-
Original Article
Trends Associated with Stillbirth in a Maternity Hospital School in the North Zone of São Paulo: A Cross-Sectional Study
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(10):597-606
11-07-2019
Summary
Original ArticleTrends Associated with Stillbirth in a Maternity Hospital School in the North Zone of São Paulo: A Cross-Sectional Study
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(10):597-606
11-07-2019Views133See moreAbstract
Objective
To evaluate conditions associated with stillbirth (SB), and possible trends related with it, in a maternity hospital school in the North zone of São Paulo.
Methods
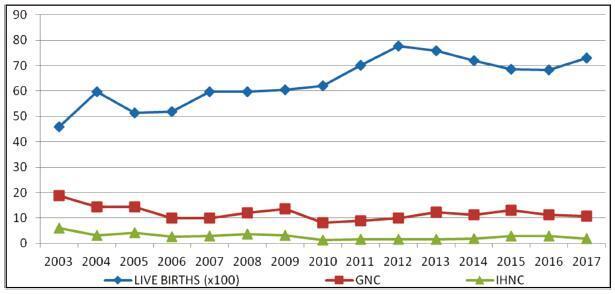
An observational, cross-sectional study conducted at the Hospital Maternidade- escola de Vila Nova Cachoeirinha with 1,139 SBs in the period of 2003 to 2017. Cases of intermediate SB (ISB) (weight between 500 and 999 g) and late SB (LSB) (weight ≥ 1,000 g) were compared. We evaluated clinical data, laboratory tests, and fetal and placental studies. Data were stored in Windows Excel (Microsoft Corp., Redmond, WA, USA) worksheets, according to which graphs and tables were constructed. We used the statistical software SPSS for Windows version 18.0 (SPSS In., Chicago, IL, USA), estimating the prevalence ratio (PR) and odds ratio (OR), considering the 95% confidence interval (95% CI).
Results
The general SB rate was 11.9%, and the in-hospital SB rate was 2.8%. Pregnant women younger than 16 years of age were more likely to have ISB (OR 0.32, 0.15- 0.76), while patients older than 40 years old had a higher chance of LSB (PR 0.85, 0.72- 0.99). A total of 25.7% of the general population did not have prenatal care, and 77.1% of the cases presented fetal death at admission. The cases of ISB had a statistically significant association with home birth (OR 0.61, 0.46-0.80). Cesarean section was performed in 16.1% of the subjects, and misoprostol was the most used method for induction. Necropsy and placental study of the fetuses were performed, respectively, in 94.2% and 97.3% of the cases. Associated causes were not identified in 22.1% of the cases, and the main causes identified were amniotic sac infections (27.9%), fetal malformations (12.5%), placental abruption (11.2%), hypertensive syndromes (8.5%), and maternal syphilis (3.9%), the latter with an increasing trend.
Conclusion
Among the factors associated to SB were: hypertensive syndromes, amniotic sac infections, fetal malformations, placental abruption and syphilis. There was a growing trend in the number of cases of syphilis, which translates an alert. Diagnostic limitations justify indeterminate causes.
-
Artigos Originais
Difficulties for identification of cause of fetal death: how to solve?
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(9):403-408
11-26-2012
Summary
Artigos OriginaisDifficulties for identification of cause of fetal death: how to solve?
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(9):403-408
11-26-2012DOI 10.1590/S0100-72032012000900003
Views56See morePURPOSE: To identify the causes of fetal death in the studied population and to measure their contribution in identifying the cause of this outcome. To propose the use of the system Relevant Condition of Death (ReCoDe) in elucidating the causes of fetal death to minimize the number of unknown causes. METHODS: Cross-sectional study related to fetal deaths seen at a specialized academic hospital in the South of Brazil, from January 2000 to December 2009. The data were collected in the death certificates, maternal medical records and the reports of study of fetuses and attachments, and the findings were compared. Data analysis was performed using SPSS version 17.0. RESULTS: Were included 111 fetuses and their respective mothers in this study. The comparison between the diagnostic causes in the pathology and clinical evaluation showed 74 (66.7%) and 73 (65.8%), respectively. Together, they found a potential cause in 48.7% of cases, while 16.2% remained unknown. When analyzing both together with the ReCoDe system, only 9.9% of stillbirths remained as "unclassified." CONCLUSIONS: The proportion of diagnoses in the cause of death among the pathological and clinical evaluation showed no significant difference. When comparing the results of the cause of death suggested by the clinic/pathology with the use of the ReCoDe system, it appears that this tool has helped to clarify the cause by reducing the amount of those that remained without a possible etiology.
-
Artigos Originais
Pregnancies complicated by maternal syphilis and fetal death
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(2):56-62
03-15-2012
Summary
Artigos OriginaisPregnancies complicated by maternal syphilis and fetal death
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(2):56-62
03-15-2012DOI 10.1590/S0100-72032012000200003
Views74PURPOSE: To describe the characteristics of pregnancies complicated by maternal syphilis and fetal death. METHODS: Retrospective descriptive study performed by reviewing the medical records of 48 pregnant women with maternal syphilis and fetal death outcome admitted to Hospital Geral de Nova Iguaçu, Baixada Fluminense, State of Rio de Janeiro, during the period from 2005 to 2008. Birth weight >500 g and fetal death documented by Death Certificate were the inclusion criteria. The following aspects were analyzed: sociodemographic factors, reproductive history, aspects of the current pregnancy, prenatal care, Venereal Disease Research Laboratory (VDRL) testing, and other gestational conditions, in addition to syphilis. The fetal deaths were classified as maternal, placental or fetal. Percentage, mean, standard deviation (SD), maximum and minimum values were reported. RESULTS: The mean maternal age was 22.7 years (SD=0.9 years), and at least 50% of the patients had low educational level. At hospital admission, 68.8% of the subjects were in the third trimester, with a mean gestational age of 29.2 weeks (SD=0.5), and more than 50% were in labor. The vast majority of fetal deaths (93%) occurred before maternal hospitalization. Among the patients who received prenatal care (54.2%), 30.8% had no VDRL test, 30.8 and 15.4% had a reactive and non-reactive result, respectively, and none had more than one prenatal VDRL test. At the time of childbirth, most of the mothers (95.8%) carried out VDRL testing. Overall, the VDRL titers varied from 1:1 to 1:512, with predominant values >1:4 (91.7%). In 23% of cases other clinical conditions related to fetal death, in addition to syphilis, were found. CONCLUSIONS: The infection was the main clinically identified cause of fetal death in this patient series. Fetal death occurred during the preterm period and in the presence of high titers of maternal infection, suggesting recent syphilis infection.
Key-words Fetal deathPregnancy complications, infectionsPregnancy, high riskPrenatal careStillbirthSyphilis, congenitalSee more -
Artigos Originais
Cesarean section in fetal death
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(4):169-175
07-02-2010
Summary
Artigos OriginaisCesarean section in fetal death
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(4):169-175
07-02-2010DOI 10.1590/S0100-72032010000400004
Views68See morePURPOSE: to determine the factors associated with cesarean section in pregnancies with fetal death at a maternity hospital in Recife, Pernambuco, Brazil. METHODS: a cross-sectional study was performed, which analyzed data from the information system about mortality and medical records, from January 2005 to December 2008, of Hospital Barão de Lucena (HBL). We analyzed women with fetal death diagnosis, with gestational age of 20 weeks or more, in terms of sociodemographic characteristics, causes and types of fetal death, obstetrical precedents and birth characteristics. The associations between the variables were analyzed by the χ2 test of association and Fisher exact test, with the level of significance set at 5%. We calculated the prevalence ratio as the measure of risk and the confidence interval (CI) at 95%. Logistic regression analysis was also performed and the Odds Ratio (OR) was calculated. RESULTS: among the 258 pregnant women with fetal death, 27.5% (n=71) underwent cesarean section. After multivariate analysis, the factors that remained significantly associated with cesarean section were maternal age below 20 years (OR=0.23; 95%CI=0.06-0.85), history of one or more cesarean sections (OR=7.02; 95%CI=2.29-21.55), multiple gestation (OR=9.06; 95%CI=2.01-40.71), use of misoprostol for birth induction (OR=0.07; 95%CI=0.01-0.32), fetal death occurring during birth (OR=4.01; 95%CI=1.13-14.24), low birth weight (OR=0.33; 95%CI=0.11-0.94), presence of hypertensive disorders (OR=3.7; 95%CI=1.46-9.39) and abruptio placentae (OR=13.9; 95%CI=4.67-41.69). CONCLUSION: in HBL, the risk factors for cesarean section in pregnancies with fetal death were previous cesarean section, multiple gestation, intrapartum deaths, hypertensive disorders and abruptio placentae. The protective factors were teenage pregnancy, use of misoprostol and low birth weight.
-
Trabalhos Originais
Epidemiology of fetal death in a low income population
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(2):71-75
04-16-1998
Summary
Trabalhos OriginaisEpidemiology of fetal death in a low income population
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(2):71-75
04-16-1998DOI 10.1590/S0100-72031998000200003
Views46See moreFetal death may not be considered an unusual event and, in developing countries, the most prevalent causes could be possibly controlled and/or treated. The purpose of the present study was to investigate causes of fetal death in a Brazilian population. This is a descriptive study performed at the Hospital Maternidade Leonor Mendes de Barros in São Paulo. The study subjects were 122 pregnant women with diagnosis of fetal death and gestation age of 20 or more weeks. The statistical procedures used were means and standard deviation. The main causes of the fetal death were hypertensive disorders and infections and, for a quarter of the cases, they were not identified at all. It is concluded that an important percentage of fetal deaths would have been prevented and that there was a significant number of unidentified causes. Results of the present study might be useful to orientate a primary prevention health program, specially concerning antenatal care.
-
Trabalhos Originais
Risk Factors for Stillbirth at a Universitary Hospital in Southern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(9):617-622
02-13-2002
Summary
Trabalhos OriginaisRisk Factors for Stillbirth at a Universitary Hospital in Southern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(9):617-622
02-13-2002DOI 10.1590/S0100-72032002000900008
Views46See morePurpose: to study the influence of the prenatal care, fetal and maternal factors on the stillbirth rates of a university hospital from the south of Brazil. Methods :a case-control study of the cases of stillbirth occurred before the beginning of labor, from March 1998 to June 2001, at the Hospital Geral of Caxias do Sul University. The controls were selected among live newborns. The analysis of the quality of the prenatal care was based on the criteria established by the Programa de Humanização do Pré-natal e Nascimento of the Brazilian Health Ministry (2000). To evaluate possible risk factors for stillbirth we used the odds ratio (OR). Other confounding factors were evaluated by logistic regression. Results: preterm delivery was more prevalent in the cases of stillbirth (31.7+4.7 vs 38.6+0.9). The average birth weight among the stillborns was 1,705 g (+837 g), while in the controls it was 3,080 g (+576 g). Prenatal care was observed in 81.5% of the stillbirths and in 91.6% of the control group. The initial analysis showed that three factors were associated with stillbirth: inadequate prenatal care (43.6 vs 23.4%), history of previous stillbirth (6.6 vs 0.9%) and maternal age (27+7.9 years vs 24+6.4 years). Nevertheless, after adjustment of these variables through logistic regression, only the maternal age maintained its association with the stillbirth rates. Conclusions: in the present study, the strongest factor associated with the occurrence of stillbirth was the increase in maternal age.


