-
Original Article
Applicability, Safety, and Efficiency of Salpingectomy versus Electrocoagulation and Laparoscopic Tubal Section in Ambulatory
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):866-870
08-29-2022
Summary
Original ArticleApplicability, Safety, and Efficiency of Salpingectomy versus Electrocoagulation and Laparoscopic Tubal Section in Ambulatory
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):866-870
08-29-2022Views115See moreAbstract
Objective
Female sterilization is a surgical procedure that aims women to permanently stop the use of conception. The benefits, risks and cost-effectiveness are important issues. The purpose of this study was comparing the applicability, complications and efficacy of salpingectomy versus electrocoagulation and tubal occlusion by laparoscopy in the Ambulatory Surgery Unit.
Methods
We performed a retrospective and observational study that included women undergoing laparoscopic sterilization procedures at our Ambulatory Surgery Unit, during three years. Statistical analysis was performed using SPSS, applying the Fisher exact test, the Mann-Whitney test, and Linear Regression.
Results
Two hundred and twenty-one laparoscopic surgical procedures were performed, including 79 (35.7%) bilateral total salpingectomies and 142 (64.3%) electrocoagulation and bilateral tubal occlusion procedures. The majority of the procedures were performed by a resident (n = 162; 73.3%), with 40% (n = 33) of salpingectomies. The surgical time, independently the type of surgeon, was significantly shorter in the tubal occlusion (42.2 vs. 52.7 min, p < 0.001). Safety and efficacy endpoints were not significantly different between the two groups, with a case of pregnancy in tubal occlusion group.
Conclusion
Salpingectomy is a safe and effective alternative comparing with electrocoagulation and tubal occlusion.
-
Original Article
The Use of Long Acting Reversible Contraceptives and the Relationship between Discontinuation Rates due to Menopause and to Female and Male Sterilizations
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(5):210-217
05-01-2016
Summary
Original ArticleThe Use of Long Acting Reversible Contraceptives and the Relationship between Discontinuation Rates due to Menopause and to Female and Male Sterilizations
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(5):210-217
05-01-2016Views165See moreAbstract
Introduction
Women require effective contraception until they reach menopause. The long acting reversible contraceptives (LARC) and the depot-medroxyprogesterone acetate (DMPA, Depo-Provera(r), Pfizer, Puurs, Belgium) are great options and can replace possible sterilizations.
Purpose
To assess the relationship between the use of LARCs and DMPA and terminations ascribed to menopause and sterilizations in a Brazilian clinic.
Methods
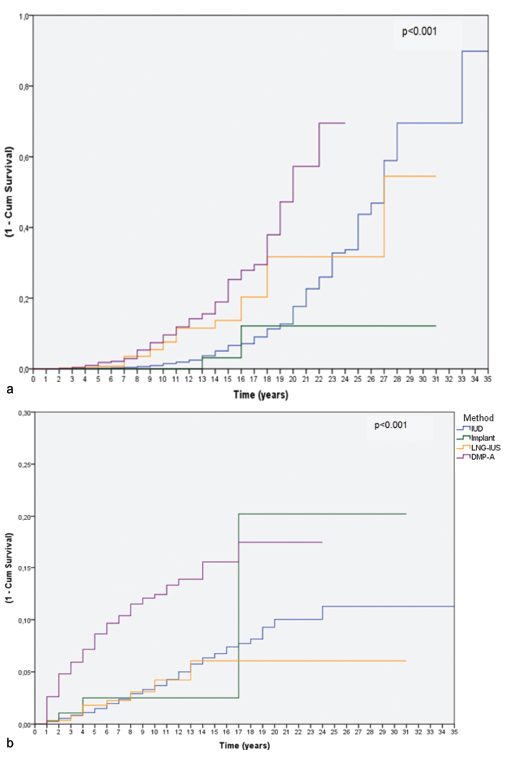
We reviewed the records of women between 12 and 50 years of age attending the clinic that chose to use a LARC method or DMPA. Cumulative termination rates due to sterilization or because the woman had reached menopause were computed using single decrement life-table analysis over 32 years. We also examined all records of surgical sterilization at our hospital between the years 1980-2012.
Results
Three hundred thirty-two women had continuously used the same contraceptive until menopause, and 555 women had discontinued the method because they or their partners underwent sterilization. From year 20 to year 30 of use, levonorgestrel intrauterine-releasing system (LNG-IUS - Mirena(r), Bayer Oy, Turku, Finland; available since 1980), copper intrauterine device (IUD - available since 1980) and DMPA users showed a trend of cumulative higher discontinuation rates due to menopause when compared with the discontinuation rates due to sterilization. Over the study period, a steep decline in the use of sterilization occurred.
Conclusion
Over the past 15 years of research we have observed a trend: women usually preferred to continue using LARC methods or DMPA until menopause rather than decide for sterilization, be it their own, or their partners'. The annual number of sterilizations dropped in the same period. The use of LARC methods and DMPA until menopause is an important option to avoid sterilization, which requires a surgical procedure with potential complications.
-
Artigos Originais
Wishes, intention and behavior in reproductive health: the practice of cesarean section in a city in the northeast of Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(7):388-396
12-06-2006
Summary
Artigos OriginaisWishes, intention and behavior in reproductive health: the practice of cesarean section in a city in the northeast of Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(7):388-396
12-06-2006DOI 10.1590/S0100-72032006000700003
Views81PURPOSE: to generate knowledge in order to allow of the determination the factors affecting the high incidence of caesarean section and its relation to sterilization. METHODS: the multicentric study on reproductive health in Brazil, carried out from 1998 to 2000, included the States of Rio Grande do Norte, Minas Gerais, São Paulo, and Rio Grande do Sul. It was characterized as a longitudinal study, where the women, proceeding from public as well as private health services, were interviewed at three moments: at the beginning of pregnancy (until the 22nd week of gestation), at the end of pregnancy (between 30 and 40 days before the probable date of childbirth) and after delivery (between 15 and 45 days after childbirth). The interviewed women complied with the following eligibility criteria: to have 18 to 40 years of age, to live in Natal and plan to deliver the baby in Natal. At the first moment, 433 women were interviewed, 380 at the second moment and 269 at the third moment. The data were submitted to the chi-square test, with the level of significance set at 0.05, just to assure the relation between the variable years of schooling (0 to 8 and 9 or +) and the representative variables for reproductive health. RESULTS: the result disclosed a statistically significant relationship (p<0.05) between the variables: years of schooling, parity, type of service used, social class, job status, and prenatal consultations. It was found that a higher educational level is predominant among those women who searched for private services, coming from higher social classes and large number of prenatal visits. Although without statistical significance, having a for the women coming from this type of service, a higher number of caesarean section5 was observed, probably due to an easy doctor-patient interaction, while the planned caesarean section was frustrated for 43% of those women coming from public health services, as well as the wish to have a tubal ligation at childbirth (57%). CONCLUSIONS: These results show up the great differentials between the private and public services, with a clear favoritism for the private sector, demonstrating clearly that the practical obstetrics in Brazil needs a change and an improvement both for those women with access to the private service, who obtain the accomplishment of the caesarean section without consistent medical indications, and those with access to the public service, who face difficulties in accomplishing this procedure, even with consistent medical indications, in order to provide equality in the reproductive rights of those women.
Key-words Caesarean sectionContraceptionIncidenceMulticenter studiesReproductive medicineSterilizationSee more


