Summary
Revista Brasileira de Ginecologia e Obstetrícia. 01-23-2023;44(11):1014-1020
Cervical pregnancy is challenging for the medical community, as it is potentially fatal. The treatment can be medical or surgical; however, there are no protocols that establish the best option for each case. The objective of the present study was to describe the cases of cervical pregnancy admitted to a tertiary university hospital over a period of 18 years.
A retrospective study based on a review of the medical records of all cervical pregnancies admitted to the Women's Hospital at Universidade Estadual de Campinas, Southeastern Brazil, from 2000 to 2018.
We identified 13 cases of cervical pregnancy out of a total of 673 ectopic pregnancies; only 1 case was initially treated with surgery because of hemodynamic instability. Of the 12 cases treated conservatively, 7 were treated with single-dose intramuscular methotrexate, 1, with intravenous and intramuscular methotrexate, 1, with intravenous methotrexate, 1, with 2 doses of intramuscular methotrexate, and 2, with intra-amniotic methotrexate. Of these cases, one had a therapeutic failure that required a hysterectomy. Two women received blood transfusions. Four women required cervical tamponade with a Foley catheter balloon for hemostasis. There was no fatal outcome.
Cervical pregnancy is a rare and challenging condition from diagnosis to treatment. Conservative treatment was the primary method of therapy used, with satisfactory results. In cases of increased bleeding, cervical curettage was the initial treatment, and it was associated with the use of a cervical balloon for hemostasis.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 01-11-2021;42(12):800-804
In recent years, there has been an increase in the incidence of ectopic pregnancies; therefore, it is important for tertiary centers to report their approaches and outcomes to expand and improve treatment modalities. The aim of the present study was to evaluate the general characteristics, treatment and outcomes of cases diagnosed with ectopic pregnancy.
In total, 432 patients treated for ectopic pregnancy between February 2016 and June 2019 were retrospectively evaluated.
Overall, 370 patients had tubal pregnancy, 32 had cesarean scar pregnancy, 18 had pregnancy of unknown location, 6 had cervical pregnancy, and 6 had interstitial pregnancy. The most important risk factors were advanced age (> 35 years; prevalence: 31.2%) and smoking (prevalence: 27.1%). Thirty patients who did not have any symptoms of rupture and whose human chorionic gonadotropin (β-hCG) levels were ≤ 200 mIU/ml were followed-up with expectant management, while 316 patients whose β-hCG levels were between 1,500 mIU/ml and 5,000 mIU/ml did not have an intrauterine gestational sac on the transvaginal or abdominal ultrasound, did not demonstrate findings of rupture, and were treated with a systemic multi-dose methotrexate treatment protocol. In total, 24 patients who did not respond to the medical treatment, 20 patients whose β-hCG levels were > 5,000 mIU/ml, 16 patients who had shown symptoms of rupture at the initial presentation, and 6 patients diagnosed with interstitial pregnancy underwent surgery. Patients with cervical and scar pregnancies underwent ultrasound-guided curettage, and no additional treatment was needed.
The fertility status of the patients, the clinical and laboratory findings, and the levels of β-hCG are the factors that must be considered in planning the appropriate treatment.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 10-23-2020;42(9):562-568
The present comprehensive review aims to show the full extent of what is known to date and provide a more thorough view on the effects of SARS-CoV2 in pregnancy.
Between March 29 and May, 2020, the words COVID-19, SARS-CoV2, COVID- 19 and pregnancy, SARS-CoV2 and pregnancy, and SARS and pregnancy were searched in the PubMed and Google Scholar databases; the guidelines from well-known societies and institutions (Royal College of Obstetricians and Gynaecologists [RCOG], American College of Obstetricians and Gynecologists [ACOG], International Society of Ultrasound in Obstetrics & Gynecology [ISUOG], Centers for Disease Control and Prevention [CDC], International Federation of Gynecology and Obstetrics [FIGO]) were also included.
The COVID-19 outbreak resulted in a pandemic with > 3.3 million cases and 230 thousand deaths until May 2nd. It is caused by the SARS-CoV2 virus and may lead to severe pulmonary infection and multi-organ failure. Past experiences show that unique characteristics in pregnancy make pregnant women more susceptible to complications from viral infections. Yet, this has not been reported with this new virus. There are risk factors that seem to increase morbidity in pregnancy, such as obesity (body mass index [BMI] > 35), asthma and cardiovascular disease. Current reports describe an increased rate of pretermbirth and C-section. Vertical transmission
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 05-16-2019;41(3):176-182
The aim of the present study was to describe and analyze data of 57 women with borderline ovarian tumors (BOTs) regarding histological characteristics, clinical features and treatment management at the Department of Obstetrics and Gynecology of the Universidade Estadual de Campinas (Unicamp, in the Portuguese acronym).
The present retrospective study analyzed data obtained from clinical and histopathological reports of women with BOTs treated in a single cancer center between 2010 and 2018.
A total of 57 women were included, with a mean age of 48.42 years old (15.43- 80.77), of which 30 (52.63%) were postmenopausal, and 18 (31.58%) were < 40 years old. All of the women underwent surgery. A total of 37 women (64.91%) were submitted to complete surgical staging for BOT, and none (0/57) were submitted to pelvic or paraortic lymphadenectomy. Chemotherapy was administered for two patients who recurred. The final histological diagnoses were: serous in 20 (35.09%) cases, mucinous in 26 (45.61%), seromucinous in 10 (17.54%), and endometrioid in 1 (1.75%) case. Intraoperative analyses of frozen sections were obtained in 42 (73.68%) women, of which 28 (66.67%) matched with the final diagnosis. The mean follow-up was of 42.79 months (range: 2.03-104.87 months). Regard ingthe current status of the women, 45(78.95%) are alive without disease, 2(3.51%) arealive with disease, 9 (15.79%) had their last follow-up visit > 1 year beforethe performanceof the present study but arealive, and 1 patient(1.75%) died of another cause.
Women in the present study were treated according to the current guidelines and only two patients recurred.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 11-01-2018;40(11):713-721
Does the use of metformin have an influence on the outcomes of preeclampsia (PE)?
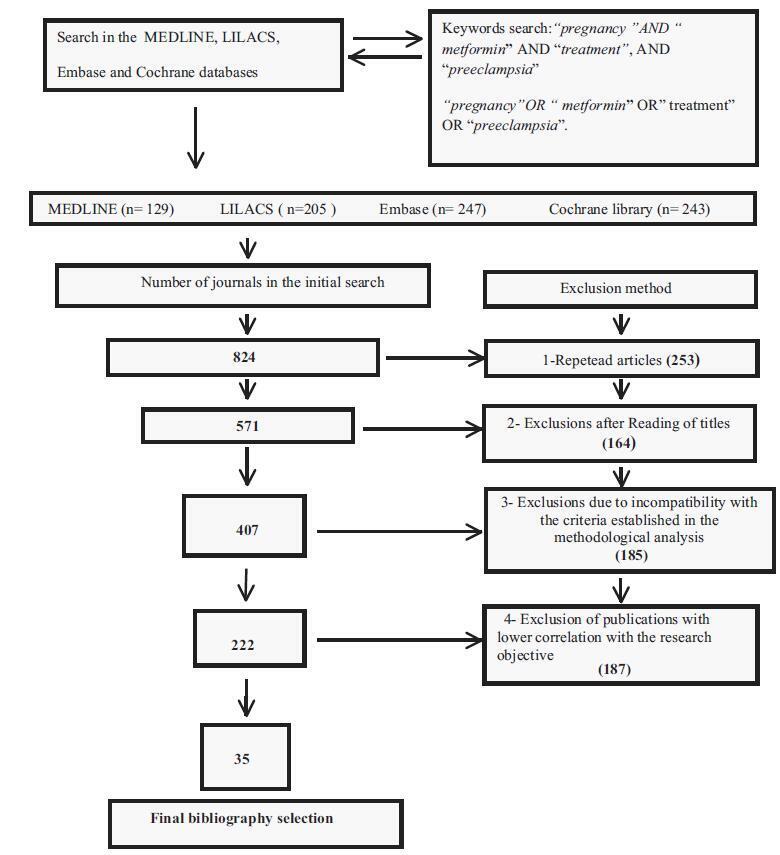
The descriptors pregnancy, metformin, treatment, and preeclampsia associated with the Boolean operators AND and OR were found in the MEDLINE, LILACS, Embase and Cochrane databases. A flowchart with exclusion criteria and inclusion strategy using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol, and eligibility criteria was used. Data were extracted regarding the type of study, the applied dosage, treatment time, segment, bias risks, and the Patient, Intervention, Comparison and Outcome (PICO) strategy to identify the quality of the study.
Total number of journals in the initial search (n= 824); exclusions from repeated articles on different search engines (n= 253); exclusions after reading the titles, when the title had no correlations with the proposed theme (n= 164); exclusions due to incompatibility with the criteria established in the methodological analysis (n= 185), exclusion of articles with lower correlation with the objective of the present study (n= 187); and final bibliographic selection (n= 35).
At first, a systematic review of the literature was performed. Subsequently, from the main selection, randomized and non-randomized trials with metformin that presented their results in absolute and relative numbers of PE outcomes were selected. The variables were treated statistically in the meta-analysis with the Review Manager software (RevMan), version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration. Denmark in the Hovedistaden region.
The study showed that metmorfin presented greater preventive effects for pregnancy-induced hypertension and was less effective for PE.
Metformin may gain place in preventive treatments for PE, once the dosages, the gestational age, and treatment time are particularly evaluated. A methodological strategy with an improved perspective of innovative and/or carefully progressive dosages during pregnancy to avoid side effects and the possibility of maternal-fetal risks is suggested.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 03-01-2018;40(3):147-155
Endometriosis can have several different presentations, including overt ascites and peritonitis; increased awareness can improve diagnostic accuracy and patient outcomes. We aimto provide a systematic review and report a case of endometriosis with this unusual clinical presentation. The PubMed/MEDLINE database was systematically reviewed until October 2016. Women with histologically-proven endometriosis presenting with clinically significant ascites and/or frozen abdomen and/or encapsulating peritonitis were included; thosewith potentially confounding conditionswere excluded.Our search yielded 37 articles describing 42 women, all of reproductive age. Ascites was mostly hemorrhagic, recurrent and not predicted by cancer antigen 125 (CA-125) levels. In turn, dysmenorrhea, dyspareunia and infertility were not consistently reported. The treatment choices and outcomes were different across the studies, and are described in detail. Endometriosis should be a differential diagnosis of massive hemorrhagic ascites in women of reproductive age.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 06-27-2002;24(3):201-204
DOI 10.1590/S0100-72032002000300009
Chronic placental abruption is a rare condition that can be early detected by ultrasound. Vaginal bleeding and uterine excitability can be present in an infrequent way. Chronic placental abruption physiopathology is unknown and there are no consistent medical risks that predispose to this condition. The perinatal outcome is poor and is often associated with prematurity and fetal or perinatal death. The obstetric treatment depends on the gestational age, fetal conditions and the size of the clot. We present a case of a chronic placental abruption diagnosed in a 14-week gestation complicated by intrauterine growth retardation, oligohydramnios and perinatal death.