-
Review Article02-18-2022
Burch Procedure: A Historical Perspective
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):511-518
Abstract
Review ArticleBurch Procedure: A Historical Perspective
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):511-518
Views153See moreAbstract
Introduction
The Burch procedure (1961) was considered the gold standard treatment for stress urinary incontinence (SUI) before the midurethral slings (MUSs) were introduced, in 2001.
Objective
This historical perspective of the Burch’s timeline can encourage urogynecological surgeons to master the Burch technique as one of the options for surgical treatment of SUI.
Search Strategy and Selection
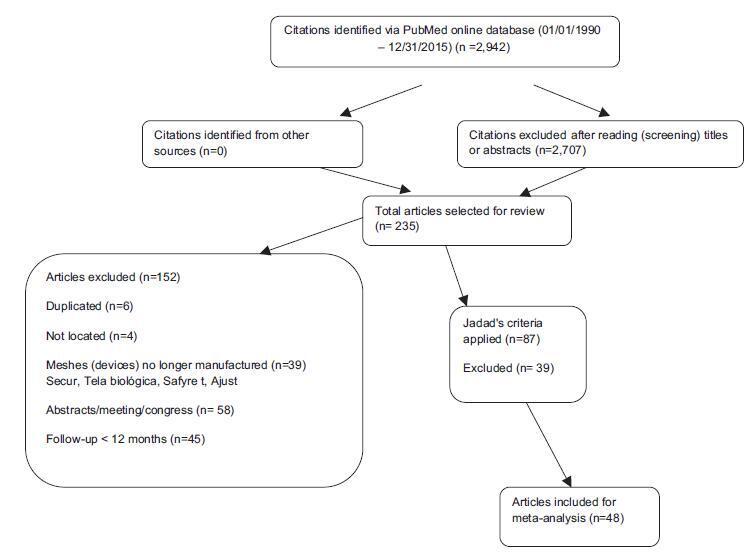
Criteria A bibliographic search was performed in the PubMed and National Library of Medicine (NIH) databases with the terms Burch colposuspension AND history AND stress urinary incontinence in the last 20 years. The original article by Burch (1961) was included. The references were read by three authors. The exclusion criterion was studies in non-English languages. Biomedical Library Special Collections were included as historical relevant search.
Data Collection, Analysis and Main Results
Some modifications of the technique have been made since the Burch procedure was first described. The interest in this technique has been increasing due to the negative publicity associated with vaginal synthetic mesh products. Twenty-nine relevant articles were included in the present review article, and numerous trials have compared Burch colposuspension with MUS.
Conclusion
This historical perspective enables the scientific community to review a standardized technique for SUI. Burch colposuspension should be considered an appropriate surgical treatment for women with SUI, and an option in urogynecological training programs worldwide.
-
Original Article01-19-2021
Effect of Preoperative Urodynamic Study on Urinary Outcomes after Transobturator Sling
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):131-136
Abstract
Original ArticleEffect of Preoperative Urodynamic Study on Urinary Outcomes after Transobturator Sling
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):131-136
Views105Abstract
Objective
To evaluate whether performing preoperative urodynamic study influences postoperative urinary symptoms of women with stress urinary incontinence that underwent transobturator sling.
Methods
Retrospective analysis of patients treated for stress urinary incontinence by transobturator sling from August 2011 to October 2018. Predictor variables included preoperative urodynamic study, age, incontinence severity, body mass index, preoperative storage symptoms and previous anti-urinary incontinence procedure. Outcome variables were postoperative subjective continence status, storage symptoms and complications. Logistic regression after propensity score was employed to compare outcomes between patients who underwent or not pre-operative urodynamic study.
Results
The present study included 88 patients with an average follow-up of 269 days. Most patients (n = 52; 59.1%) described storage symptoms other than stress urinary incontinence, and 38 patients (43.2%) underwent preoperative urodynamic studies. Logistic regression after propensity score did not reveal an association between urinary continence outcomes and performance of preoperative urodynamic study (odds ratio 0.57; confidence interval [CI]: 0.11-2.49). Among women that did not undergo urodynamic study, there was a subjective improvement in urinary incontinence in 92% of the cases versus 87% in those that underwent urodynamic study (p = 0.461). Furthermore, postoperative storage symptoms were similar between women who did not undergo urodynamic study and those who underwent urodynamic study, 13.2% versus 18.4%, respectively (p = 0.753).
Conclusion
Preoperative urodynamic study had no impact on urinary incontinence cure outcomes as well as on urinary storage symptoms after the transobturator sling in women with stress urinary incontinence.
Key-words propensity scoreStress urinary incontinencetransobturator suburethral tapeUrinary incontinenceurodynamicSee more -
Original Article10-01-2018
Five-year Follow-up of Transobturator Sling: 152 Cases with the Same Surgeon
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):614-619
Abstract
Original ArticleFive-year Follow-up of Transobturator Sling: 152 Cases with the Same Surgeon
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):614-619
Views164See moreAbstract
Objective
To evaluate the long-term subjective cure rate of the transobturator sling, including an analysis of the risk factors and of the impact of increased surgical experience on the results.
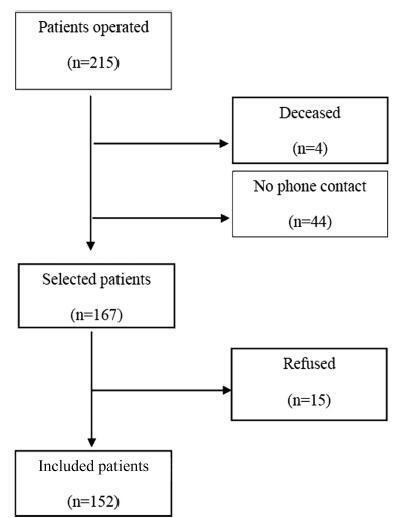
Methods
A retrospective cohort study of women who underwent transobturator sling surgery from 2005 to 2011 was conducted. Patients were evaluated by a telephone survey using the International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF) and by subjective questions regarding satisfaction. An ICIQ-SF score of 0 was considered a cure. The crude and adjusted odds ratios and 95% confidence intervals were estimated in univariate and multivariate logistic regression models to identify risk factors for surgical failure. Differences with p < 0.05 were considered significant.
Results
In total, 152 (70.6%) patients answered the questionnaire. The median follow-up period was 87 months. The urodynamic diagnosis was stress urinary incontinence in 144 patients (94.7%), and mixed urinary incontinence in 8 (5.3%) patients. Complications occurred in 25 (16%) patients. The ICQ-SF results indicated that 99 (65.10%) patients could be considered cured (ICIQ-SF score = 0). Regarding the degree of satisfaction, 101 (66%) considered themselves cured, 43 (28%) considered themselves improved, 7 (4.6%) considered themselves unchanged, and one reported worsening of the incontinence. After the univariate and multivariate analyses, the primary risk factor for surgical failure was the presence of urgency (p < 0.001).
Conclusion
The transobturator sling is effective, with a low rate of complications and a high long-term satisfaction rate. The risk factors for failure were the presence of urgency and patient age. The increased experience of the surgeon was not a factor that influenced the rate of complications.
-
Original Article01-17-2010
Body mass index influence in female urinary incontinence
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(9):454-458
Abstract
Original ArticleBody mass index influence in female urinary incontinence
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(9):454-458
DOI 10.1590/S0100-72032010000900007
Views69See morePURPOSE: to evaluate and compare the effects of body mass index (BMI) on the severity of female urinary incontinence (UI) using the quality of life questionnaire King's Health Questionnaire (KHQ), variables of urodynamic studies and the medical history taken. METHODS: cross-sectional clinical study. We selected 65 patients with stress urinary incontinence (SUI) who were divided into three groups: Group I (BMI: 18-25 kg/m²), Group II (BMI: 25-30 kg/m²) and Group III (BMI>30 kg/m²). The KHQ domains were compared between these groups. In addition, some clinical history urodynamic data (presence of nocturia, enuresis, urgency and urge incontinence) were also related to BMI by calculating the Odds Ratio (OR). The BMI in the presence and absence of non-inhibited detrusor contractions and Valsalva leak point pressure (VLPP) <60 or > 60 cmH2O were evaluated. Finally, the correlation between BMI and the nine KHQ domains has been tested in order to detect some association. RESULTS: the KHQ did not record deterioration of quality of life in women with UI with increasing BMI in any of its areas. The OR for the presence of enuresis in relation to a BMI was 1.003 [CI: 0.897-1.121], p=0.962. The OR for nocturia was 1.049 [CI: 0.933-1.18], p=.425. The OR for urgency was 0.975 [CI: 0.826-1.151], p=0.762, and the OR for incontinence was 0.978 [CI: 0.85-1.126], p=0.76. We studied the BMI in patients with and without non-inhibited detrusor contractions and detected medians of 26.4±4.8 and 28.3±5.7 kg/m², respectively (p=0.6). Similarly, the median BMI values for the groups with VLPP <60 and >60 cmH2O were 29.6±4.1 and 27.7±5.7 kg/m², respectively (p=0.2). Finally, we failed to demonstrate an association between BMI and any of the nine KHQ domains by means of the Spearman correlation. CONCLUSION: there was no association of KHQ scores with BMI. There was also no correlation between the parameters of clinical history and of the urodynamic study with BMI.
-
Original Article10-17-2000
Comparison of the results of the treatment of stress urinary incontinence with three different surgical procedures
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(1):43-48
Abstract
Original ArticleComparison of the results of the treatment of stress urinary incontinence with three different surgical procedures
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(1):43-48
DOI 10.1590/S0100-72032000000100008
Views120See morePurpose: to analyze the prevalence of genuine urinary incontinence (GUI) recurrence, after at least two years of follow-up, in different surgical techniques used for its correction. Patients and Methods: fifty-five patients with diagnosis of GUI, submitted to surgery for its repair at the Serviço de Ginecologia e Obstetrícia do Hospital de Clínicas de Porto Alegre from 1992 to 1996 and whose post-surgical follow-up was superior to 2 years were divided into three groups according to the surgical approach: Kelly-Kennedy (n = 24), Burch (n = 23) and Marshall-Marchetti-Krantz (n = 8). Results: there were no differences regarding recurrence rate, age at surgery and at recurrence time, estrogen therapy, number of pregnancies and vaginal delivery (p>0.05). Although posterior perineoplasty was more prevalent in the Kelly-Kennedy group, it did not influence the recurrence rate. The group submitted to the Burch approach had more years of menopause at the time of surgery. Conclusion: the recurrence rates of urinary incontinence comparing the three different techniques (Kelly-Kennedy, Burch and Marshall-Marchetti-Krantz) were, respectively, 29.2, 39.1 and 50%, which did not differ statistically. Considering the potential confusional bias for urinary stress incontinence, they did not differ among the groups. Nevertheless, we noticed that all women who had previous surgery presented recurrence of incontinence.
-
Original Article07-05-2005
Is there any difference between female pelvic floor muscle contractility in different positions?
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(1):12-19
Abstract
Original ArticleIs there any difference between female pelvic floor muscle contractility in different positions?
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(1):12-19
DOI 10.1590/S0100-72032005000100005
Views114See morePURPOSE: to evaluate and compare results of female pelvic floor surface electromyography in different positions: lying, sitting and standing. METHODS: twenty-six women with the diagnosis of stress urinary incontinence treated with a protocol of exercises to strengthen the pelvic floor muscle were evaluated. Pelvic floor surface electromyography was performed with an intravaginal sensor connected to Myotrac 3G TM equipment, as follows: initial rest of 60 s, five phasic contractions, one 10-s tonic contraction and one 20-s tonic contraction. The amplitudes were obtained from the difference between the final contraction amplitude and the amplitude at rest (in µV). Wilcoxon test was applied for nonparametric data (p value <0.05). RESULTS: the amplitudes of contractions were higher in the lying position, decreasing in the sitting and standing positions. In the lying position, the median values of phasic and tonic contractions were 23.5 (5-73), 18.0 (3-58) and 17.0 (2-48), respectively. In the sitting position, they were 20.0 (2-69), 16.0 (0-58) and 15.5 (1-48). In the standing position they were 16.5 (3-67), 12.5 (2-54) and 13.5 (2-41). All amplitude values were significantly lower in the standing position compared to the lying position (p<0.001, p<0.001 and p=0.003). Similar results were also found in comparison to the sitting position. However, there was no significant difference between the lying and the sitting positions. CONCLUSION: all female pelvic floor contraction amplitudes were lower in the standing position, suggesting that the muscle strength should be intensified in that position.