Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):137-144
The present study aims to evaluate the profile of endometrial carcinomas and uterine sarcomas attended in a Brazilian cancer center in the period from 2001 to 2016 and to analyze the impact of time elapsed fromsymptoms to diagnoses or treatment in cancer stage and survival.
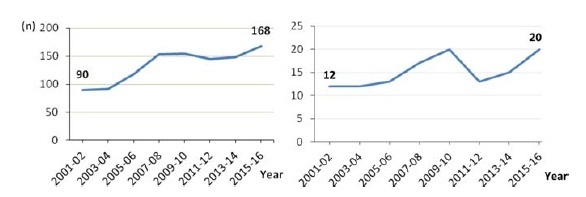
This observational study with 1,190 cases evaluated the year of diagnosis, age-group, cancer stage and histological type. A subgroup of 185 women with endometrioid histology attended in the period from 2012 to 2017 was selected to assess information about initial symptoms, diagnosticmethods, overall survival, and to evaluate the influence of the time elapsed from symptoms to diagnosis and treatment on staging and survival. The statistics used were descriptive, trend test, and the Kaplan- Meier method, with p-values < 0.05 for significance.
A total of 1,068 (89.7%) carcinomas (77.2% endometrioid and 22.8% nonendometrioid) and 122 (10.3%) sarcomas were analyzed, with an increasing trend in the period (p < 0.05). Histologies of non-endometrioid carcinomas, G3 endometrioid, and carcinosarcomas constituted 30% of the cases. Non-endometrioid carcinomas and sarcomas weremore frequently diagnosed in patients over 70 years of age and those on stage IV (p < 0.05). The endometrioid subgroup with 185 women reported 92% of abnormal uterine bleeding and 43% diagnosis after curettage. The average time elapsed between symptoms to diagnosis was 244 days, and between symptoms to treatment was 376 days, all without association with staging (p = 0.976) and survival (p = 0.160). Only 12% of the patients started treatment up to 60 days after diagnosis.
The number of uterine carcinoma and sarcoma cases increased over the period of 2001 to 2016. Aggressive histology comprised 30% of the patients and, for endometrioid carcinomas, the time elapsed between symptoms and diagnosis or treatment was long, although without association with staging or survival.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(10):467-472
DOI 10.1590/SO100-720320150005440
The administration of a single-course antenatal corticosteroid treatment is recommended for pregnant women between 24 and 34 weeks with risk of premature birth. The maximum effect is achieved when antenatal corticosteroids are administered between 24h and 7 days before delivery. The objective of this study was to evaluate the occurrence of birth within seven days of corticosteroid therapy in major obstetric situations with risk of preterm birth
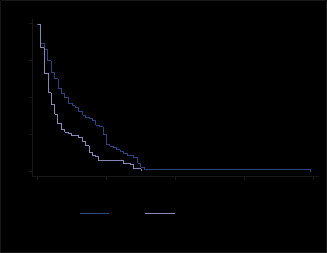
Retrospective cohort study including 209 pregnant women hospitalized in risk of preterm delivery, submitted to corticosteroid therapy for fetal lung maturation. The study was carried out between January 2012 and March 2014 at a university hospital. Main outcome measure was the number of women who delivered within 7 da ys after antenatal corticosteroid administration. Two groups were defined according to the reason for starting corticosteroids: threatened preterm labour (Group APPT) and other indications for corticosteroid therapy (Group RPPT). A Kaplan-Meier survival analysis was performed and a p value <0.05 was considered statistically significant.
46.4% (n=97) of pregnant women gave birth in the seven days following corticosteroid administration. Delivery within 7 days occurred more frequently on group 2 in comparison to group 1 (57.3 versus42.4%; p=0.001). There is a statistically significant difference between the survival curve for groups 1 and 2, with a hazard ratio for delivery within 7 days 1.71 times higher for group 2 (95%CI 1.23-2.37; p<0.001)
It can be concluded that the probability of an event (birth within 7 days after corticosteroids) is smaller in the group of pregnant women admitted in the context of threatened preterm labor than for other indications. The use of corticosteroids in pregnant women admitted for suspected preterm labor should be subject to rigorous clinical evaluation