-
Original Articles
Evaluation of Probably Benign Adnexal Masses in Postmenopausal Women
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):229-234
05-01-2017
Summary
Original ArticlesEvaluation of Probably Benign Adnexal Masses in Postmenopausal Women
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):229-234
05-01-2017Views79See moreAbstract
Background
Preoperatively identification of malignancy potential of a postmenopausal adnexal masses is important.
Aim
To evaluate the effectiveness of the Risk of Malignancy Index-2 in presumably benign adnexal masses in postmenopausal women.
Study Design
Retrospective, observational study.
Methods
119 women with postmenopausal adnexal masses with a preliminary diagnosis of benign tumors according to the Risk of Malignancy Index-2 were included. Age, duration of menopause, ultrasonographic findings, and serum CA-125 levels were recorded preoperatively. The definitive diagnosis was based on postoperative histopathological examination.
Results
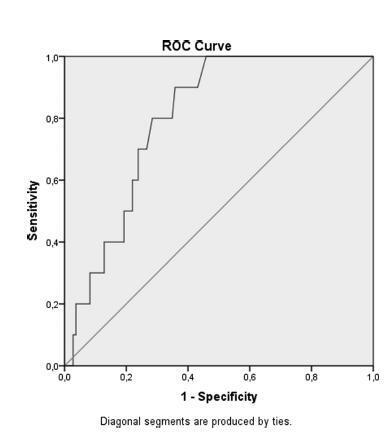
Of 119 adnexal mass, 10 were malignant and 109 were benign. There was no statistically significant difference with regard to age and tumor size between the groups. The two significant ultrasonographic parameter between groups were the presence of solid area in the mass and bilaterality. Moreover, if the cut off point for serum CA-125 was adjusted to 14.75 IU/mL according to ROC curve, a sensitivity value of 80% and a specificity value of 72% could be achieved to discriminate benign and malign cysts.
Conclusion
In the differential diagnosis of benign and malignant adnexal masses in postmenopausal women, the presence of a solid component, bilaterallity based on ultrasonography and high CA-125 values may be used as discriminative criteria. There is no direct relation between the size of the adnexal mass and malignancy potential. Therefore, in the malignancy indexes of postmenopausal women, we recommend lower cut-off values of CA-125 to increase the sensitivity of preoperative evaluation tests without having a great impact on negative predictive values.
-
Original Article
Sonographic Cervical Shortening after Labor Induction is a Predictor of Vaginal Delivery
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(12):585-588
12-01-2016
Summary
Original ArticleSonographic Cervical Shortening after Labor Induction is a Predictor of Vaginal Delivery
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(12):585-588
12-01-2016Views90See moreABSTRACT
Objective:
Analyzing if the sonographic evaluation of the cervix (cervical shortening) is a prognostic marker for vaginal delivery.
Methods:
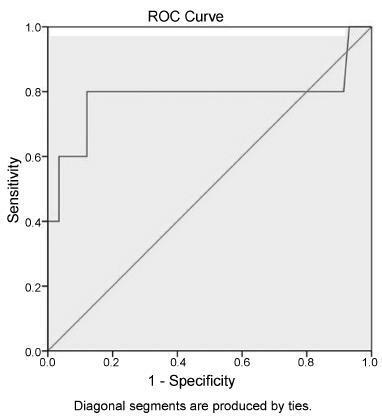
Women who underwent labor induction by using dinoprostone were enrolled. Before the induction and three hours after it, the cervical length was measured by ultrasonography to obtain the cervical shortening. The cervical shortening was introduced in logistic regression models among independent variables and for calculating receiver operating characteristic (ROC) curves.
Results:
Each centimeter in the cervical shortening increases the odds of vaginal delivery in 24.4% within 6 hours; in 16.1% within 24 hours; and in 10.5% within 48 hours. The best predictions for vaginal delivery are achieved for births within 6 and 24 hours, while the cervical shortening poorly predicts vaginal delivery within 48 hours.
Conclusion:
The greater the cervical shortening 3 hours after labor induction, the higher the likelihood of vaginal delivery within 6, 24 and 48 hours.
-
Original Article
Accuracy of Transvaginal Ultrasonography, Hysteroscopy and Uterine Curettage in Evaluating Endometrial Pathologies
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):506-511
10-01-2016
Summary
Original ArticleAccuracy of Transvaginal Ultrasonography, Hysteroscopy and Uterine Curettage in Evaluating Endometrial Pathologies
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):506-511
10-01-2016Views114Abstract
Objective
To evaluate the accuracy of transvaginal ultrasonography, hysteroscopy and uterine curettage in the diagnosis of endometrial polyp, submucous myoma and endometrial hyperplasia, using as gold standard the histopathological analysis of biopsy samples obtained during hysteroscopy or uterine curettage.
Methods
Cross-sectional study performed at the Hospital Universitário de Brasília (HUB). Data were obtained from the charts of patients submitted to hysteroscopy or uterine curettage in the period from July 2007 to July 2012.
Results
One-hundred and ninety-one patients were evaluated, 134 of whom underwent hysteroscopy, and 57, uterine curettage. Hysteroscopy revealed a diagnostic accuracy higher than 90% for all the diseases evaluated, while transvaginal ultrasonography showed an accuracy of 65.9% for polyps, 78.1% for myoma and 63.2% for endometrial hyperplasia. Within the 57 patients submitted to uterine curettage, there was an accuracy of 56% for polyps and 54.6% for endometrial hyperplasia.
Conclusion
Ideally, after initial investigation with transvaginal ultrasonography, guided biopsy of the lesion should be performed by hysteroscopy, whenever necessary, in order to improve the diagnostic accuracy and subsequent clinical management.
Key-words accuracyEndometrial hyperplasiaEndometrial polypHysteroscopysubmucous myomaTransvaginal ultrasonographyuterine curettageSee more -
Trabalhos Originais
Evaluation of Risk for Preterm Delivery by Fetal Fibronectin: Test and Measurement of Uterine Cervix
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(10):633-639
07-23-2000
Summary
Trabalhos OriginaisEvaluation of Risk for Preterm Delivery by Fetal Fibronectin: Test and Measurement of Uterine Cervix
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(10):633-639
07-23-2000DOI 10.1590/S0100-72032000001000006
Views106See morePurpose: to evaluate the risk of preterm delivery using the fetal fibronectin test and the measurement of the cervix by transvaginal ultrasonography in pregnant women with previous preterm delivery. Methods: one hundred and seven women were enrolled in the study at 24th, 28thand 32ndweek to detect the presence of fetal fibronectin by immediate-reading membrane test and to perform vaginal ultrasonography to measure the length of the cervix between the internal and external cervical os. The cervix was considered to be short when the cervical length was at or below the cutoff set by the receiver-operating characteristic (ROC) curve for prediction of preterm delivery. Sonographic cervical length and fetal fibronectin were compared to assess the risk of preterm birth before 34 and 37 weeks. Results: the spontaneous preterm delivery rate was 37.4% (40/107). The analysis made by the ROC curve indicated 30 mm as the best cutoff to maximize sensitivity and specificity at 24 and 28 weeks and 25 mm at 32 weeks of gestation. The positive test of fetal fibronectin had a significant relative risk (RR: 1.77; 95% confidence interval (IC): 1.10-2.84) to predict delivery before 37 weeks, when compared with a negative test, only at 28 weeks. The presence of short cervix at 24, 28 and 32 weeks showed a significative RR for birth before 37 weeks. The highest RR occurred with a short cervix at 24 weeks (RR: 4.42; 95% CI: 1.25-15.56). Conclusion: we concluded that the measurement of uterine cervix by vaginal ultrasonography is better than the fetal fibronectin test for evaluating the risk of preterm delivery in women with previous preterm delivery.
-
Trabalhos Originais
Changes in cervical length during pregnancy measured by transvaginal ultrasound
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(2):115-121
07-04-2003
Summary
Trabalhos OriginaisChanges in cervical length during pregnancy measured by transvaginal ultrasound
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(2):115-121
07-04-2003DOI 10.1590/S0100-72032003000200007
Views113See morePURPOSE: to establish a normality curve of cervical length during pregnancy measured by transvaginal ultrasonography. METHODS: we conducted a prospective, longitudinal study on 82 healthy pregnant women who were followed up from the beginning of pregnancy to delivery at four-week intervals, of whom 49 concluded the study. Patients were divided according to parity into nulliparous women and women with one or more previous deliveries. Cervical length was measured in a sagittal view by transvaginal ultrasonography, as the linear distance between internal and external cervical os. RESULTS: no significant difference was observed in mean cervical length or the 5th, 25, 50th, 75th, or 95th percentile according to gestational age between groups (p>0.05). Between the 20thand 24th gestacional week, the 5th, 50th and 95th percentiles of cervical length were 28, 35 and 47.2 mm, respectively. Cervical length decreased progressively during normal pregnancy, with a significant shortening observed after 20 weeks of gestation and being more marked after 28 weeks (p<0.05). CONCLUSION: the pattern of cervical length behavior does not seem to differ between nulliparous women and women with one or more previous deliveries. The numerical values of the normality curve of cervical length according to gestational age reflect the variability in the peculiar characteristics of the studied sample, thus emphasizing the value of the parameters established for different populations.


