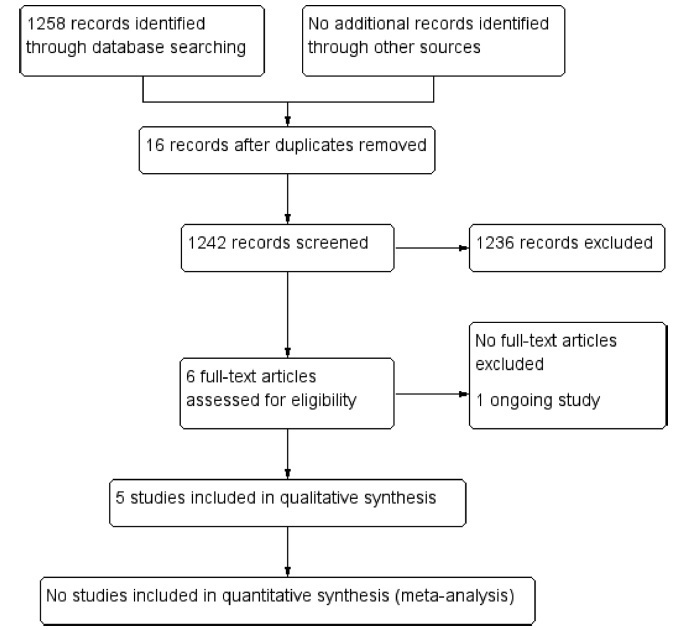
We performed unrestricted electronic searches in the MEDLINE, CENTRAL, EMBASE, LILACS, CINAHL, PsycINFO,WHO-ICTR, Clinicaltrials.gov and OpenGrey databases. Selection of studies We included any randomized controlled trials (RCTs) that compared T. terrestris versus inactive/active interventions. After the selection process, conducted by two reviewers, 5 RCTs (n = 279 participants) were included.
Data extraction was performed by two reviewers with a preestablished data collection formulary.
Due to lack of data and clinical heterogeneity, we could not perform meta-analyses. The risk of bias was assessed by the Cochrane Risk of Bias (RoB) tool, and the certainty of evidence was assessed with Grading of Recommendations, Assessment, Development and Evaluations (GRADE).
After 1 to 3 months of treatment, premenopausal and postmenopausal women randomized to T. terrestris had a significant increase in sexual function scores. Three months of treatment with T. terrestris showed a significant increase in the serum testosterone levels of premenopausal women. There was no report of serious adverse events, and none of the studies assessed health-related quality of life. The certainty of the evidence was very low, whichmeans that we have very little confidence in the effect estimates, and future studies are likely to change these estimates.
MoreRCTs are needed to supportor refute the use of T. terrestris. The decision to use this intervention should be shared with the patients, and the uncertainties around its effects should be discussed in the clinical decision-making process. Number of Protocol registration in PROSPERO database: CRD42019121130
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(3):140-146
The aim of this study was to study the effects of Tribulus terrestris on sexual function in menopausal women.
This was a prospective, randomized, double-blind, placebo-controlled clinical trial that included 60 postmenopausal women with sexual dysfunction. The women were divided into two groups, placebo group and Tribulus group, and evaluated by using the Sexual Quotient-female version (SQ-F) and Female Intervention Efficacy Index (FIEI) questionnaires.
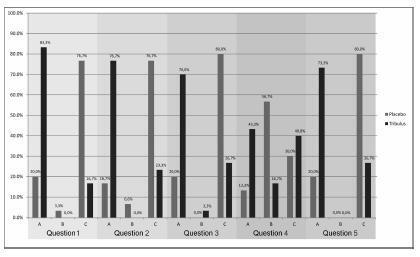
There was no significant difference between the groups in age, age at menopause, civil status, race, and religion. In the evaluation with the SQ-F questionnaire, there were significant differences between the placebo (7.6±3.2) and Tribulus (10.2±3.2) groups in the domains of desire and sexual interest (p d" 0.001), foreplay (3.3±1.5 versus 4.2±1.0) (p d" 0.01), arousal and harmonious interaction with the partner (5.7±2.1 versus 7.2±2.6) (p d" 0.01), and comfort in sexual intercourse (6.5±2.4 versus 8.0±1.9) (p d" 0.01). There was no significant difference between the placebo and Tribulus groups in the domains of orgasm and sexual satisfaction (p = 0.28). In the FIEI questionnaire, there was a significant improvement (p < 0.001) in the domains of vaginal lubrication during coitus and/or foreplay (20 versus 83.3%), sensation in the genitalia during sexual intercourse or other stimuli (16.7 versus 76.7%), sensation in the genital region (20 versus 70%), sexual intercourse and/or other sexual stimulations (13.3 versus 43.3%), and the ability to reach orgasm (20% versus 73.3%). There was no significant difference in adverse effects between the two groups.
After 90 days of treatment, at the doses used, we found Tribulus terrestris to be effective in treating sexual problems among menopausal women.