Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(7):290-294
DOI 10.1590/S0100-72032013000700002
PURPOSE: To identify the predictive factors for voiding dysfunction after transobturator slings. METHODS: We retrospectively reviewed the records of all patients who underwent a transobturator sling between March 2003 and December 2008. A total of 514 women had available data with at least a six-week follow-up. Patients' demographics, preoperative symptoms, urodynamic testing including multichannel voiding studies and surgical variables were tabulated. Voiding dysfunction was defined by a catheterized or ultrasonographic postvoid residual greater than 100 cc (≥six weeks after the procedure) associated with any complaints of abnormal voiding. Univariate logistic regression analysis was performed with respect to postoperative voiding dysfunction. RESULTS: The patient population had a mean age of 58.5±12.9 years. Thirty-three out of 514 patients (6.4%) had postoperative voiding dysfunction according to our definition, and 4 (0.78%) required sling transection. No differences were observed between normal and dysfunctional voiders in age, associated prolapse surgery, preoperative postvoid residual, preoperative urinary flow rate, prior pelvic surgery, and menopausal status. Valsalva efforts during the preoperative pressure flow study was the only predictive factor for postoperative voiding dysfunction, 72.4% dysfunctional versus 27.6% normal (p<0.001). CONCLUSION: Preoperative Valsalva maneuver during the micturition could identify those at risk for voiding dysfunction after transobturator sling, and it should be noted during preoperative counseling.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(5):411-416
DOI 10.1590/S0100-72032004000500011
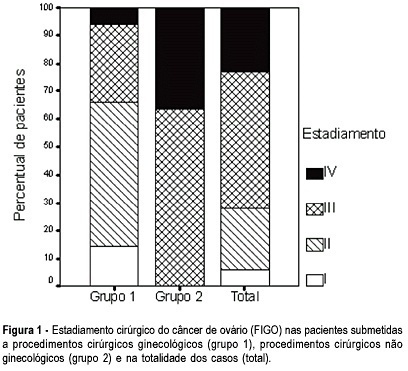
OBJECTIVE: to evaluate the incidence of non-gynecological surgical procedures used in the treatment of ovarian cancer, as well to describe their complications. METHODS: eighty-two patients with ages from 22 to 89 (mean = 54.1 ± 15.1 years), submitted to laparotomy for surgical treatment of ovarian cancer from February 1999 to October 2003 were retrospectively evaluated. This study included only patients with epithelial ovary carcinoma. The patients were divided into 2 groups, patients submitted exclusively to gynecological procedures and patients submitted to non-gynecological procedures. Statistical analysis was made with the Student's t-test or the chi-square test. RESULTS: 5 patients (6.1%) were in stage (FIGO) I, 18 (21.9%) in stage II, 40 (48.8%) in stage III, and 19 (23.2%) in stage IV. Non-gynecological procedures were done in 35 cases (42.7%), including: 17 colostomies, 16 enterectomies, 8 peritonectomies, 7 colectomies, 5 partial diaphragm resections, 4 partial cystectomies, 4 splenectomies, 2 ileostomies, and 1 hepatectomy. All patients submitted to non-gynecological procedures were included in stages III and IV. This group of patients underwent longer-lasting surgeries (5.3 ± 1.4 versus 3.1 + 0,0 h; p < 0.001). There was no significant difference between these two groups regarding hemotransfusion requirement (42,2 versus 40%; p = 0.512) and hospitalization time (11.5 ± 7.2 versus 10 ± 9.9 days; p = 0.454). Patients submitted to non-gynecological surgeries developed higher rates of postoperative complications (37 versus 17.1%; p = 0.042), and two of them (2.4%) died. CONCLUSION: non-gynecological surgical procedures are frequently used in the treatment of patients with ovarian cancer. These procedures are associated with a longer-lasting surgery and higher rates of postoperative complications.